 by Malathi Latha Perugula, MD, and Steven Lippmann, MD
by Malathi Latha Perugula, MD, and Steven Lippmann, MD
The authors are from the Department of Psychiatry and Behavioral Science, University of Louisville School of Medicine, Louisville, Kentucky.
Innov Clin Neurosci. 2016;13(11–12):41–42.
This column series compares neurological conditions that pose differential challenges in diagnoses.
Funding: No funding was provided for the preparation of this article.
Financial disclosures: The authors have no conflicts of interest relevant to the content of this article.
Introduction
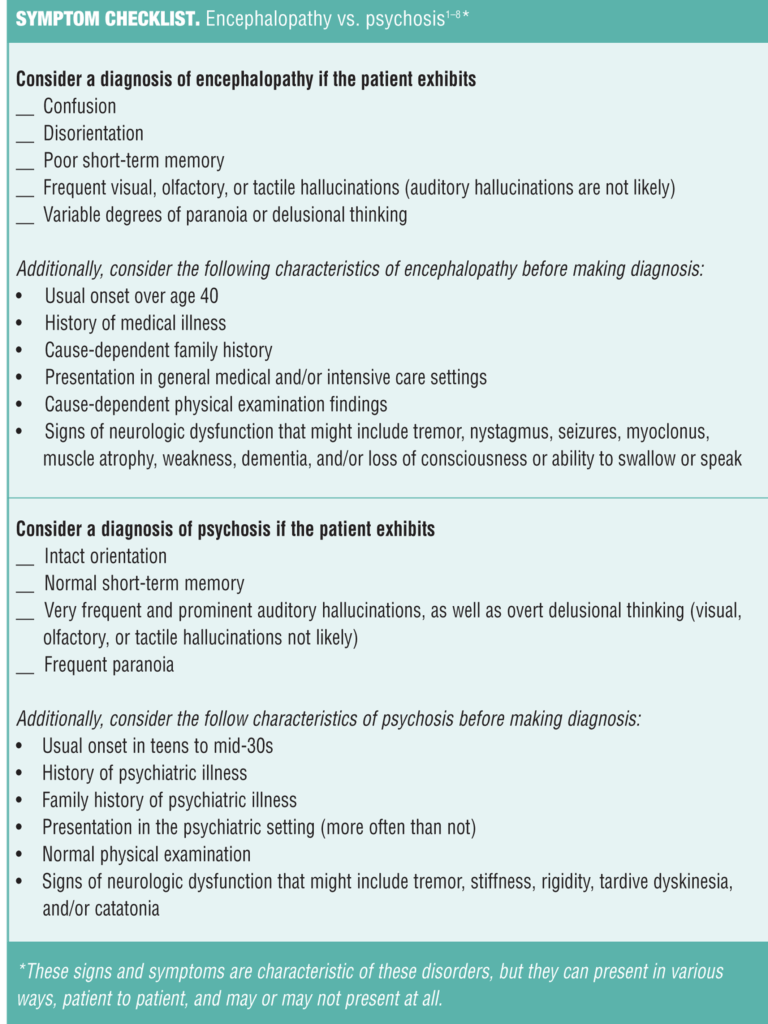
Encephalopathy and psychosis are two separate mental states that are both characterized by symptoms of paranoia, to varying degrees, but that’s about where the similarity ends. Here we present a checklist of symptoms and characteristics of both disorders for use as a diagnostic aid (See Checklist), as well as etiology and treatment.
Etiology: Encephalopathy vs. Psychosis
Encephalopathy is most commonly caused by the following:
- Organ failure (e.g., renal, hepatic, pulmonary, hypoxia, hypercapnia)
- Infection: Systemic (e.g., urinary tract, pneumonia) or involving the central nervous system (e.g., meningitis, encephalitis), bacterial, viral, parasitic, or prions, especially with high fever
- Disorders of the thyroid, adrenal, pituitary, or related glands
- Toxicity or withdrawal (e.g., alcohol, salicylates, benzodiazepines, barbiturates, tricyclic antidepressant or antipsychotic medications, poisons, organophosphates, hydrocarbons, recreational drugs, medicinal drugs)
- Metabolic disorders (e.g., abnormal concentrations of sodium, glucose, calcium, or hypophosphatemia; acidosis, alkalosis, inborn errors of metabolism)
- Anoxia
- Neoplasms (e.g., tumors of the central nervous system, paraneoplastic syndromes)
- Nutritional deficiencies (e.g., dehydration, vitamin B1, other vitamins)
- Other dysfunctions/disorders, including fever, seizures, mitochondrial dysfunction, trauma (e.g., concussion, contusion, subdural hematoma, epidural hematoma, diffuse axonal injury), vascular (e.g., ischemic and hemorrhagic strokes, vasculitis, venous thrombosis), hypertensive encephalopathy, neonatal encephalopathy, encephalomyopathy.[1–4]
Psychosis is most commonly caused by the following:
- Psychiatric illnesses (e.g., schizophrenia and related disorders, delusional disorder, brief psychotic disorder, schizotypal disorder, major depressive disorder with psychotic features, bipolar disorder with psychotic features, chronic hallucinatory psychosis)
- Myxedema
- Toxicity from stimulants (e.g., amphetamines, cocaine, methylphenidate, caffeine), steroids, and/or hallucinogenic substances (e.g., lysergic acid diethylamide, mescaline, phencyclidine)
- Menstrual cycle (i.e., in a periodicity in rhythm with the menstrual cycle)
- Recent childbirth (e.g., postpartum psychosis)
- Dopaminergic antipsychotic drugs by the depletion of dopamine (e.g., tardive psychosis).[5–8]
Treatment: Encephalopathy vs. Psychosis
If a diagnosis of encephalopathy is made…
Immediately remove any offending agent and focus treatment on the specific causative pathology (e.g., administer glucose in hypoglycemia or benzodiazepines in alcohol withdrawal). Symptomatic pharmacotherapy or restraints should only be applied when urgently needed for behavioral control.[1–4]
If a diagnosis of psychosis is made…
Antipsychotic drugs are usually the first-line of treatment, with benzodiazepines utilized for calmative influence or in cases of catatonia. Mood stabilizing pharmaceuticals might be indicated as well. If related to some offending agent, it should immediately be removed. Patients at risk for harm to themselves or others might require hospitalization, restraints, or other measures to ensure safety.[5–8]
Summary
Encephalopathy defines a clinical presentation of pathology affecting brain function, of extra-cranial or intra-cranial origin. It is manifested by an altered mental status characterized by disorientation, short-term memory impairment, inattentiveness, and often with an abnormal state of arousal. In encephalopathy, treating the underlying cause may induce remission; however, the pathology can result in permanent damage to brain function and may be fatal and/or recurrent.[1–4]
Psychosis is a clinical presentation characterized by loss of contact with reality and is usually considered a psychiatric condition. The mental status examination usually includes delusions, hallucinations, abnormalities of arousal, but with orientation and memory functions intact. In psychosis, treating the underlying cause usually resolves an acute illness, but relapse and chronicity are common.[5–8]
References
1. Samala RV, Davis MP. Encephalopathy. Xiangya Med. 2016;1:2.
2. Iacobone E, Bailly-Salin J, Polito A, et al. Sepsis-associated encephalopathy and its differential diagnosis. Crit Care Med. 2009;37(10):S331–S336.
3. Cie?ko-Michalska I, Szczepanek M, S?owik A, et al. Pathogenesis of hepatic encephalopathy. Gastroenterol Res Pract. 2012(2012):642108. doi:10.1155/2012/642108
4. De Holanda NC, De Lima DD, Cavalcanti TB, et al. Hashimoto’s encephalopathy: systematic review of the literature and an additional case. J Neuropsychiatry Clin Neurosci. 2011;23(4):384–390.
5. Larson MK, Walker EF, Compton MT. Early signs, diagnosis and therapeutics of the prodromal phase of schizophrenia and related psychotic disorders. Exp Rev Neurotherapeut. 2010;10(8):1347–1359.
6. Caton CLM, Hasin DS, Shrout PE, et al. Predictors of psychosis remission in psychotic disorders that co-occur with substance use. Schizophr Bull. 2006; 32(4): 618–625.
7. Mannion A, Slade P. Psychotic-like experiences in pregnant and postpartum women without a history of psychosis. Schizophr Res. 2014;160(1-3):118–123.
8. Trotman HD, Holtzman CW, Ryan AT, et al. The development of psychotic disorders in adolescence: a potential role for hormones. Horm Behav. 2013;64(2):411–419.




