 by Varun Monga, MD, and Prasad R. Padala, MD, MS, FACHE
by Varun Monga, MD, and Prasad R. Padala, MD, MS, FACHE
Dr. Monga is from Banner Thunderbird Medical Center, Glendale, Arizona, and Dr. Padala is from the Central Arkansas Veteran’s Healthcare System Geriatric Research Education and Clinical Center, Little Rock, Arkansas.
Innov Clin Neurosci. 2015;12(9–10):33–36.
Funding: No funding was received for the preparation of this manuscript.
Financial Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Aripiprazole, apathy, depression
Abstract: Objective: The objective of this article is to present a case of improved outcome of apathy syndrome with aripiprazole. Case summary: A 42-year-old man with depression and seizure disorder had significant apathy that did not respond to carbamazepine, sertraline, and topiramate. Apathy was assessed using Apathy Evaluation Scale. Discontinuation of carbamazepine did not alleviate apathy. Aripiprazole, a novel antipsychotic with partial agonistic activity at dopamine D2 receptors, was introduced and the dose adjusted to 15mg a day. The patient showed significant improvement in apathy after six weeks of therapy with aripiprazole. Discussion: Depression is often mistaken for apathy, which is different in symptoms, presentation, and treatment options. Selective serotonin reuptake inhibitors are known to cause or increase symptoms of apathy in some patients. Recent evidence suggests that dopamine receptor agonists can be helpful in treatment of apathy. Apathy significantly improved in this patient after initiation of aripiprazole. Conclusion: Aripiprazole may be useful for treatment of apathy syndrome. Its role in treatment of apathy requires further investigation in clinical trials.
Introduction
Apathy is a profound loss of motivation not attributed to decreased level of consciousness, cognitive impairment, or emotional distress.[1] Apathy refers to a set of behavioral, emotional, and cognitive features such reduced interest and participation of activities of daily life. Another prime characteristic is lack of initiative or an absence of responsiveness to stimuli as demonstrated by a lack of self initiated action.[2] Apathy is highly prevalent in neurodegenerative diseases such Alzheimer’s disease (70–90 %) and Parkinson’s disease (63.3 %).[3,4] Although the symptoms of apathy and depression overlap, one hypothesis is that apathy and depression are not the same.[5] Apathetic individuals show lack of concern while depressed individuals shows self-criticism and negative outlook—two characteristics usually absent in apathy.[6] Since reliable differentiation of apathy and depression is difficult, the Apathy Evaluation Scale (AES) was developed to assess apathy and discriminate it from depression.[7] As noted by Levy et al,[5] after assessing patients with AES, several studies have identified patients with apathy without depression in several illnesses.
Treatment of apathy lacks standard guidelines. Several agents such as amantadine, amphetamine, bromocriptine, buproprion, methylphenidate, and selegiline have been used with mixed results.[8] Recent data suggest the dysfunction in dopaminergic systems may be responsible for the neurobiology of apathy.[9] In this case report, aripiprazole, a novel antipsychotic with partial agonistic properties at serotonin 5-HT1A and dopamine D2 receptors, was initiated in our patient with significant success in relieving symptoms of apathy. Aripiprazole, with partial agonist activity at dopamine D2 receptors, binds with high affinity to recombinant human 5-HT1A receptors (H5-HT1A) while displaying potent, partial agonism at 5-HT1A receptors in a guanosine-5’-O-(3-[35S]thio)-triphosphate ([35S]GTPgS)-binding assay. An interaction with 5-HT1A receptors may contribute to the overall efficacy of aripiprazole against symptoms of schizophrenia, including anxiety, depression, problems with cognition, and negative symptoms, and to its favorable side-effect profile. Aripiprazole is considered the first dopamine-serotonergic system stabilizer.[10] Furthermore, aripiprazole shows preferential increase in dopamine release in areas of the brain implicated in apathy such as the prefrontal cortex and hippocampus in rat brain. This preferential action on medial prefrontal cortex and hippocampus may contribute to its ability to improve negative symptoms and cognition.[11] Thus we hypothesized that aripiprazole would be beneficial in treating apathy.
Case Report
A 42-year-old Caucasian man with a four-year history of depression after surgery for his seizure disorder presented to our clinic. He complained of significant anhedonia, a sense of worthlessness, and guilt. He reported a significant increase in these symptoms over the years. These symptoms were associated with tiredness, reduced amount of sleep, and frequent awakening every few of hours at night. He denied weight loss and any change in his appetite. Symptoms related to memory problems, psychosis, posttraumatic stress disorder, and bipolar disorder were denied by him. He had a past psychiatric history significant for depressive episodes. He reported his discharge from the Navy as a main trigger for his first-time episode of depression. Other medical conditions included hypertension, seizure disorder with no recurrence of seizures after the surgery, atopic dermatitis, hypothyroidism, and bursitis. No allergies were reported. He was being treated with carbamazepine 400mg twice a day, topiramate 75mg twice a day, levothyroxine NA 0.112mg daily, metoproplol tartarate 50mg twice a day, and sertraline 150mg every morning. He worked as a mail handler in a post office. He denied use of alcohol, tobacco, or recreational drugs. A diagnosis of major depressive disorder, recurrent, was made.
Upon presentation, our patient reported that the medications he was currently taking kept him seizure free and were also managing his mood symptoms. His medications were continued after confirming that the carbamazepine level was within therapeutic range. After two months, however, patient returned with the complaint of increased sedation. He reported that his mood symptoms were under good control. He reported concerns about his finances and work. He also reported significant apathy, or a disinterest in things. He reported to have lost interest even in woodworking, which had been his favorite hobby. An 18-point Apathy Evaluation Scale (AES) was conducted. The patient scored 48 on the AES (Table 1). Since carbamazepine is known to cause sedation and because the patient was seizure free for many years, a decision was made to taper and stop carbamazepine while keeping the rest of his medications at that same doses.
On a return visit four months later, the patient continued to report feelings of apathy and that nothing motivated him anymore. He had been off of the carbamazepine for three months and did not have any recurrence of seizures. AES was repeated with a score of 45 (Table 1).
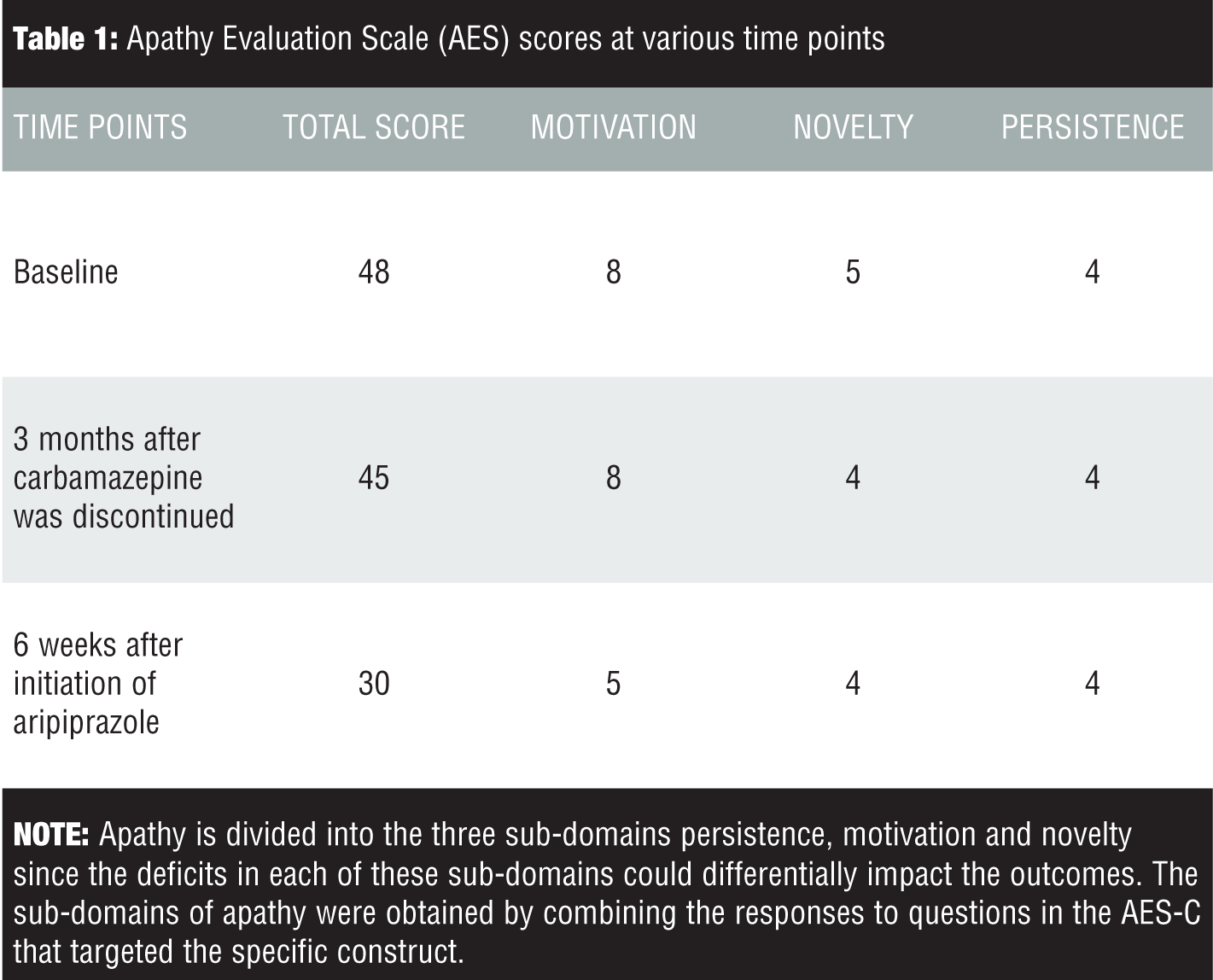
At this point, he was started on aripiprazole 10mg daily. Two weeks after initiation of aripiprazole, the patient reported that 10mg did not seem strong enough, so we increased his dosage to 20mg. The patient reported somnolence at this dosage, so we reduced aripiprazole to 15mg a day. When the patient returned for his six-week follow-up visit, he reported that his motivation had improved. He denied any side effects. He also reported that his sleep had improved and that he had resumed wood working and was able to handle marital discord well. AES was performed at this visit and the patient scored 30 points, a significant improvement from his previous score of 48.
Discussion
Apathy is not synonymous to depression.[5] Selective serotonin reuptake inhibitors (SSRIs), which are commonly used for treatment of depression, have been known to worsen the symptoms of apathy in some patients.[12] Emerging literature supports that the development of apathy syndrome is a late-onset, adverse effect of SSRIs and may be dose dependent in some cases.[13] The association of SSRIs with apathy syndrome has been reported in children, young adults, and geriatric patients.[12,14,15] Although the exact mechanism is unknown, an SSRI-induced frontal hypodopaminergic state may lead to apathy.[12] SSRI-induced apathy may be reversible in some patients by discontinuing the SSRI or by augmenting treatment with a dopaminergic agent.[15]
Frontal-sub cortical circuits mediate motor activity and behavior in humans. These frontal-sub cortical circuits originate from the supplementary motor area, frontal eye field, dorsolateral prefrontal region, lateral orbitofrontal region, and anterior cingulate portion of the frontal cortex. Prefrontal and basal ganglia lesions or dysfunction manifests as apathy.[16] There is some evidence that selective D2/D3 dopamine agonists, such as piribedil used in patients with parkinsonism, may reduce the symptoms of apathy.[17] Dopamine stimulants like methylphenidate have been used for treatment of apathy, confirming the dopamine hypothesis in the pathogenesis of apathy in patients with Parkinson’s disease.[18] Use of methylphenidate for treatment of apathy in Alzheimer’s dementia has shown positive response in recent randomized, placebo controlled trials.[19,20]
In this case, the patient had long-term symptoms of depression and apathy. Our patient was taking sertraline for depression and his symptoms of apathy were not improved. Tapering and stopping carbamazepine, a potentially sedating medication, did not result in improvement in motivation. In this case, aripiprazole was added to the patient’s regimen, and significant improvement in his apathy score after six weeks was noted. In this case report we used the MAE scale, developed specifically to assess apathy and differentiate it from depression. Our patient had score of 48 at the beginning of treatment with aripiprazole, and after six weeks of treatment, he improved significantly (MAE score of 30). Our patient did not report any adverse drug reactions. This case highlights the need to specifically assess and treat apathy in patients, especially if their depression is being treated with SSRIs.
Conclusion
Apathy is a syndrome that is often under diagnosed and under treated.[18] In this case, aripiprazole was useful in treating apathy. A favorable side effect profile shows aripiprazole as promising treatment option for apathy syndrome, especially in patients taking multiple medications. Further systematic trials are needed to assess overall safety and efficacy.
References
1. Marin RS. Differential diagnosis and classification of apathy. Am J Psychiatry. 1999;147:22–30.
2. Donald ST, Van Reekum R, Murphy KJ. Differentiation of States and Causes of Apathy. Barod J (ed). The Neuropsychology of Emotion. New York: Oxford University Press; 2000.
3. Starkstein SE, Petracca G, Chemerinski E, Kremer J. Syndromic validity of apathy in Alzheimer’s disease. Am J Psychiatry. 2001;158:872–877.
4. Pedersen KF, Alves G, Aarsland D, Larsen JP. Occurrence and risk factors for apathy in Parkinson disease: a 4-year prospective longitudinal study. J Neurol Neurosurg Psychiatry. 2009;80(11):1279–1282.
5. Levy ML, Cummings JL, Fairbanks LA, et al. Apathy is not depression. J Neuropsychiatry. 1998;10:314–319.
6. Landes AM, Sperry SD, Strauss ME, et al. Apathy in Alzheimer’s disease. J Am Geriatr Soc. 2001;49:1700–1707.
7. Marin RS, Biedrzycki RC, Firinciogullari S. Reliability and validity of the Apathy Evaluation Scale. Psychiatry Res. 1991;38:143–162.
8. Marin RS, Fogel BS, Hawkins J, et al. Apathy: a treatable syndrome. J Neuropsychiatry Clin Neurosci. 1995;7:23–30.
9. Mitchell RA, Herrmann N, Lanctôt KL. The role of dopamine in symptoms and treatment of apathy in Alzheimer’s disease. CNS Neurosci Therapeut. 2010; DOI: 10.1111/j.1755-5949.2010.00161.x.
10. Jordan S, Koprivica V, Chen R, et al. The antipsychotic aripiprazole is a potent, partial agonist at the human 5-HT1A receptor. Eur J Pharmacol. 2002;441(3):137–140.
11. Zhu Li, Ichikawa J, Jin Dai and Meltzer HY. Aripiprazole, a novel antipsychotic drug, preferentially increases dopamine release in the prefrontal cortex and hippocampus in rat brain. Eur J Pharmacol. 2004;493(1–3):75–83.
12. Hoehn-Saric R, Lipsey JR, McLeod, DR. Apathy and indifference in patients on fluvoxamine and fluoxetine. J Clin Psychopharmacol. 1990;10(5):311–386.
13. Bolling MY, Kohlenberg RJ. Reasons for quitting serotonin reuptake inhibitor therapy: paradoxical psychological side effects and patient satisfaction. Psychother Psychosom. 2004;73:380–385
14. Barnhart WJ, Makela EH, Latocha MJ. SSRI-induced apathy syndrome: a clinical review. J Psychiatr Pract. 2004;10:196–199.
15. Padala PR, Padala KP, Monga V, et al. Reversal of SSRI-associated apathy syndrome by discontinuation of therapy. Ann Pharmacother. 2012;46(3):e8. DOI. 10.1345/aph.1Q656.
16. Levy R, Dubois B. Apathy and the functional anatomy of the prefrontal cortex–basal ganglia circuits. Oxford Journals. 2006;16(7):916–928.
17. Thobois S, Lhommée E, Klinger H, et al. Parkinsonian apathy responds to dopaminergic stimulation of D2/D3 receptors with piribedil. Brain. 2013;136(Pt 5):1568–1577. doi: 10.1093/brain/awt067. Epub 2013 Mar 29.
18. Padala PR, Burke WJ, Shostrom VK et al. Methylphenidate for apathy and functional status in dementia of the Alzheimer type. Am J Geriatr Psychiatry. 2010;18:371–374.





