 by Rajshekhar Bipeta, MBBS, DPM, DNB (psych); Srinivasa SRR Yerramilli, MD (psych); Ashok Reddy Karredla, MD (psych); and Srinath Gopinath, MBBS, DPM
by Rajshekhar Bipeta, MBBS, DPM, DNB (psych); Srinivasa SRR Yerramilli, MD (psych); Ashok Reddy Karredla, MD (psych); and Srinath Gopinath, MBBS, DPM
Dr. Bipeta is a consultant psychiatrist from Rajasri Clinic, Hyderabad, Telangana, India, and Drs. Yerramilli and Karredla are consultant psychiatrists from Hyderabad, Telangana, India; and Dr. Gopinath is with SUNY Downstate Medical Center, Brooklyn, New York, USA.
Innov Clin Neurosci. 2015;12(3–4):14–23.
Funding: No funding was provided for the preparation of this article.
Financial disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Internet addiction, obsessive-compulsive disorder, OCD, psychopathology, Internet Addiction Test, Young’s Diagnostic Questionnaire
Abstract: Whether internet addiction should be categorized as a primary psychiatric disorder or the result of an underlying psychiatric disorder still remains unclear. In addition, the relationship between internet addiction and obsessive-compulsive disorder remains to be explored. We hypothesized that internet addiction is a manifestation of underlying psychopathology, the treatment of which will improve internet addiction. We enrolled 34 control subjects (with or without internet addiction) and compared them to 38 patients with “pure” obsessive-compulsive disorder (with or without internet addiction). Internet addiction and obsessive-compulsive disorder were diagnosed based on Young’s Diagnostic Questionnaire and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), respectively. Age and Internet Addiction Test scores were comparable in both the control (years: 26.87±6.57; scores: 43.65±11.56) and obsessive-compulsive disorder groups (years: 27.00±6.13 years, p=0.69; scores: 43.47±15.21, p=0.76). Eleven patients with obsessive-compulsive disorder (28.95%) were diagnosed with internet addiction as compared to three control subjects (p=0.039). In the obsessive-compulsive disorder group, no difference in the Yale-Brown Obsessive Compulsive Scale (24.07±3.73 non-internet addiction, 23.64±4.65 internet addiction; p=0.76) score was seen between the internet addiction/obsessive-compulsive disorder and non-internet addiction/obsessive-compulsive disorder groups. As expected, the Internet Addiction Test scores were higher in the internet addiction/obsessive-compulsive disorder group (64.09±9.63) than in the non-internet addiction/obsessive-compulsive disorder group (35.07±6.37; p=0.00). All enrolled patients with obsessive-compulsive disorder were subsequently treated for a period of one year. Treatment of obsessive-compulsive disorder improved Yale-Brown Obsessive Compulsive Scale and Internet Addiction Test scores over time. At 12 months, only two of the 11 patients with obsessive-compulsive disorder (18.18%) fulfilled the Young’s Diagnostic Questionnaire criteria for internet addiction. In conclusion, treatment of the underlying disorder improved internet addiction.
Introduction
Internet addiction (IA) is being increasingly regarded as an emerging disorder with significant detrimental implications,[1–4] particularly in countries with easy and fast accessibility to the internet.[1] Along with the emergence of IA, the world of psychiatry has also witnessed a pervasive and enduring debate as to whether IA should be regarded as an independent psychiatric disorder[5] or a manifestation of an underlying psychiatric disorder.[6] Many researchers are of the view that IA merits an autonomous label,[5] and, based on the comorbid conditions, symptom-dimensions, and responses that patients with IA exhibit, conceptualize IA as a form of an impulse-control disorder (ICD),[7–9] or a behavioral addiction.[10,11]
Supporters of IA as an ICD argue that the prolonged duration of internet use is experienced by patients with IA as being “ego-syntonic,” corresponding to pleasure or even euphoria.[7,10] This is in contrast to obsessive-compulsive disorder (OCD), which has also been correlated with IA, wherein obsessions are regarded as “ego-dystonic,” or causing significant distress and anxiety. In the study by Shapira et al,[7] every subject’s problematic internet use met criteria for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) ICD-not otherwise specified (ICD-NOS).[12] Consistent with this finding, subjects rated the distress associated with thoughts, impulses, or urges to use the internet as well as the degree of effort made to resist the excessive internet use as low. In addition, some researchers are of the view that IA is an impulsive-compulsive spectrum disorder,[5] and both “ego-dystonic” and “ego-syntonic” as well as mixed subtypes of IA may exist.[6]
Proponents of IA as a behavioral addiction put forth the classical hallmarks of addiction as the diagnostic criteria, including salience, mood modification, tolerance, withdrawal, conflict, relapse, and inability to cut back.[13,14] In addition, they propose classification of IA into subtypes based on the type of addiction related to the type of content searched online (gaming, pornography, or social networking).[10]
Although IA has been the focus of much research in recent times, no consensus on the conceptualization, and hence, the diagnostic criteria of IA has been reached. In addition, IA has not been officially recognized as an independent psychiatric disorder in the recently published fifth edition of the DSM (DSM-5),[15] as further research and more evidence is required to establish it as a primary disorder.[6,16] One of the main reasons for this is the finding that patients with IA frequently have “comorbid” psychopathological conditions,[6] and these underlying conditions may explain IA.[6,10]
A number of studies investigated the association between IA and psychopathology. IA was found to be associated with depression,[7,17–22] obsessive-compulsive (OC) symptoms/disorder,[7,17–20] other anxiety disorders,[7,19] aggression and hostility,[21,23] substance-use,[7] attention deficit hyperactivity disorder (ADHD),[18,19] ICDs,[7] eating disorders,[7,19] bipolar disorder,[7] and personality disorders.[19] In addition, some researchers investigated the association of IA with personality traits, and demonstrated lower conscientiousness,[24] anxious temperament,[25] and impulsivity[26,27] to be positively related to IA. Other researchers investigated the effect of parent-child relationship28 and morningness-eveningness[29] on IA. Morningness-eveningness denotes individual preferences in sleep-wake patterns (the time of day the individual likes to wake up, feels and performs best, and goes to sleep); “morning types” like to rise early in the morning and go to bed early, while “evening types” prefer to sleep until later in the day and stay up until later at night.
In view of these findings, some researchers are of the view that IA is a manifestation of an underlying psychopathology or a form of escape from existing mental states and should not be regarded as a distinct psychiatric disorder.[6,30] However, it is clear that IA exacerbates negative affect and has deleterious psychosocial and functional consequences,[1–4,18,31,32] and patients with IA may require professional care and treatment. Consistent with the hypothesis that IA is a manifestation or an extension of the behavior resulting from underlying psychopathology and considering the negative impact of IA, it is imperative that patients presenting with IA as the chief complaint be screened for psychopathological/psychiatric conditions and vice versa. This may involve a comprehensive assessment of the patient, followed by treatment of the underlying condition, which may alleviate both the underlying condition as well as the “comorbid” IA.
OCD is characterized by the occurrence of unwanted and recurrent thoughts, ideas, feelings, urges, or mental images (called obsessions) that drive an individual to engage in behaviors or mental acts (called compulsions) designed to prevent or reduce anxiety and distress.[12] Common obsessions include ruminative thoughts about contamination, repeated doubts, orderliness, aggressive impulses, and sexual imagery, while common compulsions comprise repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, counting, repeating words silently). In practice, clinicians often find it difficult to distinguish obsessions and compulsions of OCD from “impulses” of ICD, and, at times, ICDs are misdiagnosed as OCD.[33]
One of the important distinctions between OCD and ICD is that ICDs are characterized by failure to resist “impulses,” whereas (although obsessions of OCD are difficult to resist) patients with OCD try to resist obsessions,[12,34] and many patients with OCD are able to resist obsessions up to a certain point. In addition, obsessions, in many individuals with OCD, cause marked anxiety and distress. However, the distress associated with “impulses” of ICD is low.[12,35]
Although the term impulse is associated with ICDs, both the DSM-IV and DSM-5 use the term impulses in the definition of obsessions of OCD. The DSM-IV[12] definition of obsessions of OCD is “recurrent and persistent thoughts, impulses, or images that are experienced, at some time during the disturbance, as intrusive and inappropriate, and that cause marked anxiety and distress.” In DSM-5,[15] the definition is slightly modified and includes both “urges” and “impulses.” According to Leckman et al,[33] the term impulse is possibly confusing, in that impulses are characteristic of the impulse-control disorders. They recommend replacing “impulse” with “urge,” as “impulse” indirectly refers to the notion of ICDs.
Another feature that distinguishes OCD from ICD is that in ICD, acting on the “impulses” causes pleasure or gratification,[12,34] while performance of compulsions in OCD is to prevent or reduce anxiety.[33] For example, a patient with kleptomania gets pleasure while stealing, and following the act, feels relieved. On the other hand, an OCD patient with obsessions related to contamination, while engaging in compulsive washing, may, although transiently get initial relief or reduction of mental discomfort,[36] feels distress, and following the act, feels guilty.
Since OCD patients have a tendency to ritualistic behavior because of the nature of the underlying disease, they may be at risk of developing IA. Patients with OCD may experience unwanted and recurrent thoughts of, for example, “surfing the internet,” or unwanted images of “seeing the computer screen.” Considering that these phenomena are mental experiences, such experiences may constitute bona fide obsessions according to the DSM-IV criteria.[12] In addition, patients with OCD may experience repeated, persistent, difficult-to-resist urges (obsessions) to surf the internet or stay online (though they do not want to), which leads to anxiety and distress. Similarly, like other compulsions (e.g., hand washing), once the individual logs online, he or she may not be able to control his or her internet use and will keep browsing the internet repeatedly (compulsive act), though this is followed by distress and guilt when the act is over.
Hence, we propose that a subset of patients with IA have underlying or comorbid OCD, which makes it difficult for the patients to go offline once they start browsing, though they would actually like to.
The relationship between OC symptoms and IA has been investigated in a few studies. Significant correlation between IA and psychological symptoms (somatization, OC symptoms, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) was demonstrated in one study.[37] Among Symptom Checklist-90-Revised subscales, severity of OC symptoms was found to be the only predictor for IA scale scores in another study.[38] A longitudinal study that investigated freshmen students before and after development of IA, found an abnormal OC dimension before the students became addicted to the internet. After developing IA, significantly higher scores were observed for dimensions on depression, anxiety, hostility, interpersonal sensitivity, and psychoticism, suggesting that these were the outcomes of IA.[23] In yet another study, the OC symptoms were statistically associated with IA (chi² test=23.53, p=0.000), and the authors found that, among young people, there is a relationship between compulsive behavior and IA.[39] In a study by Chou et al,[2] OC symptoms were observed to be the most related symptoms in both genders in subjects with IA.
Since IA has been linked with OC symptoms/disorder and as we routinely treat OCD patients in our clinic, we explored the relationship between IA and OCD. We enrolled “pure OCD” patients (other psychopathologies were excluded) in our study and hypothesized that IA would be one of the “manifestations” in the pure OCD population enrolled and that treatment of OCD would improve both OCD and IA.
Methods
This study was approved by the Institutional Review Board and was conducted according to the ethical principles laid down by the Declaration of Helsinki.[40] The study setting was an outpatient psychiatric clinic in Hyderabad, Telangana, India.
OCD was diagnosed by a board certified psychiatrist (with over fourteen years of clinical and academic experience) according to DSM-IV criteria.[12] Age-matched controls were the non-relatives accompanying all psychiatric patients (e.g., friends, neighbors). Enrolled subjects with OCD were selected from individuals who presented to the psychiatric outpatient clinic for treatment of OCD. OCD subjects and control subjects provided written informed consent to participate in the study and were consecutively enrolled based on the following inclusion criteria: 1) 18 years of age or older, 2) either gender, 3) completion of high school and literate in the English language, and 4) ability to access the internet.
Additional inclusion criteria for OCD subjects included 1) not receiving any treatment for the previous six months and 2) good insight into their illness. Exclusion criteria for OCD and control subjects were 1) presence of comorbid Axis I disorders (e.g., major depressive disorder, ADHD), 2) a total score of 55 or greater on the Barratt’s Impulsivity Scale-11[41] (BIS-11) (to exclude comorbid impulsivity), 3) a history of substance abuse/dependence within the previous one year, and 4) presence of any personality disorder. Comorbidity was excluded based on clinical interview.
This was a two-phased naturalistic study. In Phase 1, OCD and control subjects were administered standard instruments and compared. In Phase 2 of the study, OCD subjects were treated over a period of one year and assessed periodically.
Standard instruments. BIS-11.[41] BIS-11 assesses impulsivity in three domains: motor impulsiveness, nonplanning impulsiveness, and attentional impulsiveness. It is a self-administered, 30-item, 4-point scale. According to Stanford et al,[42] BIS-11 has good internal consistency, with Cronbach’s alpha ranging from 0.79 to 0.83, good validity, and moderate correlations with other measures of impulsivity.
Yale-Brown Obsessive Compulsive Scale (YBOCS). The Y-BOCS is a 10-item, 0- to 4-scored clinician-rated instrument to determine the severity of OCD and to monitor improvement during treatment. The interrater reliability is 0.72 to 0.98, and intra-class correlation is 0.80.[43]
Young’s Diagnostic Questionnaire (YDQ). According to YDQ, subjects are considered to have IA if they answer yes to five or more of the questions.[32]
Internet Addiction Test (IAT).[44] The IAT is a 20-item measure of severity of IA, with high face and concurrent validity. Internal consistency has been found for six factors with alpha coefficients ranging from 0.54 to 0.82.[45] The higher the score on the IAT, the greater the severity of IA.[44]
Data analyses. Data were analyzed using SPSS v 20.0 (IBM Corp.). Demographic characteristics were summarized using descriptive statistics. Due to the small sample size of the IA control group, the two control groups (with and without IA) were not compared statistically with each other.
Cross-sectional analysis was performed using appropriate nonparametric tests (Pearson’s chi-square test for comparing the number of male subjects and the number of subjects with IA) or parametric tests (t-test for comparing age, duration of OCD, IAT scores, and YBOCS scores). Repeated measures MANOVA was used to analyze longitudinal data. Pearson’s correlation coefficient was used to analyze the relationship of YBOCS scores with IAT scores in the two OCD groups (with and without IA).
Results
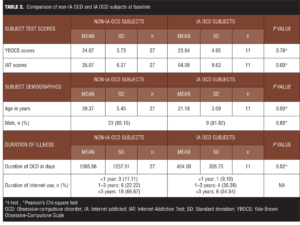
Phase 1. Overall, 72 subjects (38 OCD, 34 controls) were enrolled. The mean age of the study sample was 26.72±6.24 years. Table 1 presents the comparison of control subjects and OCD subjects. Table 2 presents comparison of non-IA OCD and IA OCD subjects at baseline. No difference in OCD severity (YBOCS) was evident between the two groups. The IA OCD group tended to be younger with a shorter duration of OCD.
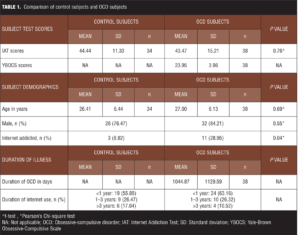
Of the 11 IA OCD subjects, one had four types of OCD symptoms, one had three types, one had two types, and eight had one type of symptom. The OCD symptoms observed were checking (5 subjects, 45.45%); symmetry, ordering, and arranging compulsions (4 subjects, 36.36%); aggressive, harming obsessions (3 subjects, 27.27%); dirt/contamination obsessions (2 subjects, 18.18%); washing and cleaning compulsions (2 subjects, 18.18%); and sexual obsessions (1 subject, 9.09%).
Among the 27 non-IA OCD subjects, two had four types of symptoms, one had three types, five had two types, and 19 had one type of symptom. The OCD symptoms seen were dirt/contamination obsessions (11 subjects, 40.74%); sexual obsessions (8 subjects, 29.62%); religious obsessions (7 subjects, 25.92%); hoarding (4 subjects, 14.81%); symmetry, ordering, and arranging compulsions (3 subjects, 11.11%); washing and cleaning compulsions (2 subjects, 7.4%); and somatic obsessions (2 subjects, 7.4%); and counting compulsions (1 subject, 3.7%).
Phase 2. According to the study protocol, OCD subjects were to be treated for one year. All of the OCD subjects (IA OCD, n=11; non-IA OCD, n=27) were provided standard pharmacological treatment for OCD (treatment as usual [TAU]). All OCD subjects received clonazepam, which was tapered off in three weeks, in addition to either a selective serotonin reuptake inhibitor (SSRI) or clomipramine. In the IA OCD group, five subjects received fluvoxamine (4 subjects, 200mg/day; 1 subject, 150mg/day), four received sertraline (3 subjects, 150mg/day; 1 subject, 200mg/day), one received fluoxetine (60mg/day), and one received clomipramine (200mg/day). Similarly, in the non-IA OCD group, eight received fluvoxamine (1 subject, 150mg/day; 5 subjects, 200mg/day; 2 subjects, 300mg/day), five received sertraline (1 subject, 100mg/day; 2 subjects, 150mg/day; 2 subjects, 200mg/day), 11 received fluoxetine (2 subjects, 40mg/day; 7 subjects, 60mg/day; 2 subjects, 80mg/day), and three received clomipramine (1 subject, 150mg/day; 2 subjects, 200mg/day).
Overall, five of the 38 OCD subjects were lost to follow-up at various time points. All remaining OCD subjects were administered YBOCS and IAT at three months, six months, and 12 months of treatment; and YDQ was administered at 12 months.
Repeated-measures MANOVA analyses confirmed that there were significant multivariate between-subjects (IA OCD group vs. non-IA OCD group) effects (V [0.876], F [2, 30]=105.713, p=0.00; partial eta-squared=0.876), with-in subject (time point) effects (V [0.983], F [6, 26]=252.107, p=0.00; partial eta-squared=0.983), and the interaction between IA status and time point (V [0.834], F [6, 26]=21.813, p=0.00; partial eta-squared=0.834) (Table 3). Univariate between-group analyses showed that YBOCS scores were not significantly different across IA OCD groups (F [1, 31]=0.060, p=0.808; partial eta-squared=0.002), while IAT scores were significantly higher in the IA OCD group than the non-IA OCD group (F [1, 31]=59.500, p=0.00; partial eta-squared=0.657). Within-group univariate analyses indicated that YBOCS scores (F [2.365, 73.312]=455.527, p=0.00; partial eta-squared=0.936) and IAT scores (F [2.113, 65.493]=77.312, p=0.00, partial eta-squared=0.714) significantly improved from baseline to 12 months (irrespective of the IA group).

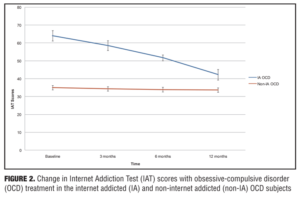
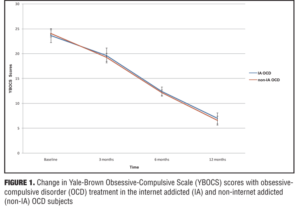
There was a significant interaction between IA status and time point for IAT scores (F [2.113, 65.493]=77.312, p=0.00; partial eta-squared=0.714), but not for YBOCS scores (Figure 1) (F [2.365, 73.312]=1.169, p=0.322; partial eta-squared=0.036), indicating that the IAT scores in the IA OCD group decreased more steeply than those in the non-IA OCD group (Figure 2), while the decrease in YBOCS scores was more or less comparable between the two groups (Figure 1). Further analyses of the interaction for IAT scores revealed that IAT scores were higher in the IA OCD group at baseline (t [36]=-10.936; p=0.00), three months (t [36]=-9.190; p=0.00), six months (t [34]= -7.793; p=0.00) and were maintained at 12 months (t [31]=-3.173; p=0.003).
Improvements in IAT scores were greater in the IA OCD group than the non-IA OCD group at all time points (Figure 2). At 12 months, out of the 11 IA OCD subjects, only two (18.18%) IA OCD subjects still met the criteria for IA.
The relationship between YBOCS and IAT scores was analyzed using Pearson’s correlation coefficient at the four time points during the one-year treatment period. Correlation was significant at baseline (r=0.404; p=0.012), three months (r=0.489; p=0.002), six months (r=0.347; p=0.038), and 12 months (r=0.526; p=0.002).
Discussion
Almost all of the studies conducted to date in the field of IA have demonstrated the existence of comorbid psychopathological/ psychiatric conditions in patients with IA.[5–7,9,18,19] This issue of psychiatric comorbidity has raised concerns regarding whether IA should be categorized as a bona fide psychiatric disorder or a secondary manifestation of an underlying psychiatric disorder. In our study, a greater number of the OCD subjects exhibited IA symptoms than did the control subjects. If viewed conversely, this finding is in concordance with studies that have demonstrated high rates of psychiatric comorbidity with IA, including OCD, ICDs, depression, anxiety, ADHD, and personality disorders, although we excluded other psychiatric comorbidities from our study and enrolled subjects considered to have “pure” OCD.
If regarded as a secondary manifestation of the primary disorder, it seems logical that IA should respond to therapy for the underlying primary disorder. To this end, we attempted to treat all OCD subjects in our study alike, assuming no differences in severity in the two groups of OCD patients (those with IA and those without). This was also demonstrated by our results; no differences in YBOCS scores were evident between the two groups. As expected, therapy for OCD improved YBOCS and IAT scores in both the groups and, at 12 months, only two of the 11 subjects in the IA OCD group (18.18%) fulfilled IA YDQ criteria. Therefore, the diagnostic stability of IA was not seen at 12 months. A point worth mentioning here is that all OCD subjects were given standard pharmacological treatment for OCD, and no specific treatment was provided for IA. It may also be reasonable to assume that the two IA OCD subjects who still met the criteria for IA at the end of the study might have improved further had they received treatment for a longer duration. In addition, an overall significant decrease in IAT scores of the non-IA OCD subjects was also observed, although this decrease was not as steep as that in the IA OCD group, given the non-IA OCD group’s low IAT scores at baseline and hence less room for improvement. However, the decrease in YBOCS scores was more or less comparable between the two groups. Thus, our study shows that, over a period of one year, treatment of the underlying disorder (OCD) improved OCD as well as IAT scores, in both IA OCD and non-IA OCD groups.
The results of our study are in agreement with other studies in which therapy was chosen based on the comorbid psychiatric conditions (depression and anxiety),[46–50] and was found to be effective in the treatment of IA. Our findings, therefore, lend further support to the concept that treatment of the underlying or comorbid psychiatric condition improves IA. Studies investigating treatment for IA have employed anti-depressants, such as SSRIs,[47–51] bupropion,[52] as well as psychostimulants, such as methylphenidate[53] or even the opiate antagonist, naltrexone.[54] In one of the studies, SSRIs decreased the duration of internet use.[51] In another study, craving for internet video game playing was reduced, as were total game play time and cue-induced brain activity in dorsolateral prefrontal cortex after a six-week period of bupropion treatment.[52] In the study that employed methylphenidate in 62 internet video game-playing children diagnosed with ADHD,[53] the YDQ Korean version scores and internet usage times were significantly reduced after eight weeks of treatment.
Limitations. Given the effectiveness of treatment of the underlying or comorbid psychiatric condition, in our opinion, IA in our OCD subjects was a secondary manifestation of an underlying illness. However, a major limitation of our study is that we did not have a “pure” IA group (only three control subjects with IA without any comorbid psychiatric conditions). It may have been possible that the “pure” IA group would have responded well to SSRIs and, in that case, the hypothesis that both OCD and IA are autonomous, discrete disorders related to serotonergic dysfunction would be supported. In addition, it is at least theoretically possible that a treatment known to improve “pure” IA might also improve OCD (in an IA + OCD group), which would lead to the hypothesis that IA is the primary and OCD the secondary disorder. Therefore, the relationship between OCD and IA may not be accurately described by regarding OCD as the primary disorder and IA as a secondary manifestation of the underlying OCD. As mentioned below, more longitudinal studies are required to understand the true nature of IA.
Patients with OCD may be at higher risk for IA, and IA in such patients may signify adaptive “escape or relief-seeking” behavior from symptoms (obsessions), depression, or interpersonal discomfort resulting from the underlying disease. Due to the nature of obsessions in OCD, this “escape or relief-seeking” behavior may become repetitive and uncontrollable, resulting in a new spectrum of internet-related compulsions. However, in order to regard these internet-related behaviors as compulsions, it is imperative to know that the behavior is “ego-dystonic” or experienced as being “driven” or guilt-ridden, rather than pleasurable or tension-relieving. Our study did not investigate this aspect, and this remains an open area to be explored in future studies.
More carefully controlled studies are needed to resolve the diagnostic controversies shrouding IA. Research on IA needs to focus on investigating the diagnostic stability of IA over time (which we attempted in our study), reliability of the diagnostic criteria, neurobiological correlates and markers, genetic patterns of expression, and treatment response in order to delineate the true nature of IA.[6] More longitudinal studies investigating the temporal relationship between IA and other psychopathologies are required to clarify if IA is a secondary manifestation of the underlying disorder or is a true disorder in itself.[6,16] As stated by Pies,[6] “The precise definition of pathological internet use and its relationship to other psychiatric disorders requires additional investigation. The so-called IA should not be written off as another attempt by psychiatry to ‘medicalize’ unfortunate or self-destructive behaviors.”
Our study has certain other limitations as well. Since we enrolled only OCD patients, the findings from our study cannot be generalized to patients with other psychiatric disorders. We also did not study the relation between the type of obsessions and compulsions (e.g., hoarding, checking, counting, washing) with the type of IA (e.g., cybersexual, cyber-relationship, net compulsions, information overload, and computer addiction), as well as the temporal relationship between OCD and IA. Our study also used an unblinded design and had a small sample size.
Nevertheless, one of the key strengths of our study was its longitudinal design. Most of the published studies on IA are cross-sectional[18–22] and, if longitudinal, have not studied the effect of treatment.[23] In addition, to the best of our knowledge, this is the first study investigating 1) IA in a OCD-treatment seeking clinical population, 2) the relationship between “pure” OCD and IA, 3) whether treatment of the primary disorder improves IA, and 4) the treatment of IA in Indian patients.
Conclusion
In conclusion, due to the increasing number of patients with IA worldwide, it is important that clinicians be aware of IA and its associated symptoms. Unless consensus is achieved regarding the approach to the IA patient, it is pragmatic and reasonable to employ a step-wise approach. Every treatment-seeking IA patient should be screened for underlying or comorbid psychiatric/ psychopathological condition(s), and after careful consideration of patient history, treatment should be directed against this condition(s) based on the clinical presentation and severity of symptoms. In case of no or partial response to therapy, other drugs shown to be effective in IA may be added.
Author Contributions
Rajshekhar Bipeta (RB) was involved in conceptualizing and designing the study and was a major contributor in preparing and writing the manuscript. RB acquired the data and performed all the assessments. RB, Srinivasa SRR Yerramilli, Ashok Reddy Karredla, and Srinath Gopinath analyzed and interpreted the data. All the authors were involved in revising and editing the manuscript critically for important intellectual content and read and gave approval for the final version of the manuscript to be published. All the authors made substantial intellectual contributions to this study and participated sufficiently in the work. All authors take public responsibility for appropriate portions of the content and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. RB is the guarantor for this study.
Acknowledgments
The authors sincerely thank Ms. Romana Zulfiqar, Romed Communications, New Delhi, India, for providing statistical assistance and helping in the preparation of this manuscript in the form of writing, copy-editing, and proof-reading. The authors wish to thank Dr. Prasad UV, formerly Research Scholar, National Institute of Nutrition, Hyderabad, India; Mr. Sundaresh Peri, retired lecturer of biostatistics, Kakatiya Medical College, Warangal, India; and Dr. Farooq A. Khan, Consultant Psychiatrist, Birmingham & Solihull Mental Health NHS Foundation Trust, England, for their advice. The authors also want to express their gratitude to the anonymous Innovations in Clinical Neuroscience peer reviewers for spending their valuable time reviewing the manuscript and for their scholarly and constructive comments.
References
1. Ahn DH. Korean policy on treatment and rehabilitation for adolescents’ internet addiction. Presented at 2007 International symposium on the counseling and treatment of youth internet addiction. Seoul, Korea, National Youth Commission 2007:49.
2. Chou C, Condron L, Belland JC. A review of the research on internet addiction. Educ Psychol Rev. 2005;17:363–388.
3. Kraut R, Patterson M, Lundmark V, et al. Internet paradox: a social technology that reduces social involvement and psychological well being? Am Psychol. 1998;53:1017–1031.
4. Tsai C-C, Lin SSJ. Internet addiction of adolescents in Taiwan: an interview study. Cyberpsychol Behav. 2003;6:649–652.
5. Block JJ. Issues for DSM-V: internet addiction. Am J Psychiatry. 2008;165:306–307.
6. Pies R. Should DSM-V designate “internet addiction” a mental disorder? Psychiatry (Edgmont). 2009;6:31–37.
7. Shapira NA, Goldsmith TD, Keck PE Jr, et al. Psychiatric features of individuals with problematic internet use. J Affect Disord. 2000;57:267–272.
8. Beard KW, Wolf EM. Modification in the proposed diagnostic criteria for internet addiction. Cyberpsychol Behav. 2001;4:377–383.
9. Mazhari S. Association between problematic internet use and impulse control disorders among Iranian university students. Cyberpsychol Behav Soc Netw. 2012;15:270–273.
10. Hinic D. Problems with ‘internet addiction’ diagnosis and classification. Psychiatr Danub. 2011;23:145–151.
11. Ko CH, Yen JY, Chen CC, et al. Proposed diagnostic criteria of internet addiction for adolescents. J Nerv Ment Dis. 2005;193:728–733.
12. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fouth Edition. Washington, DC: American Psychiatric Press, Inc.; 1994.
13. Griffiths MD. Internet addiction: does it really exist? In: Gackenbach J, ed. Psychology and the Internet. New York, NY: Academic Press; 1998:61–75.
14. Grif?ths MD. Does internet and computer addiction exist? Some case study evidence. Cyberpsychol Behav. 2000;3:211–218.
15. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth 15. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Press Inc.; 2013.
16. Morahan-Martin J. Internet abuse: Addiction? Disorder? Symptom? Alternative explanations? Soc Sci Comput Rev. 2005;23:39–48.
17. Jang KS, Hwang SY, Choi JY. Internet addiction and psychiatric symptoms among Korean adolescents. J Sch Health. 2008;78:165–171.
18. Ha JH, Yoo HJ, Cho IH, et al. Psychiatric comorbidity assessed in Korean children and adolescents who screen positive for internet addiction. J Clin Psychiatry. 2006;67:821–826.
19. Bernardi S, Pallanti S. Internet addiction: a descriptive clinical study focusing on comorbidities and dissociative symptoms. Compr Psychiatry. 2009;50:510–516.
20. Kim K, Ryu E, Chon MY, et al. Internet addiction in Korean adolescents and its relation to depression and suicidal ideation: a questionnaire survey. Int J Nurs Stud. 2006;43:185–192.
21. Yen JY, Ko CH, Yen CF, et al. The comorbid psychiatric symptoms of Internet addiction: attention deficit and hyperactivity disorder (ADHD), depression, social phobia, and hostility. J Adolesc Health. 2007;41:93–98.
22. Ko CH, Yen JY, Chen CS, et al. Psychiatric comorbidity of internet addiction in college students: an interview study. CNS Spectr. 2008;13:147–153.
23. Dong G, Lu Q, Zhou H, Zhao X. Precursor or sequela: pathological disorders in people with internet addiction disorder. PLoS One. 2011;6:e14703.
24. Müller KW, Koch A, Dickenhorst U, et al. Addressing the question of disorder specific risk factors of internet addiction: a comparison of personality traits in patients with addictive behaviors and comorbid internet addiction. BioMed Res Int. 2013; 2013: Article ID 546342, 7 pages.
25. Ozturk FO, Ekinci M, Ozturk O, Canan F. The relationship of affective temperament and emotional behavioral difficulties to internet addiction in Turkish teenagers. ISRN Psychiatry. 2013;2013:961734.
26. Lee HW, Choi JS, Shin YC, et al. Impulsivity in internet addiction: a comparison with pathological gambling. Cyberpsychol Behav Soc Netw. 2012;15:373–377.
27. Choi JS, Park SM, Roh MS, et al. Dysfunctional inhibitory control and impulsivity in Internet addiction. Psychiatry Res. 2014;215:424–428.
28. Wu X, Chen X, Han J, et al. Prevalence and factors of addictive internet use among adolescents in Wuhan, China: interactions of parental relationship with age and hyperactivity impulsivity. PLoS One. 2013;8:e61782.
29. Lin YH, Gau SS. Association between morningness eveningness and the severity of compulsive internet use: the moderating role of gender and parenting style. Sleep Med. 2013;14:1398–1404.
30. Miller MC. Questions & answers. Is “internet addiction” a distinct mental disorder? Harv Ment Health Lett. 2007;24:8.
31. Orzack M. Computer addiction: is it real or virtual? Harv Ment Health Lett. 1999;15:8.
32. Young K. Internet addiction: The emergence of a new clinical disorder. Cyberpsychol Behav. 1998;1:237–244.
33. Leckman JF, Denys D, Simpson HB, et al. Obsessive-compulsive disorder: a review of the diagnostic criteria and possible subtypes and dimensional specifiers for DSM-V. Depress Anxiety. 2010;27:507–527.
34. Sadock BJ, Sadock VA, eds. Kaplan and Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins and Wolter Kluwer Health; 2003:782.
35. Winchel RM, Simson D, Yovell Y. Impulse control disorders. In: Tasman A, Kay J, Lieberman JA, eds. Psychiatry. 2nd ed. Indian reprint. Chichester, West Sussex, England: John Wiley & Sons Ltd; 2003:1555.
36. Hales RE, Yudofsky SC, eds. The American Psychiatric Publishing Textbook of Clinical Psychiatry. 4th ed. Washington DC: The American Psychiatric Publishing Inc; 2003:584.
37. Adal?er A, Balkan E. The relationship between internet addiction and psychological symptoms. The International Journal of Global Education. 2012;1:42–49.
38. Dalbudak E, Evren C, Topcu M, et al. Relationship of internet addiction with impulsivity and severity of psychopathology among Turkish university students. Psychiatry Res. 2013;210:1086–1091.
39. Cecilia MR, Mazza M, Cenciarelli S, et al. The relationship between compulsive behaviour and internet addiction. Styles of Commun. 2013;5:24–31.
40. World Medical Association. World Medical Association Declaration of HelsinkiEthical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194.
41. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–774.
42. Stanford MS, Mathias CW, Dougherty DM, et al. Fifty years of the Barratt Impulsiveness Scale: An update and review. Personality and Individual Differences. 2009;47:385–395.
43. Goodman WK, Price LH, Rasmussen SA, et al. The Yale–Brown Obsessive Compulsive Scale II. Validity. Arch Gen Psychiatry. 1989;46:1012–1016.
44. Young KS. Caught in the net: how to recognize the signs of internet addiction and a winning strategy for recovery. New York, NY: John Wiley & Sons; 1998.
45. Widyanto L, Mcmurran M. The psychometric properties of the internet addiction test. Cyberpsychol Behav. 2004;7:443–450.
46. Arisoy O. Internet addiction and its treatment. Psikiyatride Guncel Yaklasimlar. 2009;1:55–67.
47. Atmaca M. A case of problematic internet use successfully treated with an SSRI-antipsychotic combination. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:961–962.
48. Huang X-q, Li M-c, Tao R. Treatment of Internet addiction. Curr Psychiatry Rep. 2010;12:462–470.
49. Sattar P, Ramaswamy S. Internet gaming addiction. Can J Psychiatry. 2004;49:871–872.
50. Wieland DM. Computer addiction: implications for nursing psychotherapy practice. Perspect Psychiatr Care. 2005;41:153–161.
51. Dell’Osso B, Hadley S, Allen A, et al. Escitalopram in the treatment of impulsive-compulsive internet usage disorder: an open-label trial followed by a double-blind discontinuation phase. J Clin Psychiatry. 2008;69:452–456.
52. Han DH, Hwang JW, Renshaw PF. Bupropion sustained release treatment decreases craving for video games and cue-induced brain activity in patients with internet video game addiction. Exp Clin Psychopharmacol. 2010;18:297–304.
53. Han DH, Lee YS, Na C, et al. The effect of methylphenidate on internet video game play in children with attention-deficit/hyperactivity disorder. Compr Psychiatry. 2009;50:251–256.
54. Bostwick JM, Bucci JA. Internet sex addiction treated with naltrexone. Mayo Clin Proc. 2008;83:226–230.