 by Khurshid A. Khurshid, MD, FAASM
by Khurshid A. Khurshid, MD, FAASM
Dr. Khurshid is Clinical Associate Profressor and Chief of the Neuromodulation and Sleep Disorders Program in the Department of Psychiatry at the University of Florida College of Medicine in Gainsville, Florida.
Innov Clin Neurosci. 2018;15(3–4):28–32
Funding: No funding was received for the preparation of this article.
Disclosures: The author has no conflicts of interest relevant to the content of this article.
Abstract: Insomnia is a clinical problem of significant public health importance. Insomnia can be a symptom or harbinger of other psychiatric disorders. Insomnia can also be comorbid with other psychiatric disorders, thereby adding to the medical burden and increasing the risk of psychiatric relapse. Insomnia can also be associated with medical and neurological disorders. Some medications can also cause insomnia. Treatment of insomnia can lead to positive outcomes, not only by alleviating symptoms and moderating these comorbid disorders, but by preventing new episodes. Therefore, it is vital to be aware of the relationship between insomnia and psychiatric illness. This article reviews this relationship and provides recommendations for management.
Keywords: Insomnia, sleep disorder, psychiatric disorder, depression, psychosis, schizophrenia, anxiety disorder
Insomnia affects 25 million people in the United States annually and leads to an estimated $100 billion health care burden. Insomnia has also been shown to be a causal factor in other medical and psychiatric disorders, cognitive impairments, accidents, absenteeism, and reduced quality of life.1 The cost of not treating insomnia is more than the cost of treating insomnia.2 Insomnia as a symptom is seen in up to one third of the United States population, while the disorder is seen in up to 20 percent.3
The diagnostic criteria of insomnia have been updated in the International Classification of Sleep Disorders, Third Edition (ICSD-3) and the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The distinction between primary and secondary insomnia was removed from both classifications. Insomnia is a disorder unto itself that needs independent clinical attention. Viewing insomnia mainly as a symptom of another disorder prompted many clinicians to direct the bulk of their treatment efforts at the so-called primary disorder. Studies have shown that treating insomnia leads to better outcomes and improvement in co-existing psychiatric disorders. To achieve optimal treatment outcomes in people with comorbid psychiatric illness and insomnia, the clinician should target both disorders.4–7
Neurobiological Correlates of Insomnia and Psychiatric Disorders and Their Implications in Treatment
Monoaminergic neuronal regions promote wakefulness. These regions include basal forebrain (producing acetylcholine); locus ceruleus (located beneath floor of fourth ventricle), producing norepinephrine; dorsal raphe nucleus (located in brainstem), producing serotonin; tuberomammilary nucleus (located at the base of posterior hypothalamus), producing histamine; and ventral tegmental area, producing dopamine. Orexin and hypocretin are excitatory neuropeptides produced by neurons in the lateral and posterior hypothalamus that promote wakefulness. Gamma-aminobutyric acid (GAB) and glycine, which are produced in preoptic areas (particularly in the ventrolateral preoptic area [VLPO]), produce sleep.8
Conditions that induce high aminergic output and medications that increase central aminergic states can cause insomnia. Also, conditions that decrease inhibitory neurotransmission can cause insomnia. Anxiety and cognitive distortions seen in various psychiatric disorders can also contribute to hyperarousal seen in insomnia and perpetuate chronic insomnia.9
The same pathophysiological mechanisms that cause psychiatric disorders, such as depression, anxiety, and psychosis, can also cause insomnia or hypersomnia. Medications that increase serotonergic activity (e.g., selective serotonin reuptake inhibitors [SSRIs]) can cause insomnia. Increased dopaminergic states that are implicated in causation of psychosis can cause insomnia. This can also be true for drug-induced psychosis—the prototypical example is cocaine-induced psychosis and insomnia.
Insomnia and Depression
Insomnia is a diagnostic criterion of MDD (MDD). Insomnia is also rated on one or more items on various rating scales for depression, such as Patient Health Questionnaire (PHQ-9), Hamilton Depression Rating Scale (HAM-D), and Montgomery Asberg Depression Rating Scale (MADRS).10–12 Insomnia is seen in more than 90 percent of patients with clinical depression. Insomnia as a symptom has a 60- to 70-percent positive predictive value in diagnosing MDD13,14 More than 50 percent of patients presenting to sleep disorder clinics have insomnia, and those who present with insomnia have a higher prevalence of MDD.15
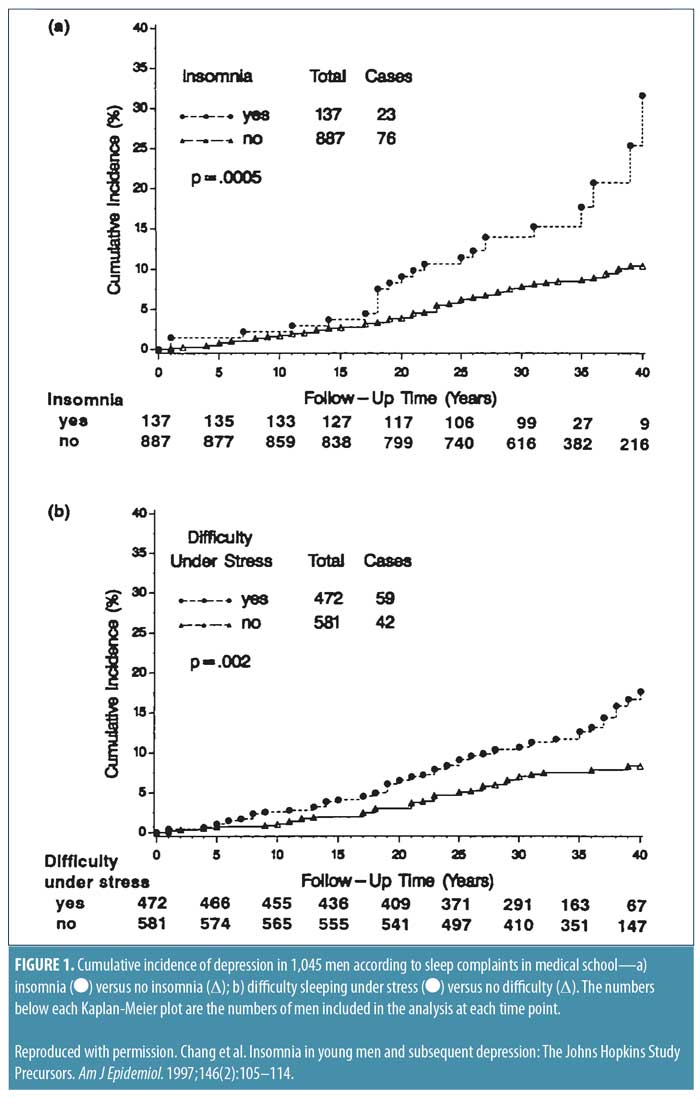
There is a bidirectional relationship between insomnia and depression.16 Insomnia can be a risk factor for subsequent development of depression. In a 40-year longitudinal follow-up of medical students, it was noted that those who had baseline insomnia were at higher risk for the subsequent development of MDD (relative risk [RR] 2.0, confidence interval [Cl] 1.2–3.3)] (Figure 1).17 Patients with insomnia but without depression displayed an odds ratio of 6.2 for developing depression later in life, while patients with depression but without insomnia had an odds ratio of 6.7 of developing insomnia later in life.12 In addition, in patients with insomnia and mood disorders, the insomnia preceded the mood disorder in 41 percent of patients, mood disorder preceded insomnia in 29 percent, and the symptoms appeared simultaneously in 29 percent.18
Insomnia is a marker for increased risk of suicidal thinking. Higher levels of insomnia and depression, as recorded with the HAM-D, corresponded to significantly greater intensity of suicidal thinking (p<0.01, p<0.001, respectively).19 Furthermore, the relation between suicidality and sleep disturbances has been shown even in the absence of mental disorders.20
Insomnia is also a risk factor for relapse in patients treated for depression.21 It has been shown that treatment of insomnia with cognitive behavior therapy in patients with depression resulted in a significantly greater decrease in depression scores, decreased relapse, and improved remission rates.22
Table 1 summarizes these implications.
Insomnia and Psychotic Disorders
Insomnia is common in patients with schizophrenia.23 Sleep problems might emerge during any stage of the illness, including the prodrome, first episode, acute recurrence, and even during remission stages. Severe insomnia is a hallmark of the prodromal phase of psychosis. Insomnia is also a major risk factor for impending relapse of psychosis. Sleep abnormalities might play an important role in identifying at-risk patients (i.e., those in the prodromal phase).21 Treatment of insomnia might play a role in prevention and treatment of psychosis.24 Although a number of patients with schizophrenia might report longer and better sleep on antipsychotics, many continue to report significant sleep difficulties, including early and middle insomnia.25
Sleep problems have been correlated with cognitive dysfunction in schizophrenia.28 Patients with schizophrenia tend to have circadian rhythm dysfunctions.26,27 These circadian rhythm abnormalities might be caused by decreased exposure to light due to psychotic symptoms, abnormalities in melatonin, and dysfunction of the suprachiasmatic nucleus.28
Recommendations for evaluation and treatment of Insomnia in patients with psychotic disorders include the following:
All patients with schizophrenia should be evaluated for insomnia.
Medical comorbidities should be evaluated to determine their contribution to the insomnia.
Caffeine is well known to cause insomnia, and its use should be limited to earlier in the day.
Patients with schizophrenia are often prescribed statins, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and SSRIs. These medications can cause insomnia. In cases where a medication is the presumed cause of sleep dysfunction, alternatives should be considered.
Sleep apnea is common in patients with psychotic disorders. It can contribute to insomnia and poor sleep quality. It should be managed with continuous positive airway pressure (CPAP) with supportive encouragement. Lifestyle modifications, positional therapy, use of oral appliances, and consultation with an ear, nose, and throat specialist should be explored in patients who are not candidates for CPAP.
Pharmacotherapy for insomnia with antipsychotic medications alone might improve sleep and psychotic symptoms. Antipsychotic medications have been shown to increase total sleep time and decrease sleep latency and awakenings. Hence, olanzapine, clozapine, chlorpromazine, quetiapine, and asenapine, the more sedating atypical medications, are more frequently used when sedation is a desirable side effect. However, care should be taken to avoid other untoward effects, such as cognitive decline and increased risk of falls.
Melatonin has been shown to improve sleep in patients with schizophrenia. It might increase sleep efficiency, decrease awakenings, reduce sleep latency, and increase total sleep time. An added advantage of melatonin is that it might diminish antipsychotic- induced metabolic effects.28
Tables 2 and 3 summarize the relationship between insomnia and psychotic disorders.
Insomnia and Anxiety Disorders
Insomnia is the most common sleep disturbance associated with anxiety disorders. Poor sleep quality is seen in adults with anxiety disorders.29 Nocturnal panic occurs frequently in patients with sleep apnea and might predispose patients to developing panic disorders,30 which can also cause insomnia. A thorough assessment of sleep difficulties should should be undertaken during clinical evaluation of patients with anxiety symptoms.
Separation anxiety disorder. Separation anxiety disorder is characterized by developmentally inappropriate fear or anxiety regarding separation from home or an attachment figure. It usually occurs in childhood and is rarely seen beyond adolescence. Sleep problems form part of the criteria for the diagnosis of separation anxiety disorder in the DSM-5.31 The individual might show a persistent reluctance or refusal to sleep away from home or to go to sleep without being near a major attachment figure. The individual might also experience repeated nightmares involving the theme of separation. Sleep onset might be disturbed in these patients by unusual perceptual experiences while alone in the dark, such as seeing people peering into their room who aren’t there or imagining the presence of frightening creatures reaching for them or staring at them (Table 4).32
Panic disorder. Patients with panic disorder suffer from recurrent unexpected panic attacks. Panic attacks are abrupt surges of intense fear or discomfort that become intense within minutes. Overbeek et al37 studied prevalence of sleep complaints in 70 patients with panic disorder (PD), comparing them with sleep complaints in 70 healthy controls. Patients with PD demonstrated a higher prevalence of insomnia than normal controls.37 Potvin et al, in a random sample of 2,393 individuals aged 65?years or older, found that anxiety disorder, like panic disorder, was related to short sleep duration, daytime sleepiness, and sleep disturbances.38
Phobias. Specific phobia. Specific phobia is the fear or anxiety about a specific situation or object (e.g., flying, heights, animals). It usually starts prior to the age of 10, the median age of onset being 7 to 10 years. It has a waxing and waning course, and, if it persists into adulthood, remission is rare.
Patients with a specific phobia have problems with sleep latency, sleep quality, and daytime functioning, even after accounting for age, sex, marital status, education, and past-month mood or substance use disorder.33
Social anxiety disorder (social phobia). Social anxiety disorder is a marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others. The majority of children who develop the disorder do so between the ages of 8 and 15, with a median age of 13.
Studies have found that insomnia occurs in up to two-thirds of patients with social anxiety. Patients with social phobia also tend to have poorer sleep quality, increased sleep latency, more sleep disturbances, and altered daytime functioning than healthy controls.34,35 Sleep difficulties also predict the severity of the social anxiety disorder.36
Agoraphobia. Agoraphobia is marked fear or anxiety about real or anticipated exposure to situations, such as use of public transportations, being in open or enclosed spaces, being in a crowd, or being outside the home alone. The sleep profile in agoraphobia mirrors what is seen in patients with panic disorder.
Generalized anxiety disorder (GAD). GAD is characterized by excessive anxiety and worry (apprehensive expectation) about a number of events or activities. Sleep disturbance is one of the DSM-5 diagnostic criteria for GAD. Symptoms include sleep disturbance, difficulty falling asleep or staying asleep, and restless, unsatisfying sleep.31
Ohayon et al39 conducted an epidemiological study on insomnia complaints in 5,622 subjects and found that insomnia symptoms were reported by 18.6 percent of the sample. An anxiety disorder diagnosis was given to 33.1 percent of those who reported insomnia. GAD was seen in about half the cases who were diagnosed with an anxiety disorder. In an earlier study by Ohayon et al of the French population,40 researchers found that GAD was the most prevalent psychiatric diagnosis among subjects reporting insomnia. Alfano et al,41 in a study of 30 nonmedicated, pre-pubescent children (ages 7–11 years), of which 15 had GAD and 15 were healthy controls, researchers used polysomnography (PSG) and found that children with GAD showed significantly increased sleep onset latency. Monti and Monti,42 in a review of polysomnographic studies involving patients with GAD, found that sleep disturbance associated with mild-to-moderate GAD was sleep-maintenance insomnia and, to a lesser extent, sleep-onset insomnia. Most of the studies reported a decrease in total sleep time (TST). Four out of six studies reported an increase in waking after sleep onset (WASO).43
Clinical Implications. Insomnia is common in patients with various anxiety disorders. Insomnia can be a presenting complaint is patients with GAD. Insomnia is seen in studies using both subjective and objective testing, such as polysomnography.
Insomnia and Attention Deficit Hyperactivity Disorder (ADHD)
Some children with ADHD might have sleep-onset insomnia; others might have a predilection for delayed sleep onset but otherwise sleep well. Medications used to treat ADHD can contribute to sleep disturbances. Sleep disorders, such as obstructive sleep apnea (OSA) and restless legs syndrome, lead to sleep disruption and thereby can contribute to the symptoms of ADHD. These disorders might also present with ADHD-like symptoms. These sleep problems and disorders affect the quality of life of children and adolescents with ADHD, with potential adverse effects on learning and memory processing. It is recommended that all children with ADHD be evaluated for sleep problems and primary sleep disorders. These children should also be treated for comorbid sleep problems and disorders, preferably with nonpharmacological behavioral interventions before or concurrent with treatment of ADHD. Long-acting stimulants might also be more beneficial than short-acting stimulants to prevent sleep disturbances.43
Insomnia and Substance Abuse
A complex bidirectional relationship exists between insomnia and substances of abuse. Substances of abuse produce their effects by acting on various receptors and neurotransmitter systems, some of which are involved in normal sleep regulation. Prevalence of insomnia is higher in patients with substance use disorders.44 Mahfoud et al45 found the prevalence of insomnia to be three times higher in individuals with substance abuse disorder. Insomnia has also been shown to predispose to individuals to substance use disorder. Alcohol is the most commonly used sleep aid. People with insomnia are twice as likely to develop alcohol-related problems than those without insomnia. Patients with substance use disorder are more susceptible to effects of sleep deprivation. Rates of insomnia range from 36 to 91 percent in patients admitted for treatment of alcoholism. Insomnia can persist for many weeks or months after abstinence from alcohol. Persistent insomnia can lead to relapse. This is often not recognized by substance abuse treatment programs. Incorporating strategies to help with insomnia can lead to relapse prevention. Cognitive behavior therapy for insomnia (CBTi) can help patients with substance use disorders but might need to be modified to achieve desired effects. Patients with substance use might respond differentially to CBTi. Pharmacological strategies include trazodone, gabapentin, and melatonin. Gabapentin has also shown to decrease risk of relapse in patients with alcohol use disorder.46
Summary
Clinicians should evaluate their psychiatric patients for sleep problems. They should also evaluate their patients who present with complaints of insomnia for comorbid psychiatric problems. Clinicians should query their patients about the quantity and quality of sleep and, daytime somnolence/ hypersomnia, as well as screen for initial, middle, and terminal insomnia. Circadian rhythm disruptions might also be present and should be assessed. Insomnia presentation is of particular clinical importance among patients with comorbid psychiatric disorders. A comprehensive history should include caffeine and alcohol/drug use; level of physical activity; presence comorbid psychiatric symptoms, psychosocial stressors, medical conditions, and medications; and overall sleep hygiene. A physical examination that includes height, weight, and description of body habitus is also recommended. Screening questionnaires, such as the Epworth Sleepiness Scale (ESS) (eight questions),47 the Insomnia Severity Index (ISI) (seven questions),48 and the Berlin Questionnaire (10 questions),49 might aid in the detection of sleep problems, and multiple such instruments are available, Polysomnography and other more intensive and costly examinations are useful in making definitive diagnoses of various primary sleep disorders, such as OSA, and should be reserved for patients who are suspected of having such disorders.
As an initial step in treatment, medical conditions that might contribute to the sleep dysfunction should be assessed. Multiple medical conditions can cause sleep and circadian disturbances, including nasal and sinus allergies, hypothyroidism and hyperthyroidism, coronary artery disease, congestive heart failure, diabetes, arthritis, asthma, gastroesophageal reflux disease, and chronic pain.
CBTi is the preferred treatment for insomnia.51 Internet-based CBTi is also an option because in-person CBTi might not be readily available.50 Sleep promoting medications can be used alone or concomitantly with CBTi, usually for short-term treatment of few weeks.
References
- Walsh JK, Engelhardt CL. The direct economic costs of insomnia in the United States for 1995. Sleep. 1999;22 Suppl 2:S386–93.
- Wickwire EM, Shaya FT, Scharf SM. Health economics of insomnia treatments: Is there a return on investment for good night’s sleep? Sleep Medicine Reviews (2015), doi:10.1016/j.smrv.2015.11.004
- Morin CM, Benca R. Chronic Insomnia. Lancet. 2012;379:1129–41
- Lynne Lamberg. Manual updates sleep disorders diagnoses. Psychiatric News, August 14, 2014.
- Daley M, Morin CM, LeBlanc M, et al. The economic burden of Insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms and good sleepers. Sleep. 2009;32:55–64.
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97-111.
- Benca RM. Consequences of insomnia and its therapies. J Clin Psychiatry. 2001;62(suppl 10):33–38.
- Espana RA, Scammell TE. Sleep neurobiology from a clinical perspective. Sleep. 2011;34(7): 845–858.
- Riemann D, Spiegelhandler K, Feige B, et al. The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Med Reviews. 2010;14:19–31.
- Patient health questionnaire. www.phqscreeners.com
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 134(4):382–89.
- Gerber PD, Barrett JE, Barrett JA, et al. The relationship of presenting physical complaints to depressive symptoms in primary care patients. J Gen Intern Med. 1992;7(2):170–3.
- Ford DE, Kamerow DB. Epidemiological study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–84.
- Khurshid KA, et al. Poster presented at APA Institute of Psychiatry, 2011
- Ettensohn M, Soto Y, Bassi B, Khurshid KA. Sleep problems and disorders in patients with depression. Psychiatric Annals. 2016;46(7):390–5.
- Chang PP, Ford DE, Mead LA, et al. Insomnia in young men and subsequent depression: The Johns Hopkins precursors study. Am J Epidemiology. 1997;146:105–14.
- Agargun MY, Kara Hand Solmaz M. Sleep disturbances and suicidal behavior in patients with major depression. J Clin Psychiatry. 1997;58(6): 249–51.
- Thase ME. Depression, sleep, and antidepressants. J Clin Psychiatry. 1998;59 suppl 4:55–65.
- Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10(4):473–81.
- Manber R, Edinger JD, Gress JL, et al. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid MDD and insomnia. Sleep. 2008;31(4):489–95.
- Chouinard S, Poulin J, Stip E, Godbout R. Sleep in untreated patients with schizophrenia: a meta-analysis. Schizophr Bull. 2004;30:957–967.
- Benson KL. Sleep in schizophrenia: impairments, correlates, and treatment. Psychiatry Clin North Am. 2006;29:1033–1045.
- Keshavan MS, Diwadkar VA, Montrose, DM, et al. Premorbid characterization in schizophrenia: The Pittsburgh High Risk Study. World Psychiatry. 2004;3:163–168.
- Haffmans PM, Hoencamp E, Knegtering HJ, van Heycop ten Ham BF. Sleep disturbance in schizophrenia. Br J Psychiatry. 1994;165: 697–698.
- Karatsoreos IN. Links between circadian rhythms and psychiatric disease. Front Behav Neurosci. 2014;8:162.
- Monti JM, BaHamman AS, Pandi-Perumal SR, et al. Sleep and circadian rhythm dysregulation in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2013;43:209–216.
- Holbert RC, Khurshid KA, Averbuch R, Khawaja IS. Sleep and schizophrenia. Psychiatric Annals. 2016;46(3):192–196.
- Simon EK, Berki ZHK, Getys GC, Vedak C. Sleep problems and disorders in patients with anxiety disorders. Psychiatric Annals. 2016;46(7):396–400.
- Su VY, Chen YT, Lin WC, et al. Sleep apnea and risk of panic disorder. Ann Fam Med. 2015;13(4):325–330.
- DSM-5. Diagnostic and Statistical manual of mental disorders. American Psychiatric Association, 2016
- Anxiety Disorders. In: Diagnostic and Statistical Manual of Mental Disorders. DSM Library. American Psychiatric Association; 2013.
- Ramsawh HJ, Stein MB, Belik S-L, et al. Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. J Psychiatr Res. 2009;43(10):926–933.
- Raffray T, Bond TLY, Pelissolo A. Correlates of insomnia in patients with social phobia: role of depression and anxiety. Psychiatry Res. 2011;189(2):315–317.
- Stein MB, Kroft CD, Walker JR. Sleep impairment in patients with social phobia. Psychiatry Res. 1993;49(3):251–256.
- Kushnir J, Marom S, Mazar M, et al. The link between social anxiety disorder, treatment outcome, and sleep difficulties among patients receiving cognitive behavioral group therapy. Sleep Med. 2014;15(5): 515–521.
- Overbeek T, van Diest R, Schruers K, et al. Sleep complaints in panic disorder patients. J Nerv Ment Dis. 2005;193(7):488–493.
- Potvin O, Lorrain D, Belleville G, et al. Subjective sleep characteristics associated with anxiety and depression in older adults: a population-based study. Int J Geriatr Psychiatry. 2014;29(12):1262–1270.
- 39. Ohayon MM, Lemoine P. A connection between insomnia and psychiatric disorders in the French general population. L’Encéphale. 2002;28(5 Pt 1):420–428.
- Ohayon MM. Prevalence of DSM-IV diagnostic criteria of insomnia: Distinguishing insomnia related to mental disorders from sleep disorders. J Psychiatr Res. 1997;31(3):333–346.
- Alfano CA, Reynolds K, Scott N, et al. Polysomnographic sleep patterns of non-depressed, non-medicated children with generalized anxiety disorder. J Affect Disord. 2013;147(1-3):379–384.
- Monti JM, Monti D. Sleep disturbance in generalized anxiety disorder and its treatment. Sleep Med Rev. 2000;4(3):263–276. http://www.sciencedirect.com/science/article/pii/S1087079299900965. Accessed July 16, 2015.
- Ramnaraine LD, Rahmani M, Khurshid KA. Sleep problems and disorders in children and adolescents with attention-deficit/ hyperactivity disorder. Psychiatric Annals. 2016;46(7):401–407.
- Ara A, Jacobs W, Bhat IA, McCall WV. Sleep disturbances and substance use disorders: a bi-directional relationship. Psychiatric Annals. 2016;46(7):408–412.
- Mahfoud Y, Talih F, Streem D, Budur K. Sleep disorders is substance abusers: how common are they? Psychiatry (Edgmont). 2009;6(9):38–42.
- Gentry JR, Hill C, Malcolm R. New anticonvulsants:a review of applications for the management of substance abuse disorders. Ann Clin Psychiatry. 2002;14(4): 233–245.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540–5.
- Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–8.
- Netzer NC, Stoohs RA, Netzer CM, et al. Using Berlin questionnaireto identify patients at risk for sleep apnea syndrome. Ann Intern Med. 1999;131:485–491.
- Seyffert M, Lagisetty P, Landgraf J, et al. Internet-delivered cognitive behavioral therapy to treat insomnia: a systematic review and meta-analysis. PLoS One. 2016;11(2):e0149139. eCollection 2016.





