
by Anthi Stefatos, MD; Julie N. Ha, PharmD; Adrian Baranchuk MD; Ross J. Baldessarini, MD; and Gustavo H. Vázquez MD, PhD
Drs. Stefatos and Ha are with the Department of Psychiatry at Queens University in Kingston, Ontario, Canada. Dr. Baranchuk is with the Department of Medicine at Queens University in Kingston, Ontario, Canada. Dr. Baldessarini is with the Department of Psychiatry at Harvard Medical School in Boston, Massachusetts, and the International Consortium for Mood & Psychotic Disorder Research at McLean Hospital in Belmont, Massachusetts. Dr. Vázquez is with the Department of Psychiatry at Queens University in Kingston, Ontario, Canada, and the International Consortium for Mood & Psychotic Disorder Research at McLean Hospital in Belmont, Massachusetts.
Funding: This study was supported by a grant from the Bruce J. Anderson Foundation and by the McLean Private Donors Research Fund (given to to RJB). The funding source had no role in study design; the collection, analysis and interpretation of data; the writing of the report; or the decision to submit the paper for publication.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Innov Clin Neurosci. 2018;15(5–6):43–45
Abstract: Background: Aripiprazole is a widely clinically employed antipsychotic drug for a range of indications. It has unusual pharmacodynamics as a dopamine D2 receptor partial-agonist with complex interactions with serotonin receptors and, a relatively unusual long elimination half-life. Although other atypical antipsychotics have been associated with an increased risk of atrial fibrillation, aripiprazole is considered to be relatively neutral in regard to its cardiac risk. We report a case of a 45-year-old Caucasian patient with schizoaffective disorder who developed acute atrial fibrillation (AF) several days after an intramuscular injection of a large long-acting dose of the drug after low oral doses had been well-tolerated. The patient responded to intravenous metoprolol and amiodarone and converted back to normal sinus rhythm within 24 hours, after having his oral aripiprazole dose lowered. The timing and dose-dependent effect of aripiprazole administration suggests an association between aripiprazole and the new onset of AF in this case, which calls for added clinical vigilance in patients with risk factors for stroke and in younger patients who could have predisposing factors for arrhythmias.
Aripiprazole is a second-generation antipsychotic drug indicated for a range of psychiatric conditions. It has unusual pharmacodynamics as a dopamine D2 receptor partial-agonist with complex interactions with serotonin receptors and a longer elimination half-life than other antipsychotics. We report a case of a patient who presented with an episode of acute atrial fibrillation (AF) several days after an injection of long-acting aripiprazole.
Case Presentation
A 45-year-old Caucasian man with a history of bipolar-type schizoaffective disorder was brought to the emergency department by police after making homicidal threats. He had been nonadherent to a regimen of lurasidone prescribed at 40mg/day orally due to perceived adverse sexual effects. He had no relevant medical history and denied taking any other prescriptions or over-the-counter medicines. Initially, he appeared acutely intoxicated, and admitted to having recently drunk approximately 355mL of whiskey.
On intake, his vital signs were stable: his pulse was 98 beats/minute, blood pressure was 144/82mmHg, respiratory rate was 20 beats/minute, and oral temperature was 36.5°C (97.7°F). An initial electrocardiogram (ECG) depicted normal sinus rhythm (Figure 1A), which was consistent with previous ECGs on record. The results of complete blood count and serum concentrations of electrolytes, creatinine, and liver function tests were all unremarkable. The patient was admitted to an inpatient general psychiatric unit. He was agitated and aggressive toward staff, requiring oral sedation with two separate doses of loxapine (50mg) and lorazepam (2mg) in the initial 48 hours. Two days after admission, he was started on a regular antipsychotic regimen of oral aripiprazole at 5mg in the morning and 10mg in the evening. Because of his history of medication nonadherence, he was offered long-acting aripiprazole by intramuscular depot injection, which he accepted. After eight days of treatment with oral aripiprazole at 15mg daily, he was given an intramuscular injection of 400mg of long-acting aripiprazole and continued on oral aripiprazole 15mg daily for 14 days, as recommended by the manufacturer.1
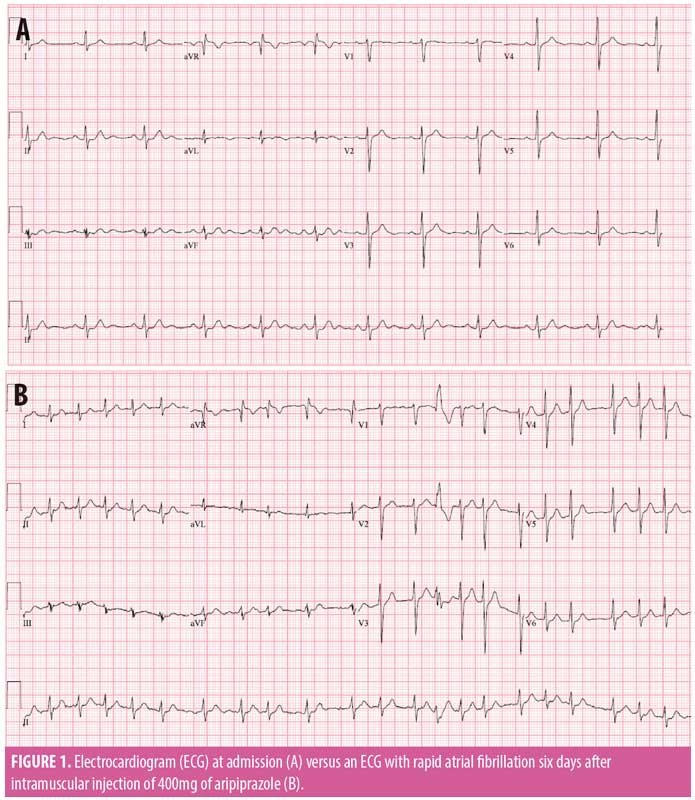
Six days after injection with aripiprazole, the hospitalized patient reported feeling unwell while doing “push-ups,” a part of his morning exercise routine. He reported shortness of breath and palpitations. His blood pressure varied between 133/67mmHg and 152/76mmHg, and his pulse ranged from 100 to 150 beats/minute, with a stable respiratory rate of 18 beats/minute. Heart sounds were irregular but physical examination was otherwise unremarkable. ECG indicated new AF (Figure 1B). He was given 2.5mg of metoprolol intravenously at 20-minute intervals over 60 minutes (7.5mg total) and two doses of intravenous amiodarone (150mg each, intravenously). He converted to normal sinus rhythm by the next day after receiving three additional oral doses of amiodarone (400mg per dose). A transthoracic echocardiogram showed normal cardiac function and no evidence of valvular abnormalities. Serum concentration of thyroid-stimulating hormone was within the normal range, and serial troponin levels were not elevated. The oral dose of aripiprazole was reduced to 5mg once daily and was continued for eight days to complete the 14 days of overlap with the injection, as recommended by the manufacturer. He was monitored in the hospital for an additional four days by nursing and medical personnel. He was evaluated and followed by the cardiology service, and several daily ECGs during hospitalization depicted normal sinus rhythm. Reduction of oral aripiprazole dose did not lead to an exacerbation of manic or psychotic symptoms in this patient. He remained clinically stable and medically asymptomatic until discharge.
At the five-month, outpatient follow-up, our patient’s medication regimen consisted of only 400mg of long-acting aripiprazole injection every four weeks, to which he adhered since his discharge from hospital. He reported no recurrence of palpitations or other symptoms of AF. His psychiatric condition remained stable, and he had no further psychiatric hospitalizations.
Discussion
Six days after aripiprazole had been well-tolerated orally, newly administered long-acting aripiprazole by intramuscular injection led to the onset of new AF in association with physical exertion. These circumstances suggest a potential association between the onset of AF and the large, first dose of injected aripiprazole in addition to the oral dose of aripiprazole. This antipsychotic agent is considered to be relatively safe in regard to its cardiac risks,2 whereas some other second-generation antipsychotics have been associated with new onset of AF.3–5 The long elimination half-life of aripiprazole (approximately 75 hours) and of its pharmacologically active metabolite dehydroaripiprazole (approximately 94 hours) adds to the duration of exposure and might increase the risk of adverse effects.1 Long-acting injected aripiprazole reaches maximum serum concentrations within 5 to 7 days,1 indicating a temporal association between the injection of the drug and onset of AF. Moreover, in general, the risk of cardiac dysrhythmias, including AF following an injection of an antipsychotic drug is reported to be greater than with oral administration.6
Adverse events associated with oral aripiprazole reportedly have a peak onset within the first four weeks of administration and subside over time.7 In addition, patients are reported to be more likely to experience treatment-emergent adverse events during the first eight days of receiving both oral and injectable antipsychotics.8 The present patient experienced AF after adding long-acting injectable aripiprazole to oral aripiprazole. but tolerated future doses of long-acting aripiprazole only, suggesting that the AF might have been related to the total dose of aripiprazole or might be an effect of the newly injected drug.
AF is of particular concern because it increases risk of cerebral ischemia or stroke, both of which have been associated with the use of many second-generation antipsychotic drugs, particularly in older patients and in association with diabetes mellitus, cardiac insufficiency, and history of stroke.9–11 AF is usually multifactorial. In the present case, prolonged abuse of alcohol might have predisposed the patient to cardiac dysrhythmia.12,13 Exercise can also increase the risk of AF.14 In addition, the risk of AF might be increased in major affective disorders with psychosis, possibly because of other underlying conditions and confounding factors, such as comorbid obesity, metabolic syndrome, systemic inflammation, and neurotransmitter imbalances.15,16
Conclusion
In summary, although it is not possible to exclude confounding factors, the timing and dose-dependent effect of aripiprazole administration in our patient suggests an association between an initial intramuscular injection of long-acting aripiprazole and new onset of AF. This observation calls for clinical vigilance, not only in patients with additional risk factors for stroke but also in younger patients who might have predisposing factors for arrhythmias.
References
- CPS (Canadian Pharmacists Association). Available at: http://www.e-therapeutics.ca. Accessed January 1, 2017.
- Polcwiartek C, Sneider B, Graff C, et al. Cardiac safety of aripiprazole treatment in patients at high risk for torsade: systematic review with a meta-analytic approach. Psychopharmacology (Berl). 2015;232(18):3297–3308.
- Low RA, Fuller MA, Popli A. Clozapine induced atrial fibrillation. J Clin Psychopharmacol. 1998;18(2):170.
- Waters BM, Joshi KG, Flynn J. Olanzapine-associated new-onset atrial fibrillation. J Clin Psychopharmacol. 2008;28(3):354–355.
- Çam B, Gülseren L, Mete L, Gülseren S. [Clozapine and olanzapine associated atrial fibrillation: case report]. Turk Psikiyatri Derg. 2015;26(3):221–226. Article in Turkish.
- Chou RH, Lo LW, Liou YJ, et al. Antipsychotic treatment is associated with risk of atrial fibrillation: nationwide nested case-control study. Int J Cardiol. 2017;227:134–140.
- Fleischhacker WW, Sanchez R, Johnson B, et al. Long-term safety and tolerability of aripiprazole once-monthly in maintenance treatment of patients with schizophrenia. Int Clin Psychopharmacol. 2013;28(4):171–176.
- Potkin SG, Raoufinia A, Mallikaarjun S, et al. Safety and tolerability of once monthly aripiprazole treatment initiation in adults with schizophrenia stabilized on selected atypical oral antipsychotics other than aripiprazole. Curr Med Res Opin. 2013;29(10):1241–1251.
- Douglas IJ, Smeeth L. Exposure to antipsychotics and risk of stroke: self-controlled case series study. BMJ. 2008;337:a1227.
- Gill SS, Rochon PA, Herrmann N, et al. Atypical antipsychotic drugs and risk of ischæmic stroke: population based retrospective cohort study. BMJ. 2005;330(7489):445.
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983–938.
- Voskoboinik A, Prabhu S, Ling LH, et al. Alcohol and atrial fibrillation: a sobering review. J Am Coll Cardiol. 2016;68(23):2567–2576.
- Whitman IR, Agarwal V, Nah G, et al. Alcohol abuse and cardiac disease. J Am Coll Cardiol. 2017;69(1):13–24.
- Kokubo Y, Matsumoto C. Traditional cardiovascular risk factors for incident atrial fibrillation. Circ J. 2016;80(12):2415–2422.
- Yang HY, Huang JH, Hsu CY, et al. Bipolar disorder and schizophrenia present different risks of atrial fibrillation: nationwide population-based analysis. Acta Cardiol Sinica. 2014;30(1):46–52.
- Chung FP, Lin YJ. Connection between cardiac and mental disorder: atrial fibrillation in patients with psychiatric disorder. Acta Cardiol Sin. 2014;30(1):53–55.





