 by Ahmed Aboraya, MD, DrPh; Henry Nasrallah, MD; Srinivas Muvvala, MD, MPH; Ahmed El-Missiry, MD, MRCPsych, IFAPA; Hader Mansour, MD, PhD; Cheryl Hill, MD PhD; Daniel Elswick, MD; and Elizabeth C. Price, PhD
by Ahmed Aboraya, MD, DrPh; Henry Nasrallah, MD; Srinivas Muvvala, MD, MPH; Ahmed El-Missiry, MD, MRCPsych, IFAPA; Hader Mansour, MD, PhD; Cheryl Hill, MD PhD; Daniel Elswick, MD; and Elizabeth C. Price, PhD
Dr. Aboraya is Chief of Psychiatry at William R. Sharpe Jr. Hospital, Clinical Professor of Psychiatry at West Virginia School of Osteopathic Medicine in Lewisburg, West Virginia, and Adjunct Faculty in the School of Public Health at West Virginia University in Morgantown, West Virginia; Dr. Nasrallah is with the Department of Psychiatry and Behavioral Neuroscience, Saint Louis University School of Medicine, St. Louis, Missouri; Dr. Muvvala is with Yale University, New Haven, Connecticut; Dr. El-Missiry is Professor of Psychiatry at Ain Shams University in Cairo, Egypt; Dr. Mansour is Assistant Professor of Psychiatry, Medical Director, Addiction Medicine Services Inpatient Unit at Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania; Dr. Hill is Assistant Professor, Department of Behavioral Medicine and Psychiatry at West Virginia University, Morgantown, West Virginia; Dr. Elswick is with West Virginia University in Morgantown, West Virginia; and Dr. Price is with the Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey VA Medical Center in Houston, Texas.
Innov Clin Neurosci. 2016;13(5–6):31–77.
Funding: No funding was received for the preparation of this article.
Financial Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Psychiatric interview, descriptive psychopathology, dimensional scores, diagnostic criteria, standardized diagnostic interviews, Standard for Clinicians’ Interview in Psychiatry, SCIP
Abstract: Existing standardized diagnostic interviews (SDIs) were designed for researchers and produce mainly categorical diagnoses. There is an urgent need for a clinician-administered tool that produces dimensional measures, in addition to categorical diagnoses. The Standard for Clinicians’ Interview in Psychiatry (SCIP) is a method of assessment of psychopathology for adults. It is designed to be administered by clinicians and includes the SCIP manual and the SCIP interview. Clinicians use the SCIP questions and rate the responses according to the SCIP manual rules. Clinicians use the patient’s responses to questions, observe the patient’s behaviors and make the final rating of the various signs and symptoms assessed.
The SCIP method of psychiatric assessment has three components: 1) the SCIP interview (dimensional) component, 2) the etiological component, and 3) the disorder classification component. The SCIP produces three main categories of clinical data: 1) a diagnostic classification of psychiatric disorders, 2) dimensional scores, and 3) numeric data. The SCIP provides diagnoses consistent with criteria from editions of the Diagnostic and Statistical Manual (DSM) and International Classification of Disease (ICD). The SCIP produces 18 dimensional measures for key psychiatric signs or symptoms: anxiety, posttraumatic stress, obsessions, compulsions, depression, mania, suicidality, suicidal behavior, delusions, hallucinations, agitation, disorganized behavior, negativity, catatonia, alcohol addiction, drug addiction, attention, and hyperactivity. The SCIP produces numeric severity data for use in either clinical care or research. The SCIP was shown to be a valid and reliable assessment tool, and the validity and reliability results were published in 2014 and 2015. The SCIP is compatible with personalized psychiatry research and is in line with the Research Domain Criteria framework.
Historical Perspectives on the Assessment of Psychopathology
The history of mental illness and description of mental symptoms are closely intertwined with the social history of humankind. Descriptions of individuals with “strange,” “maladaptive,” or “dangerous” behaviors have been documented in some of the first known written records.[1] The descriptions of King Saul’s homicidal and suicidal thoughts in the Old Testament (in about 1,000 B.C.) point to the presence of extreme mood disorder. Greek philosophers, including Plato, Aristotle, and Hippocrates, described various forms of madness—mania, hysteria, paranoia, melancholia, and dementia. It is striking that prior to the 19th century, the subjective experiences of the patients were not valued and there was no real descriptive psychopathology. The great diagnostic categories inherited by the 19th century, such as melancholia, mania, delirium, dementia, and paranoia, relied on the observation of what the individual did, looked like, and said, rather than on how the individual felt.[2]
The science of mental symptoms and signs (descriptive psychopathology) was developed in Europe in the 19th century, and the science of classification of mental disorders (psychiatric nosology) proceeded to advance significantly in the 20th century. At the beginning of 19th century, the science of mental symptoms started to develop in Europe and has taken about 100 years to complete. The incorporation of subjective experiences of the patients into the symptom repertoire of psychopathology was a significant achievement of the science of descriptive psychopathology in the 19th century.[2] Patients’ subjective feelings of anxiety, mood, melancholia, mania, paranoia, hallucinations, and other mental symptoms were described, analyzed, and classified.[2] The advances in the science of mental symptoms in the 19th century paved the way for the development of psychiatric nosology in the twentieth century.
At the turn of the 20th century, Kraepelin conceptualized his famous “dichotomy theory” that divided the “insanities” broadly into two diseases: dementia praecox (later renamed schizophrenia by Eugen Bleuler) and manic-depressive illness (later renamed bipolar disorder by Karl Kleist).[3] His classification model was enshrined in Western psychiatry for more than a century, even though Kraepelin himself revised his theory in 1920.[3] In 1933, Jacob Kasanin coined the term schizoaffective to describe patients with equal measure of co-existing psychotic and manic and/or depressive symptoms.[4] As an example of the beginning of advancement in psychiatric nosology, a survey conducted in 1936 in the Eastern Health District of Baltimore by Paul Lemkau[5] described several types of psychosis, including schizophrenia, manic-depressive, involutional, senile and arteriosclerotic, alcoholic, syphilitic, with epilepsy, with mental deficiency. The same survey described the following types of psychoneurosis: hysteria, psychasthenia, neurasthenia, hypochondriasis, reactive depression, anxiety attacks, and mixed psychoneurosis.[5] When psychoanalysis dominated American psychiatry, psychiatric nosology was put on the back burner for decades because psychoanalysts had always believed that psychiatric diagnosis was largely irrelevant for making psychotherapy treatment decisions.[6],[7]
In the beginning of the second half of the 20th century, psychiatric nosology started to expand gradually due to the efforts of the World Health Organization (WHO) and the American Psychiatric Association (APA). The World Health Organization (WHO) published the sixth revision of the International Classification of Diseases (ICD-6) in 1948, which included a mental disorders section.[8] Several editions of the ICD followed, including the 10th (and latest), published in 1993.[9] In the United States, the American Psychiatric Association Committee on Nomenclature and Statistics developed and published the first edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-I) in 1952, followed by the DSM-II in 1968.[10],[11] A major paradigm shift in psychiatric nosology in the 20th century was achieved in 1980 with the publication of the DSM-III.[12] The publication of the DSM-III represented a turning point in the history of psychiatric nosology because it included the long-awaited, detailed, explicit, and specific criteria for many psychiatric disorders.13 Revisions of the DSM-III continued with the publications of the DSM-III-Revised (R), DSM-IV, DSM-IV-Text Revision (TR), and the DSM-5.[14–17] The DSM-5, though mainly categorical in its classification, has promoted cross-cutting symptom measures and has reordered diagnoses to stimulate new clinical perspectives.
Because the DSM-III provided psychiatrists with a standardized diagnostic nomenclature, their enterprises flourished, and investigative psychiatrists collaborated with geneticists, pharmacologists, and brain imagers.[7] The advances in psychiatric nosology have resulted in the development of systematic instruments to assess and measure psychiatric symptoms and evaluate the diagnostic criteria of mental disorders. Rating scales, designed to quantify symptoms, included the Positive and Negative Syndrome Scale (PANSS), Brief Psychiatric Rating Scale (BPRS), Hamilton Rating Scale for Depression (HAM-D), Yale-Brown Obsessive Compulsive Scale (Y-BOCS) and others.18–21 However, rating scales focus on narrow clusters of symptoms that do not necessarily incorporate details of the entire clinical picture and have not been shown to have the same predictive utility as diagnoses.[22] Rating scales are mostly used by research psychiatrists and psychologists, while the vast majority of psychiatric practitioners rarely use them in clinical practice.
In addition to rating scales, Standardized Diagnostic Interviews (SDIs) were developed with the main goal of arriving at a diagnosis based on the existing classification systems. Some SDIs, such as the World Health Organization Composite International Diagnostic Interview (CIDI) and the Mini-International Neuropsychiatric Interview (M.I.N.I.), are fully structured.[23],[24] For clinicians, semi-structured interviews were designed to allow for considerable variation in the interviewing style, depth of probing, and clinical judgment as to whether a patient’s description of a particular behavior meets the relevant diagnostic criterion.[25] Two widely used semi-structured interviews in the assessment literature are the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Schedules for Clinical Assessment in Neuropsychiatry (SCAN).[25–27]
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) was designed with a top-down approach: questions are grouped by diagnosis and criteria; within each diagnosis, if a required criterion is not met, the interviewer skips the remaining questions assessing the other criteria for that diagnosis. The SCID-I authors claimed that the SCID-I was more “clinician-friendly” than the other structured diagnostic instruments.[26] Many SCID-I users, (including the authors), can make a case that the SCID-I tends to be lengthy and cumbersome and may interfere with establishing rapport with patients. Realizing that the SCID-I was not as clinician-friendly as they first claimed, the SCID-I authors subsequently published the SCID-Clinical Version (SCID-CV) in 1997. This modified version of the SCID-I includes only the DSM-IV diagnoses most commonly seen in clinical practice.[28] The SCID-CV is simply an abbreviation of the original SCID-I, and in our opinion is not compatible with clinicians’ style of interviewing and has not been adopted by clinicians in real practice.
The Schedules for Clinical Assessment in Neuropsychiatry (SCAN) is another semi-structured interview developed under the auspices of the World Health Organization (WHO). It utilizes the bottom-up approach: after comprehensive baseline symptom assessment, algorithms are used to make psychiatric diagnoses.[27] Similar to the SCID-I, the SCAN is lengthy, cumbersome, and requires extensive training. For these reasons, FJ Nienhuis, a member of the SCAN Advisory Committee, devised a shorter version of the SCAN (mini-SCAN) to promote the clinical use of the SCAN.[29] The mini-SCAN simplifies the symptom severity rating into absent or subclinical (0) and symptom level (1) and diagnoses only current episodes. The Mini-International Neuropsychiatric Interview (M.I.N.I.) was developed by DL Sheehan as a short, structured diagnostic interview.[24] However, as the M.I.N.I. covers more disorders, it takes a longer time to administer (45 minutes or longer for M.I.N.I.-Plus Version). Overall, the M.I.N.I. is simpler and shorter than the SCID-I and the SCAN and has some acceptance in clinical settings.[30] On the downside, the M.I.N.I. is simply a checklist of symptoms, and the clinical approaches of probing and exploring the symptoms are largely lost.[29]
Considering the most popular existing standardized diagnostic interviews (SDIs) and the efforts to modify them for clinicians’ use, two facts stand out. First, the existing instruments were primarily designed for researchers. None was designed from the outset for clinicians to use in real clinical practice. Second, not surprisingly, the literature indicates that clinicians do not use structured interviews or rating scales in real clinical settings.[30–37] One survey of mental health practitioners found that 98 percent did not use any of the four clinical rating scales routinely used in pivotal clinical trials required for the United States Food and Drug Administration’s approval of new psychotropic medications. These rating scales are the PANSS, Young Mania Rating Scale (YMRS),[38] HAM-D, and Montgomery-Asberg Depression Rating Scale (MADRS).[39] Lack of time was the most common reason cited for not using these tools.[37] In another survey, 72.5 percent of psychiatrists said that they do not use structured interviews in clinical settings.30 The three most commonly cited reasons for not using structured interviews were constraints on time, the perception and reality that structured interviews are research tools, and that structured interviews interfere with establishing rapport with patients.[30] Considering these serious gaps in the literature, namely the lack of an instrument designed for psychiatrists to use in clinical settings and the lack of a clinician-administered tool with dimensional measures, the first author of this article (AA) devised the Standard for Clinicians’ Interview in Psychiatry (SCIP). The SCIP was shown to be a valid and reliable diagnostic interview.[40,41]
The Design Features of the SCIP
Bottom First Then Top: the SCIP approach to psychiatric diagnosis. Two approaches to psychiatric diagnosis have been described in the literature: the “top-down” approach and the “bottom-up” approach. The advantages and disadvantages of each have been described elsewhere.[26],[27],[42–44] In the top-down approach, exemplified by the SCID-I, questions are grouped by diagnosis and criteria; within each diagnosis, if a required criterion is not met, the interviewer skips the remaining questions assessing the other criteria for that diagnosis. For example, if the patient denies depressed mood and anhedonia, the SCID-I instructs the interviewer to skip the remaining questions for the diagnosis of major depression.[26] The top-down approach leads to efficient interviews by focusing on diagnoses, facilitates clinical communication, and improves reliability. On the other hand, diagnostic interviews based upon the top-down approach tend to be biased toward preconceived diagnostic criteria, lack validity, may result in loss of important information, and need to be updated every time the diagnostic system changes. With the publications of DSM-5 in May 2013, the SCID-I requires major changes to be compatible with the new DSM-5 diagnoses criteria. Using the bottom-up approach, as exemplified by the SCAN, the interview is based upon a comprehensive assessment of symptoms, while being agnostic to diagnosis.[27] After symptoms assessment, algorithms are used to make psychiatric diagnoses. The bottom-up approach has the advantages of avoiding biases toward preconceived diagnoses and can survive diagnostic criteria changes. However, the bottom-up approach leads to lengthy interviews and may lack the precision needed to fulfill diagnostic criteria.[44]
Seasoned and competent psychiatrists generally use the Bottom First Then Top (BFTT) approach, a term coined by the first author (AA), in diagnostic assessment. An ideal diagnostic psychiatric interview starts with a bottom-up approach: the psychiatrist establishes rapport with the patient and inquires about chief complaint(s) and history of the present illness. The patient is initially allowed to take the lead to express feelings, thoughts, current stressors, and other problems. The psychiatrist continues the bottom-up approach by obtaining a detailed life history, screening for symptoms, examining mental status, exploring potential causes of symptoms, and utilizing records and informants as needed. As the psychiatrist narrows down the potential differential diagnoses, the top-down approach takes over the interview process. The psychiatrist checks the symptoms and decides whether the patient meets the diagnostic criteria of a disorder. The SCIP reflects the BFTT approach of psychiatric assessment through its three components: the SCIP interview component and the etiological component are mainly bottom-up approaches. The disorders classification component is mainly a top-down approach. The mission of the BFTT approach is to listen to and understand the patient first and then focus on making a diagnosis. The SCIP Instruction Manual explains the three components of the SCIP. Another term proposed to this approach is Patient First Then Clinician (PFTC) highlighting the importance of listening and understanding the patient first before making a diagnosis.
Phases of development of the SCIP. Initial phase. Between the years 2000 and 2004, the SCIP questions were developed, phrased, rephrased, and changed to fit the actual clinical interviews conducted by psychiatrists. The first 110 SCIP interviews included demographic and screening data. The rest of the SCIP interviews included demographic, screening, and modular data. Validity and reliability testing phase. The validity of the SCIP was tested by comparing the diagnoses generated by the SCIP method against the diagnoses generated by the SCAN interview and the diagnoses provided by experts (both were considered to be gold standard diagnoses). The reliability of the SCIP was tested using the Kappa mehtod for inter-rater reliability and Cronbach’s alpha method for internal consistency.
Multi-site phase. Two sites in Egypt (Mansoura University and Ain Shams University) and one site in Toronto (Rothbart Center) joined the project.
Unique Features of the SCIP. The SCIP was designed and tailored from the outset to serve the clinicians’ needs in clinical settings, whether inpatient or outpatient. The SCIP is a standard guide to clinicians’ diagnostic interviews, and hence the name: the Standard for Clinicians’ Interview in Psychiatry (SCIP).
The SCIP allows clinicians the full freedom to administer the interview as they see fit. The SCIP interview starts with the Screening Section followed by the Modular Section. The SCIP Screening Section has questions on anxiety, mood, psychosis, alcohol and substance, somatoform, eating, attention, and hyperactivity. The clinician can start with questions that he or she finds most appropriate. The clinician decides on the episode period that he/she evaluates. After the Screening Section, the clinician chooses the module(s) needed to make the appropriate diagnosis(es). If the clinician decides to explore two or more modules, he or she can start with any module deemed appropriate. There is no structured or semi-structured interview currently available that allows such freedom for the clinician, simply because the SCIP utilizes the full extent of clinicians’ expertise in conducting diagnostic interviews. No structured or semi-structured tool can ever replace the clinicians’ skills.
The SCIP was designed to produce three types of output: 1) numeric data for symptoms/signs and their severity, 2) dimensional scores for clusters of symptoms (anxiety, posttraumatic stress, obsessions, compulsions, depression, mania, suicidality, suicidal behavior, delusions, hallucinations, agitation, disorganized behavior, negative symptoms, catatonia, alcohol addiction, drug addiction, attention problems, and hyperactivity), and 3) disorder categories according to the to the DSM-5 (and later editions) and ICD-10 (and later editions) criteria.
The building blocks of the SCIP are the enduring symptoms and signs of psychopathology that do not change over time. Whether we have the ICD-10 or beyond, the DSM-5 or beyond, the phenomenology of mental disorders remains unchanged and the SCIP will withstand future diagnostic criteria changes. For example, although the SCIP was developed and tested before the DSM-5 publication in 2013, the SCIP contains the main criteria needed to make the diagnosis of the new DSM-5 disruptive mood dysregulation disorder (irritable mood, verbal and physical aggression, manic and hypomanic episode). The clinician inquires about the frequency, duration, and onset of temper outbursts and decides whether the patient meets the criteria for the diagnosis of disruptive mood dysregulation disorder.
The SCIP transforms routine clinical information into research data when needed. Psychiatrists evaluate thousands of patients daily. The multitudes of records produced, such as psychiatric evaluations and progress notes, have mainly one primary use—clinical management—as well as several secondary uses—billing, legal issues and research. The SCIP retains the clinical management function and also produces data that can be gleaned for research. If all psychiatric interviews can be seamlessly transformed into research data, the potential value for scientific inquiry would be highly significant.
Design of the SCIP questions and observational items
Symptoms of psychopathology. As in the case of medicine, modern psychiatric diagnosis depends on the assessment of psychopathological symptoms and signs. The SCIP interview reflects the “state-of-the-art” assessment of psychopathology and includes questions designed to evaluate symptoms and observational items for the signs of mental illness. The SCIP questions were designed and worded to be simple and easily understood by patients, regardless of their intellectual level. The meaning of the questions and examples were embedded in the questions so that each question and the response reflect the criterion being examined. The DSM set the criteria, but never set how to measure them. For example, one of the criteria of major depressive episode is “diminished ability to think or concentrate.” Here is the SCIP question and responses:
MB7. Diminished concentration.
Have you found that your concentration has decreased and you are unable to complete a task (e.g., at work, reading an article, reading a book, watching a movie), even though you were able to do that before? 0=Patient has no concentration problems 1=Patient has difficulty concentrating less than half the time 2=Patient has difficulty concentrating more than half the time
The question and responses explain the criterion, give examples of impaired concentration, and measure the severity (less than half the time or more than half the time).
Signs of psychopathology. The SCIP interview includes observational items to assess for signs of mental illness. The signs are defined and described. The interviewer observes and examines the patient and decides on the presence or absence of the sign assessed.
MC21. Derailment.
1. Patient has derailment (looseness of association): speech shifts to different topics, related or unrelated, but eventually comes back to the main topic
2. Patient has severe derailment (severe looseness of association): speech shifts to different topics, mostly unrelated, and never comes back to main topic
Questions with built-in dimensional capabilities. The SCIP questions were designed so that dimensional measures can be generated easily whether the interviewer is using the paper version or the SCIP software. For example, obsession questions cover how many hours per day obsessions occur, how many days per week obsessions occur, and the types of obsessions. Answers to the questions sum to the total dimensional score for obsessions.
OCD1. Do you have an intrusive thought or image that does not make sense and keeps coming back to your mind even when you try not to have the thought or the image?
0=Patient has no obsessions.
1=Patient has obsessions less than 1 hour/day.
2=Patient has obsessions 1 to 4 hours/day.
3=Patient has obsessions more than four hours/day.
OCD2. During a one week period, how many days do you have obsessive thoughts on the average (# of days from 0 to 7)?
OCD3. Aggressive obsessions.
0=Patient has no aggressive obsessions.
1=Patient has aggressive obsessions.
OCD4. Contamination obsessions (e.g., dirt, germs)
0=Patient has no contamination obsessions
1=Patient has contamination obsessions
OCD5. Sexual obsessions.
0=Patient has no sexual obsessions
1=Patient has sexual obsessions
OCD6. Religious obsessions.
0=Patient has no religious obsessions
1=Patient has religious obsessions
OCD7. Somatic obsessions. (concerned with disease)
0=Patient has no somatic obsessions
1=Patient has somatic obsessions
OCD8. Appearance obsessions.
0=Patient has no appearance obsessions
1=Patient has appearance obsessions
OCD9. Other obsessions.
0=Patient has no other obsessions
1=Patient has other obsessions
Description and Uses of the SCIP The SCIP materials.
The materials for the SCIP method of psychiatric assessment include the SCIP interview and the SCIP instruction manual. The SCIP interview contains approximately 230 questions and observational items, including 29 screening questions. The SCIP questions and observational items cover almost every human emotional complaint, symptom, and sign.
The SCIP Interview has four main sections: 1) demographic, social, and history of present illness; 2) screening; 3) medical, family, and psychiatric history; and 4) SCIP modules section.
The SCIP modules section comprises the following:
• Module A1: anxiety, phobia, and panic
• Module A2: obsessive compulsive disorders
• Module A3: posttraumatic stress disorder
• Module B: mood disorders
• Module C: psychotic disorders
• Module D: alcohol and substance use disorders
• Module E: somatic symptom disorders
• Module F: eating disorders
• Module G: attention deficit/hyperactivity disorders
• Module H: adjustment disorders
• Module J: neurocognitive disorders
• Module P: personality disorders.
The 36-page SCIP instruction manual describes the SCIP method for psychiatric assessment, the SCIP rules for rating symptoms and observational items, and the SCIP guidelines for making diagnoses. It is important to note that neither the DSM-III nor its successors specified assessment procedures by which to determine whether criteria are met.35 The SCIP interview and manual fills this gap. Clinicians with extensive experience in mental health can read and implement the SCIP manual guidelines during psychiatric assessment. No training is required for experienced mental health professionals.
Uses of the SCIP. The SCIP is designed to be used in either clinical or research settings.
Clinical use of the SCIP. The SCIP was designed from the outset to reflect what seasoned, competent psychiatrists do in clinical assessment, as described by the BFTT approach. The SCIP can be viewed as a translation of the language experienced psychiatrists use in performing diagnostic psychiatric evaluations. When a psychiatrist performs an assessment, he or she produces several pages of psychiatric evaluation notes. If the psychiatrist uses the SCIP method, he or she produces a psychiatric evaluation and quantitatively measured symptoms and clusters of symptoms.
The SCIP modules can be used in specialty clinics. Clinicians can use Module B in a mood disorder clinic, Module C in a thought disorder clinic, and so on. The use of the SCIP for longitudinal evaluation of patients becomes even more important and more valuable because the clinician can easily track how the dimension score changes over time. For example, the changes in the depression dimension score over time can show the efficacy of antidepressant medications and/or psychotherapy in treating patients with depression.
Research use of the SCIP. The SCIP was designed for research use in addition to clinical use. Because the SCIP questions measure meaningful clinical changes, the SCIP dimensional scores can show whether the patient has made clinically significant improvements. The SCIP screening questions and the SCIP modules can be used in some epidemiological studies depending upon the study questions, goals, design, and other factors.
Users of the SCIP: qualifications and training. Psychiatrists and experienced mental health professionals such as clinical psychologists, clinical social workers, mental health counselors and researchers can use the SCIP. Mental health professionals should A) have at least two years of inpatient or outpatient experience; B) be able to conduct independent diagnostic interviews with patients; C) be very knowledgeable about ICD and DSM diagnostic criteria; and D) be very familiar with the SCIP questions and the SCIP instruction manual. No training is required for experienced mental health professionals.
Psychiatrists have medical skills that enable them to discern the effects of medical conditions on psychiatric presentations. Other mental health professionals who lack medical skills training can use the SCIP. However, in certain conditions where medical problems complicate psychiatric presentations, clinicians without medical training should consult psychiatrists or medical personnel.
Translation of the SCIP. The SCIP was translated first into the Arabic language by two psychiatrists at Mansoura University and Ain Shams University in Egypt. The Arabic SCIP was reviewed by the SCIP author, who is fluent in both English and Arabic, to make sure that the Arabic SCIP was an accurate translation of the original English SCIP. Using a similar process, the SCIP was translated into Spanish, Hindi, and Mandarin by clinicians who were fluent in both English and the translated language. The translated Spanish, Hindi and Mandarin versions of SCIP were reviewed by independent clinicians who were fluent in both English and the translated language to make sure that the translated SCIP was an accurate translation of the original English SCIP. The translation of the SCIP will be updated formally with backward and forward translations.
Output from the SCIP The SCIP produces three types of output: 1) symptoms and observational items along with their severity, 2) dimensional scores for symptom clusters, and 3) psychiatric diagnoses. The SCIP generates the following dimensional scores: anxiety (0–7), posttraumatic stress (0–21), obsessions (0–17), compulsions (0–17), depression (0–38), mania (0–21), suicidality (0–36), suicidal behavior (0–13), delusions (0–23), hallucinations (0–19), disorganized behavior (0–13), agitation (0–11), negative symptoms (0–12), catatonia (0–16), alcohol addiction (0–15), drug addiction (0–13), attention problems (0–12) and hyperactivity (0–12). The SCIP generates the following diagnoses:
• Module A (anxiety disorders): panic disorder, agoraphobia, social phobia, specific phobia, generalized anxiety disorder, obsessive-compulsive disorder, and posttraumatic stress disorder
• Module B (mood disorders): major depression, dysthymia, bipolar I and II, cyclothymia, suicidality, and suicidal behavior
• Module C (psychotic disorders): schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder, and brief psychotic disorder
• Module D (substance use disorders): alcohol and drug use disorders
• Module E: somatic symptom and unspecified somatic symptom disorders
• Module F (eating disorders): anorexia nervosa, bulimia nervosa, and binge-eating disorders
• Module G (attention deficit hyperactivity disorder) •
Module H (adjustment disorders)
• Module J (neurocognitive disorders)
• Module P (personality disorders)
The SCIP study[38],[39] is considered an important study in the psychiatric literature as it has achieved the following:
1. One thousand and four subjects were interviewed in three countries and generated 1,419 SCIP interviews that were used in calculating validity and reliability indices. The SCIP study is the largest validity and reliability study of a diagnostic assessment tool.
2. The SCIP study measured a stable Kappa for 150 symptoms and signs of psychopathology. No other study in the literature has achieved this.
3. The SCIP study measured Cronbach’s alpha for 14 dimensions covering important areas of psychopathology (anxiety, posttraumatic stress, depression, mania, delusions, hallucinations, Schneider’s first-rank symptoms, disorganized thoughts, disorganized behavior, negative symptoms, alcohol addiction, drug addiction, attention problems and hyperactivity).
The SCIP and Future Research
Experimental psychopathology research. Inspired by Berrios’s classification of psychopathology (descriptive, experimental and psychodynamic),[2] psychopathology can be expanded as follows:
• Qualitative psychopathology (descriptive, phenomenological): focus on the form of symptoms. Examples: types of hallucinations (e.g., auditory and visual), types of delusions (e.g., paranoid, somatic, grandiose).
• Quantitative (numerical) psychopathology: assigning numbers to symptoms and signs. Example: duration of auditory hallucination—1=less than one hour, 2=1 to 4 hours, and 3=more than four hours per day. Quantitative psychopathology is useful in measuring severity of symptoms, efficacy of treatment, hypothesis testing, and other research inquiries.
• Etiological psychopathology: focus on the causes of symptoms. Example: Are auditory hallucinations due to PTSD or a brain tumor?
• Experimental psychopathology: the study of the relationship between the psychopathology of an individual and objective measures. Examples: thyroid hormone level, medication blood level, structural imaging (CT, MRI), functional imaging (fMRI), positron emission tomography (PET), single photon emission tomography (SPECT), molecular imaging (magnetic resonance spectroscopy [MRS]), genomics, pharmacogenomics, biomarkers, endophenotypes, epigenetic modifications, genetic variants, translational neuroscience technologies, or any newly developed techniques or blood tests.
Measuring psychopathology reliably at the level of individual symptoms and signs and correlating them with the brain changes in vivo is the best hope to unravel the causes of mental disorders. Uncovering the biological bases of individual symptoms may prove to be as helpful or more helpful than studying constellations of symptoms (syndromes) in order to understand the pathophysiology of the illness.[45] The SCIP measured kappa for 178 symptoms and signs and provided a framework of experimental psychopathology for adult psychiatry. Personalized psychiatry.
Personalized psychiatry is the science of systematic use of individual unique characteristics across four domains: life story, environmental factors, psychopathology assessment, and translational neuroscience findings (e.g. brain imaging, genomics, pharmacogenomics, biomarkers, endophenotypes, or any newly developed technique or blood test) to guide the clinician toward a person-centered diagnosis, person-centered prognosis, person-centered therapeutics (personalized selection and personalized dosing of medications), improving the outcome of the disease, and eventually the prevention of disease.
Individualized psychopathology assessment is one of the core components of personalized psychiatry. The SCIP Descriptive Psychopathology Code (DPC) and Descriptive Psychopathology Map (DPM) form the basis of individualized assessment. The descriptive psychopathology code (DPC) is a comprehensive psychological assessment (symptoms, signs, and dimensions) of an individual at one point in time, conducted by a clinician using the SCIP methodology. Descriptive psychopathology map (DPM). DPM?is two or more descriptive psychopathology codes (DPCs) obtained over time by the same or different clinicians. Characteristics of DPC include the following:
1. The DPC is the equivalent of a fingerprint of the mind of an individual at one point in time.
2. Each individual can have multiple descriptive psychopathology codes (DPCs) as the individual is assessed at different times by the same or a different clinician.
3. The DPC of an individual is constant at one point in time and is dynamic over time as symptoms and signs abate with treatment and new symptoms and signs emerge.
4. If the individual has no symptoms, all of the DPC items are zeroes except for ID#, date of evaluation, date of birth, and sex.
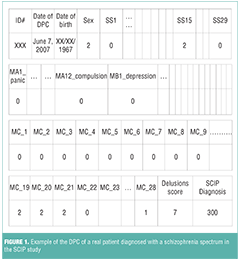
Figure 1 is an example of the DPC of a real patient diagnosed with a schizophrenia spectrum in the SCIP study. If a researcher or a clinician reviewed the DPC of the patient in Figure 1 today, he or she could conclude that on June 7, 2007, the patient was a 40-year-old woman and, upon screening, admitted to having paranoid delusions (SS15=2). The patient had full paranoid, persecutory, and conspiracy delusions (MC19, MC20, and MC21), and her delusions were bizarre (MC28). The patient’s delusions dimension score was 7, and she was diagnosed with schizophrenia spectrum.
Research Domain Criteria (RDoC) framework. The SCIP symptoms, signs, and dimensions are in line with the RDoC framework. The current research depends heavily on the DSM and ICD diagnostic categories, which lack validity and do not create homogeneous populations.[46–50] For example, the DSM-5 diagnostic criteria for schizophrenia spectrum do not identify homogeneous populations, and patients with different presentations satisfy the official criteria. Not surprisingly, decades of research in clinical neuroscience and genetics have failed psychiatry.[51, 52] Consequently, the National Institute of Mental Health (NIMH) initiated the Research Domain Criteria (RDoC) project in 2008. RDoC moves away from the constraints of the DSM/ICD categories and focuses on new ways of classifying mental disorders based on empirical data from genetics, neuroscience, and dimensions of observable behavior.[53],[54] The NIMH workgroup developed a two-dimensional matrix of five major domains of functioning (five rows) and seven units of analysis (seven columns). Symptoms, signs and dimensions are important units of analysis in the matrix. The symptoms, signs and dimensions measured by the SCIP fit well with RDoC. The RDoC project represents a major paradigm shift in psychiatric classification, so researchers and clinicians will experience a major transition (both conceptually and practically) from ICD/DSM categorical systems to the new RDoC.[54] Because the SCIP produces categorical diagnoses in addition to dimensions, the SCIP is positioned to be the right assessment tool in the transition period toward RDoC.
Conclusion
The SCIP is reliable and valid diagnostic interview, is compatible with experimental psychopathology and personalized psychiatry research, and is in line with the NIMH RDoC framework.
The SCIP Instruction Manual is also available for download by visiting https://innovationscns.com/wp-content/uploads/SCIP_Instruction_Manual_2015.pdf.
Acknowledgment
Dr. Aboraya had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses.
References
1. Stone M. Healing the Mind: A History of Psychiatry from Antiquity to the Present. In: Stone M, ed. New York: Norton; 1977.
2. Berrios G. The History of Mental Symptoms: Descriptive Psychopathology Since the Nineteenth Century. Cambridge: Cambridge University Press; 1998.
3. Kraepelin E. Die Erscheinungsformen des Irreseins. Zeitschrift fur die gesamte Neurologie und Psichiatrie. 1920;62:1.
4. Kasanin J. The acute schizoaffective psychoses. 1933. Am J Psychiatry. 1994;151:144–154.
5. Lemkau P. Mental hygiene problems in an urban district, second paper. Mental Hygiene. 1942;26:100–119.
6. Spitzer RL. Values and assumptions in the development of DSM-III and DSM-III-R: an insider’s perspective and a belated response to Sadler, Hulgus, and Agich’s “On values in recent American psychiatric classification”. J Nervous Mental Disease. 2001;189:351–359.
7. McHugh PR. Striving for coherence: psychiatry’s efforts over classification. JAMA. 2005;293:2526–2528.
8. WHO. Manual of the International Classification of Diseases, Injuries and Causes of Death. Geneva: 1948.
9. WHO. The ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research. 10th edition ed. Geneva, Switzerland: World Health Organization; 1993.
10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 1st ed. Washington, DC: American Psychiatric Press Inc.; 1952.
11. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 2nd ed. Washington, DC: American Psychiatric Press Inc.; 1968.
12. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. Washington, DC: American Psychiatric Press, Inc.; 1980.
13. Aboraya A, Rankin E, France C, et al. The reliability of psychiatric diagnosis revisited: the clinician’s guide to improve the reliability of psychiatric diagnosis. Psychiatry (Edgmont). 2006;3:41–50.
14. American Psychiatric Asoociation Diagnostic and Statistical Manual of Mental Disorders. 3rd ed, Revised. Washington, DC: American Psychiatric Press Inc.; 1987.
15. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Press Inc.; 1994.
16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed, Text Revised. Washington, DC: American Psychiatric Press Inc.; 2000.
17. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC, American Psychiatric Press Inc.; 2013.
18. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
19. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schiz Bull. 1987;13:261–276.
20. Overall JE, Gorham DR. The Brief Psychiatric Rating Scale (BPRS): recent developments in ascertainment and scaling. Psychopharmacol Bull. 1988;24:97–99.
21. Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011.
22. Wing JK, Birley JL, Cooper JE, Graham P, Isaacs AD. Reliability of a procedure for measuring and classifying “present psychiatric state”. Br J Psychiatry. 1967;113:499–515.
23. WHO. Compsite International Diagnostic Interview (CIDI). Geneva: World Health Organization; 1990.
24. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22–33;quiz 34–57.
25. Williams JB, Gibbon M, First MB, et al. The Structured Clinical Interview for DSM-III-R (SCID). II. Multisite test-retest reliability. Arch Gen Psychiatry. 1992;49:630–636.
26. Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629.
27. Wing Jk, Babor T, Brugha T, et al. SCAN. Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry. 1990;47:589–593.
28. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Clinical Version (SCID-CV). Washington, DC: American Psychiatric Press Inc.; 1997.
29. Nienhuis FJ, van de Willige G, Rijnders CA, et al. Validity of a short clinical interview for psychiatric diagnosis: the mini-SCAN. Br J Psychiatry. 2010;196:64–68.
30. Aboraya A. Use of structured interviews by psychiatrists in real clinical settings: results of an open-question survey. Psychiatry (Edgmont). 2009;6:24–28.
31. Duffy FF, Chung H, Trivedi M, et al. Systematic use of patient-rated depression severity monitoring: is it helpful and feasible in clinical psychiatry? Psychiatr Serv. 2008;59:1148–1154.
32. Gilbody SM, House AO, Sheldon TA. Psychiatrists in the UK do not use outcomes measures. National survey. Br J Psychiatry. 2002;180:101–103.
33. Bastiaens L. Poor Practice, Managed Care, and Magic Pills: Have We created a Mental Health Monster? Psychiatric Times. 2011;28:1–4.
34. Morrison J. The First Interview. 3rd ed. New York: The Guilford Press; 2008.
35. Rettew DC, Lynch AD, Achenbach TM, et al. Meta-analyses of agreement between diagnoses made from clinical evaluations and standardized diagnostic interviews. Int J Methods Psychiatr Res. 2009;18:169–184.
36. Busner J, Kaplan SL, Greco Nt, Sheehan DV. The use of research measures in adult clinical practice. Innov Clin Neurosci. 2011;8:19–23.
37. Nasrallah H. Long overdue: measurement-based psychiatric practice. Current Psychiatry. 2009;8:14–16.
38. Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435.
39. Williams JBW, Kobak KA. Development and reliability of a structured interview guide for the Montgomery-Asberg Depression Rating Scale (SIGMA). Br J Psychiatry. 2008;192(1):52–58.
40. Aboraya A. The validity results of the Standard for Clinicians’ Interview in Psychiatry (SCIP). Schiz Bull. 2015;41:S103–S104.
41. Aboraya A, El-Missiry A, Barlowe J, et al. The reliability of the Standard for Clinicians’ Interview in Psychiatry (SCIP): a clinician-administered tool with categorical, dimensional and numeric output. Schiz Res. 2014;156:174–183.
42. McHugh PR, Slavney PR. Mental illness—comprehensive evaluation or checklist? N Engl J Med. 2012;366:1853–1855.
43. Helzer JE, Kraemer HC, Krueger RF, Wittchen HU, Sirovatka PJ, Regier DA. Dimensional Appoaches in Diagnostic Classification: Refining the Research Agenda for DSM-V. Arlington, VA: American Psychiatric Press Inc.; 2008.
44. Ustun TB, Tien AY. Recent developments for diagnostic measures in psychiatry. Epidemiol Rev. 1995;17:210–220.
45. Ozomaro U, Wahlestedt C, Nemeroff CB. Personalized medicine in psychiatry: problems and promises. BMC medicine. 2013;11:132.
46. Kupfer DJ, First MB, Regier DA. A research agenda for DSM-V. Washington, DC: American Psychiatric Press Inc.; 2002.
47. Kupfer DJ, Regier DA, Kuhl EA. On the road to DSM-V and ICD-11. Eur Arch Psychiatry Clin Neurosci. 2008;258 Suppl 5:2–6.
48. Taylor MAV. Descriptive Psychopathology: The Signs and Symptoms of Behavioral Disorders. New York: Cambridge University Press; 2009.
49. Taylor MA, Shorter E, Vaidya NA, Fink M. The failure of the schizophrenia concept and the argument for its replacement by hebephrenia: applying the medical model for disease recognition. Acta Psychiatrica Scandinavica. 2010;122:173–183.
50. Andreasen NC, Flaum M, Arndt S. The Comprehensive Assessment of Symptoms and History (CASH): an instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry. 1992;49:615–623.
51. Committee PGCC. Genomewide association studies: history, rationale, and prospects for psychiatric disorders. Am J Psychiatry. 2009;166:540–556.
52. Ghaemi N. Psychopathology for what purpose? Acta psychiatrica Scandinavica. 2014;129:78–79.
53. Insel T, Cuthbert B, Garvey M, et al. Research Domain of Criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–751.
54. Cuthbert BN. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry. 2014;13:28–35.





