by Jennice S. Vilhauer, PhD; Julissa Cortes; Nazanin Moali; Sally Chung; James Mirocha, MS; Waguih William IsHak, MD
by Jennice S. Vilhauer, PhD; Julissa Cortes; Nazanin Moali; Sally Chung; James Mirocha, MS; Waguih William IsHak, MD
All authors are from Cedars-Sinai Medical Center, Los Angeles, California.
Innov Clin Neurosci. 2013;10(3):12–22
Funding: Research was internally supported by CSMC Department of Psychiatry.
Financial Disclosures: The authors do not have conflicts of interest relevant to the content of this article.
Key Words: Major depressive disorder, quality of life, future directed therapy, hopelessness, cognitive behavioral therapy, positive psychology
Abstract: Objective: Impaired quality of life is a significant problem for people with major depressive disorder and is often not addressed through symptom remediation alone. This study examines a new therapy for the treatment for depression that focuses on reducing hopelessness and increasing positive future anticipation, which are factors posited to contribute to quality of life. The new treatment was compared to depressed patients in the same setting treated with group cognitive behavioral therapy.
Design: This study used a quasi-experimental design to examine the differences between future directed therapy and cognitive behavioral therapy on improving quality of life in patients with major depressive disorder. The main variables assessed at pre and post-treatment were quality of life, depressive symptoms, and hopelessness.
Setting: Outpatient Department of Psychiatry Cedars-Sinai Medical Center
Participants: Twenty-two patients completed the future directed therapy intervention and 20 patients completed the cognitive behavioral therapy intervention.
Measurements: Patient-reported outcomes were collected using the Quick Inventory of Depressive Symptoms, the Beck Hopelessness Scale, and the Quality of Life Enjoyment and Satisfaction Questionnaire-Short Form.
Results: Though both treatments were effective at improving depression, hopelessness and positive future anticipation, those patients treated with future directed therapy demonstrated significant improvements in quality of life (p=0.002) while those treated in the cognitive behavioral therapy group did not (p=0.463). The magnitude of change for the main variables was significantly larger in the future directed therapy group and change in hopelessness and change in positive anticipation predicted change in quality of life in the future directed therapy group but not the cognitive behavioral therapy group.
Conclusions: Future directed therapy is a useful treatment for patients with major depressive disorder and quality of life impairment.
Introduction
According to the World Health Organization (WHO), major depressive disorder (MDD) is the leading cause of years lost to disability.[1] Moreover, evidence consistently shows that MDD significantly impairs quality of life (QOL).[2–7] The WHO defines QOL as “an individual’s perception of his or her position in life in the context of the culture and value systems in which he or she lives, and in relation to his or her goals, expectations, standards, and concerns”[8] Most standardized measures of QOL utilize multidimensional constructs that generally include physical, emotional, and social domains.[9] Studies using QOL measures have shown that the quality of life of depressed patients is significantly lower than that of the healthy population or even that of individuals with chronic medical disorders, such as hypertension, cancer, or chronic pain,[2,5–7] and numerous studies have shown that patients with MDD and comorbid medical or psychiatric disorders are at even greater risk for low QOL.[7,10–12] Poor quality of life in patients with MDD is associated with high rates of relapse, significant negative impact on the ability to perform and/or enjoy occupational and social activities including family, impaired future outlook, medical complications such as heart disease, and overall increase of healthcare related costs.[5,12]
Although the WHO defined health as, ‘‘A state of complete physical, mental and social well-being and not merely the absence of disease,” (WHO, 1946) and despite the detrimental impact of poor QOL in this population, reduction of symptoms has remained the primary focus in the treatment of psychiatric disorders especially depression.[8,13] This may, in part, be due to a common perception that one’s QOL is really a reflection of one’s mood state, therefore making the measurement of QOL, and/or developing specific interventions for improving QOL, something that many have viewed as redundant.[14–17] More recently, however, evidence has been accruing to indicate that, while there appears to be a mediating relationship, a significant proportion of what is contributing to self-reported QOL is distinct from affective states.[18–22] Rocha et al[23] captures this perspective well by stating, “Quality of life is neither the opposite of depression, nor is euthymia a synonym for QOL.” Many patients with MDD suffer from poor QOL after reduction of symptom severity and even after achieving remission,23 and there is a growing consensus that for treatments to be successful they must move beyond merely treating the affective symptoms of depression but also substantially improve QOL.[24–26]
The majority of interventions that have been utilized to improve QOL in MDD have not been systematically investigated. Preliminary evidence for improvement of QOL has been shown with adjunct interventions such as exercise,[27,28] meditation,[29] massage,[30] humor,[31] dopaminergic agents (e.g., bupropion),[32,33] and augmenting agents (e.g., omega-3[34]). Group cognitive behavioral therapy (CBT)[35,36] has also been shown to improve QOL in patients with varying levels of depression. One factor well known to be associated with life satisfaction and general well-being,[37–39] which has not been investigated in the improvement of QOL in those with MDD until now, is positive future anticipation.
The role of future anticipation and goal attainment play a significant role in QOL theories of depression. Hollandsworth[40] conceptualizes poor QOL as stemming from hopelessness in attaining a desired future consistent with one’s standards in important areas of life leading to negative self-evaluations and depression. De Leval[41] conceptualized QOL as the perceived gap between actual experience and future aspirations, i.e., the larger the gap the lower the QOL of the individual. Moore et al[42] empirically confirmed this model and also found that reducing hopelessness about the future was related to improvements in QOL. De Leval[41] posited that when an individual is not successful in his or her attempts to close this gap through existing coping mechanisms, and increase satisfaction in valued areas of life, depression can occur. It is not surprising then that people with depression have been found to have fewer of the skills needed to close this gap, such as goal setting and problem solving.[43,44]
Future directed therapy (FDT) is a new, fully manualized, psychotherapeutic intervention developed for the treatment of depression. FDT is intended to teach a set of comprehensive skills necessary to improve one’s ability to generate more positive future experiences and thus also enhance QOL. FDT is based on a theoretical model of human behavior that posits desire for reward (e.g., an improved future) as a primary driving force. Research on people with depression has demonstrated reduced functioning in areas of the brain responsible for reward processing.[45–47] Many of the techniques that were developed in FDT are informed by a neurobehavioral perspective, and volitional allocation of attention to reward is used as a means to increase cortical activation and stimulate cognitive processes that facilitate reward attainment. FDT is different from CBT in that it does not require individuals to examine and alter irrational thinking, but rather teaches individuals how to become aware of attention that is focused on unwanted aspects of life and how to redirect attention toward things that feel more wanted. The emphasis is on helping individuals become aware of their anticipatory focused attention and the expectations they have about the future that has not yet happened. FDT does not focus on symptom reduction but instead employs the positive psychology strategy of teaching skills for thriving and wellness. A large part of the instructional work in FDT is focused on increasing the awareness of the process by which individuals create future experiences and how to direct the process in a way that leads to more positive outcomes. For more explanation on the theoretical model behind FDT and an outline of the intervention see the pilot study by Vilhauer et al.[48] That study looked at symptom severity and QOL in patients with MDD and found that FDT did significantly reduce depression and improve QOL.[45]
In the current study, we seek to go further by comparing FDT to standard CBT in terms of effectiveness in changing factors that may improve QOL, such as hopelessness and positive future expectations, and examine how changes in these factors contribute to change in QOL. Based on our review of the literature, we hypothesize that reduction of hopelessness and increased positive expectations would predict improvements in QOL in both groups. Moreover, we hypothesize that given the specific target of FDT at improving positive future anticipation, FDT will reduce hopelessness and increase positive expectations more than CBT, and subsequently FDT is expected to improve QOL more than CBT.
Methods
Setting. All patients in the Adult Outpatient Programs in the Department of Psychiatry at Cedars-Sinai Medical Center who come for a psychiatric evaluation and treatment are enrolled in the Cedars-Sinai Psychiatric Treatment outcome Registry (CS-PTR). The details of CS-PTR design as described in details in a study by IsHak et al[8] in 2012. Briefly, CS-PTR is an institutional review board (IRB)-approved registry that tracks the outcome of psychiatric interventions in a naturalistic clinical setting. Patients are assessed with the Mini International Neuropsychiatric Interview (MINI),[49] and patient-reported outcomes (described below) are collected at baseline and on quarterly basis.
Due to the naturalistic setting, we employed a quasi-experimental mixed design with pre-test/post-test as the within-subjects factor and treatment as the between-subjects factor. We sought to reduce participant variance by systematically alternating the availability of the treatment groups to which patients were assigned. Groups for FDT and CBT were offered alternately in our clinic over a one-year period for the treatment of patients with confirmed primary diagnosis of MDD. Both groups ran twice weekly for 10 weeks for a total of 20 sessions. The groups were alternately coordinated so that a new group, either FDT or CBT, was started approximately every 5 to 6 weeks, for a total of four FDT and four CBT groups. Between 10 and 12 patients were initially enrolled in each group.
Participants. Participants with a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) confirmed primary diagnosis of MDD were referred for group treatment for depression by their psychiatrist or assessment clinician for group psychotherapy as a primary or adjunctive treatment to their medication management. Participants were assigned to the next available group, which were alternately ordered. For people who were offered the FDT group, they were informed that it was a new treatment option that was being developed and they were given the option to wait for the next CBT group if they did not want to participate in FDT. No patients declined the FDT group in lieu of the CBT group.
Measures. All participants completed measures on depression, hopelessness, and QOL at baseline and post-treatment. The individual item scores were collected for the following validated measures: 1) symptom severity: Quick Inventory of Depressive Symptomatology-Self Report (QIDS-SR)[50] 2) hopelessness: Beck Hopelessness Scale (BHS),[51] and 3) QOL: QOL, Enjoyment, and Satisfaction Questionnaire—Short Form (Q-LES-Q).[52]
Positive Future Anticipation and Negative Future Anticipation were derived as subscales from the BHS based on Beck’s original factor analytic study.[51] The Positive Anticipation subscale consists of items 1, 16, 13, 15, and 19 for a possible score of 5 and includes items that all endorse a positive expectation about the future. Lower scores reflected greater positive anticipation. The Negative Anticipation subscale consists of items 2, 3, 9, 12, 16, 17, and 20 for a possible score of 7 and includes items that focus primarily on negative expectations about the future. Higher scores reflected greater negative anticipation.
Description of interventions. In the FDT group, the emphasis for the first five weeks is on teaching patients to learn how their beliefs and expectations create the future. Once this awareness is achieved, FDT then teaches people how to formulate new ways of thinking about the future and teaches specific skills for goal setting, planning, problem solving, taking action, and dealing constructively with disappointments. For a more detailed and descriptive list of topics covered in each treatment session see Vilhauer et al.[48] The CBT groups were based on the Rand Corporation CBT group therapy for depression protocol53 that covers traditional topics including cognitive model of depression, goal setting, mood monitoring, identifying automatic thoughts, identifying cognitive errors, thought challenging and restructuring using thought records, and behavioral activation. Both groups were structured as 90-minute sessions that met twice weekly for 10 weeks for a total of 20 sessions. The first meeting of every week, the patients in both groups were given didactic instructions, which addressed a skill set relevant to each model. On the second day of the week, coaching was provided for patients around the new skills they were learning and homework assignments were reviewed. For both groups, patients were instructed to spend a minimum of 20 minutes per day completing the worksheets and homework assignments they were given between sessions. The groups were administered by doctoral level psychologists and post-doctoral fellows. Ten hours of didactic instruction on each treatment was provided to therapists conducting the treatment, and weekly supervision was provided as well as periodic observation through a one-way mirror to ensure adherence to the treatment models.
Statistical analysis. Demographic variables were compared using T-test and Fisher exact analyses. Change on the main variables of interest was calculated as post-score minus pre-score. Numerical variables were summarized by mean and standard deviation. Only complete cases were analyzed, given that common intent to treat analyses (e.g., last observation carried forward [LOCF]) have been determined to be biased in pre-post test designs with only two time point measures.54 Complete case analysis is considered valid as long as pre-test scores do not predict the reason for missing cases.54 Analyses of completers vs. noncompleters showed no significant differences on the pre-test scores of the main variables of outcome. The analysis model was a repeated measures analysis of variance (RMANOVA), with “Treatment” (at two levels—FDT and CBT) as the between-subjects factor and “Time” (at two levels—pre and post) as the within-subjects factor. Differential change across the treatment groups was assessed by the “Treatment-by-Time” interaction term. Within-treatment change was assessed by a one-degree-of-freedom contrast. Two-tailed P-values were reported for the relevant effects. Between-treatment effect size was calculated using Cohen’s delta. Linear regression models were used to assess correlations between changes in numerical variables. Changes in the severity of QOL status between the FDT and CBT groups were assessed by the Fisher exact test. Statistical calculations were made using SAS version 9.2 (SAS Institute, Cary, North Carolina) and SPSS version 20.[55,56]
Results
A total of 92 patients began treatment (each arm enrolled 46 patients) with a total of 42 patients completing treatment through the 20th session. There were no statistical differences between the FDT or CBT groups on age, gender, race, or comorbid psychiatric disorders. Demographic details for both groups of completers are reported in Table 1. For the FDT group, there were 10 women and 12 men with a mean age of 56.50 (standard deviation [SD]=15.02) that completed the intervention. Fifteen (68.1%) of the completing patients carried a comorbid psychiatric diagnosis of anxiety (40.9%) or substance abuse (27.3%). Twenty patients (91%) in the FDT group were receiving pharmacological treatment. The CBT group included 13 women and seven men. Forty percent of the CBT patients had a comorbid psychiatric disorder: personality disorders (10%), anxiety disorders (10%), substance use disorders (10%), psychotic disorders (2.2%), and other psychiatric disorders (2.2%). Eighteen of the patients (90%) in the CBT group were receiving pharmacological treatment. All participants were able to speak and understand English.
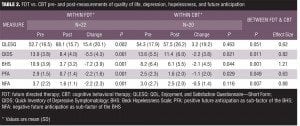
Both FDT and CBT significantly improved depression, hopelessness, and positive future anticipation; however, FDT was notably better than the CBT group at improving each of these conditions: depression,
F(1,40)= 7.082, P=0.011; hopelessness, F(1,40)=15.336, P=0.001; positive future anticipation, F(1,40)=4.122, P=0.049 (see Table 2 for means and SDs). The between-group effect sizes for depression and hopelessness were considered large at 0.82 and 1.21, respectively, and positive future anticipation had a moderate-between group effect size of 0.63. Within-group results from an RMANOVA showed that those participants treated with FDT reported significant improvement in QOL (mean=15.4, SD=20.1), F(1,21)=12.98, P=0.002, but those treated in the CBT group did not (mean=3.2, SD=19.2), F(1,19)=0.562, P=0.463. FDT was particularly effective at improving QOL in those who reported severe QOL impairments, which is defined as more than two standard deviations below the community norm (QLES-Q <55.7).[4,52,57]
Pre-treatment QOL measures show that almost 60 percent of the FDT patients and 55 precent of the CBT patients experienced severe QOL impairment, whereas post-treatment proportions of patients with severe impairment dropped to 22 percent (P=0.002) in the FDT group but did not change in the CBT group.
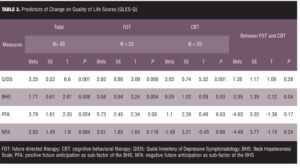
We then examined what variables predicted the change in QOL using multiple linear regressions. Table 3 details the results of these analyses. We found no evidence that age or gender was related to change in QOL. For the overall sample, change in QIDS scores (beta=3.25, SE=0.52, t=6.60, P=0.001) and BHS scores (beta=1.71, SE=0.61, t=2.81, P=0.008) predicted change in QOL. Change in positive anticipation (beta=3.79, SE=1.61, t=2.35, P=0.024) also predicted change in QOL, whereas change in negative anticipation did not (P=0.064).
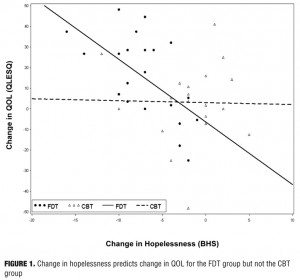
We further examined the relationship between change in depressive symptoms and change in QOL by the two treatment groups and found no evidence of a difference between predictive slopes (P=0.28). Next we examined the relationship between change in hopelessness and change in QOL between the groups and found that change in BHS scores predicted change in QOL for the FDT group (beta=2.04, SE=0.094, t=3.24, P=0.004), but not the CBT group (P=0.930) and that the difference between the slopes of the groups was significant (beta= -2.95, SEB=1.39, t= -2.12, P=0.04). Figure 1 illustrates this finding, showing that as hopelessness decreases in the FDT group, QOL improvements increase.
When we further examined the sub-factors of the BHS and their relationship to change in QOL we found that while in the FDT group, positive anticipation predicted change in QOL (beta=5.73, SE=2.45, t=2.34, P=0.03), in the CBT group it did not (P=0.63). However, there was no evidence that the slopes differed by treatment group (P=0.17). Negative anticipation did not predict change in QOL in either group, and there was no evidence that the slopes differed by treatment group (P=0.24).
We explored in each group the effect of BHS change adjusting for QIDS change using multivariable linear regression. In the FDT group, both change in depressive symptoms (beta=1.82, SE=0.86, P=0.048) and hopelessness (beta=2.18, SE=0.96, P=0.034) were significantly associated with improvement with QOL; however, in the CBT group, change in depressive symptoms (beta=4.13, SE=0.76, P=0.001) was associated with improvements in QOL, but change in hopelessness was not (beta= -0.736, SE=0.646, P=0.270). Adjusting for QIDS change, positive and negative anticipation were not significant in either group.
Discussion
The main findings in this study is that while both FDT and CBT were effective at reducing depressive symptom severity and hopelessness, FDT was not only significantly better at improving both of these aspects but also better at improving QOL. These findings were consistent with our original pilot study.[48]
The finding that CBT did not lead to a significant change in QOL was contradictory with two studies that reported group CBT did improve QOL in depressed patients. Closer examination revealed some information that may clarify this contrast. The Swan et al study[36] had a larger sample and imputed data to maximize the number of cases to be analyzed, which resulted in finding a statistical improvement in QOL scores; however, although improved, the average post-intervention QOL score still remained in the severely impaired range, which is greater than two standard deviations below the community norm.[4,52,57] Moreover, the mean post-intervention QOL score in the Swan study36 (54.7) was slightly lower than that of the mean post-intervention score of the CBT group in our current study (57.5). This illustrates the limitations of drawing meaningful conclusions exclusively from statistical significance, which is distinct from clinical significance. The second study by Wong et al[35] unfortunately reported means and standard deviations in a way that could not be interpreted, making it impossible to draw a meaningful comparison.
Reducing depressive symptoms was the largest predictor of change in QOL across all patients, indicating that depressive symptoms do have a major role in the lowered QOL experienced by patients with MDD. However, as indicated by the lack of significant change in QOL in the CBT group, reducing depressive symptoms alone does not appear to be sufficient for substantial improvement in QOL. While our hypothesis was true across the whole sample (i.e., that reduction of hopelessness and improving positive future anticipation was likely to predict change in QOL for all patients), more detailed examination comparing both groups showed that they only significantly predicted change in the FDT group, which may be the reason FDT was more successful than CBT at improving QOL. Given that patients in the CBT group did show a significant statistical change on the measures of hopelessness and positive anticipation, it seems apparent that it is the magnitude of change that matters. This finding sheds some light on one of primary underlying mechanisms of FDT. Reducing hopelessness by improving positive future anticipation appears to be an important mechanism of the treatment, resulting in positive change. Notably, change in negative future thinking did not predict change in QOL, which is consistent with studies that have found that deficits in positive future thinking contribute to depression more than negative future thinking,[58–62] and research showing that modifying negative cognitive style has little impact on the ability to produce positive future anticipation.[63]
The findings from this study are consistent with studies that have demonstrated that achieving valued life goals is associated with high levels of well-being,[64,65] as well as other research demonstrating optimism and thinking positively about the future is related to increased life satisfaction, low levels of depressions, and high levels of resilience.[66,67] The results are also consistent with the QOL theories of depression that view poor QOL to be a result of a gap between where one is and where one wants to be along with one’s perceived ability to close the gap.[50,68] By teaching people skills for how to close the gap, FDT helps to change future expectations leading to improvements in their QOL. This finding is consistent with those of Moore et al,[42] who demonstrated that change in hopelessness was the significant contributing factor for change in the gap between actual and aspirational QOL. They concluded that reduction in this gap between the present and where one wants to be should be the main therapeutic goal for depressed patients, i.e., in order to provide relief from depression and achieve desired QOL, “hopelessness needs to be tackled.” FDT appears to be doing exactly that.
Improving QOL in patients with depression can affect many other important outcomes, such as reducing relapse and the onset of comorbid health conditions while lowering overall healthcare cost and utilization.[11–15] Improvement in QOL is also an important outcome that is desired from patients who seek treatment for depression, and treatments that offer symptom reduction and restore health and well-being to patients are of high value.[48,69] The skills in FDT are intended to teach people to develop greater well-being and greater ability to thrive in life. The idea of creating greater wellness as a means of reducing illness is consistent with many of the ideas developed by the recovery model of mental illness[70] and the positive psychology movement,[71] which focus on building the strengths and potential of an individual. As QOL has been referred to as the “ultimate outcome measure of interventions in major depressive disorder,”[23] FDT offers an important contribution among the many choices of treatments for depression.
Limitations. This study used a quasi-experimental design in a naturalistic setting that assigned patients to treatment groups based on the availability during the time period that they were referred, not true random assignment. However, we believe the study reflects outcomes of real clinical practice, which is of high value in determining the effectiveness of a therapeutic treatment,[72,73] and we adhered to guidelines for studies in naturalistic settings.[72,74] The sample size of the completers was small, and both groups experienced significant attrition from treatment. Nevertheless, noncompletion rates were similar for both groups, and these rates are comparable to attrition rates from other psychotherapy studies.[75–86] While there were no statistical differences between groups on any of the demographic variables, it is possible that due to the small sample size the outcome of the groups may have been affected by diagnostic comorbidities. Also due to the small sample size and because this was an early-phase, nonrandomized trial with the goal of establishing the effect of a new treatment on the QOL of patients with depression, while also examining the potential mechanism, we did not delineate between those with chronic and nonchronic depression. Further examination of how such differences may affect response outcome would be warranted in a larger, randomized trial. Data were only gathered pre- and post-treatment, so we were only able to use a completer analysis to examine data. Most patients in this study were also receiving psychotropic medication, so the effects of treatment interventions alone are unknown, though most patients had begun medication at least one month prior to the group treatment and many patients had been stabilized on medication for three months or longer.
There was no follow-up to determine the length of the treatment effect. Self-report measures were used to assess outcomes without clinician assessment. Nevertheless, more emphasis is now being placed on patient-reported outcomes as a vital source of information about impact of treatment, particularly in QOL research, as illustrated by the National Institute of Mental health initiative Patient-Reported Outcomes Measurement Information System (PROMIS).[87] The measure of positive anticipation[51] in this study was a sub-scale from the BHS, and though derived from factor analysis, it is likely not as robust of an independent measure of positive future thinking such as the Future Thinking Task developed by Macleod et al.[88] It would be recommended that future studies utilize their established measure to assess changes in positive future thinking.
Conclusion
FDT is a new psychotherapeutic treatment for the treatment of depression with a specific mechanism that appears to reduce hopelessness and increases positive future expectations more than standard CBT in patients with depression. Treatments that significantly improve QOL are of high value in maintaining remission and overall restoration of health.[69] Given that the mechanisms of FDT maps to broader theoretical models of QOL, adaptations of FDT may also be useful in improving QOL in other patient populations where QOL impairment is high such as cancer survivors[89] and heart transplant patients.[90]
References
1. World Health Organization. Mathers C, Boerma T, Ma Fat D. The global burden of disease: 2004 update. 2008;1:1–146. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/. Accessed March 2013.
2. Bonicatto S C, Dew M A, Zaratiegui R, et al. Adult outpatients with depression: Worse quality of life than in other chronic medical diseases in Argentina. Soc Sci Med. 2001;52(6):911–919.
3. Goldney R D, Fisher L J, Wilson DH, Cheok F. Major depression and its associated morbidity and quality of life in a random, representative Australian community sample. Aust N Z J Psychiatry. 2000;34:1022–1029.
4. Rapaport M H, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162(6):1171–1178.
5. Papakostas G I, Petersen T, Mahal Y, et al. Quality of life assessments in major depressive disorder: a review of the literature. Gen Hosp Psychiatry. 2004;26(1):13–17.
6. Doraiswamy PM, Khan ZM, Doahue J, Richard NE. The spectrum of quality-of-life impairments in recurrent geriatric depression. J Gerontol Med Sci. 2002;57(2):M134–M137.
7. Saarijarvi S, Salminen J K, Toikka T, Raitasalo R. Health-related quality of life among patients with major depression. Nord J Psychiatry. 2002;56(4):261–264.
8. IsHak WW, Balayan K, Bresee C, et al. A descriptive analysis of quality of life using patient-reported measures in major depressive disorder in a naturalistic outpatient setting. Qual Life Res. 2012:1–12.
9. Fayers P, Machin D. Quality of Life: The Assessment, Analysis, and Interpretation of Patient-reported Outcomes. New York, NY: John Wiley & Sons Limited; 2007.
10. Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55(7):580–592.
11. Lane D, Carroll D, Ring C, et al. Do depression and anxiety predict recurrent coronary events 12 months after myocardial Infarction? QJM 2000;93(11):739–744.
12. Keller MB, Boland RJ. Implications of failing to achieve successful long-term maintenance treatment of recurrent unipolar major depression. Biol Psychiatry. 1998;44(5):348–360.
13. Tedlow J, Fava M, Uebelacker L, et al. Outcome definitions and predictors in depression. Psychother Psychosom. 1998;67(4–5):266–270.
14. Katschnig H. How useful is the concept of quality of life in psychiatry? Curr Opin Psychiatry. 1997;10:337–345.
15. Katschnig H, Simhandl C, Serim M, et al. Depression-specific quality of life scales are flawed. Presented at American Psychiatric Association Annual Meeting. Boston, Massachusetts; 1990.
16. Monroe SM, Steiner SS. Social support and psychopathologyI interrelations with preexisting disorders,stress and personality. J Abnorm Psychol.1986;95:29–39.
17. Schwarz N, Clore G L. Mood, misattributioni and judgements of well-being: informative and directive functions of affective states. J Pers Soc Psychol. 1983;45:513–523.
18. Leinonen E, Skrstein J, Behnke K, et al. Efficacy and tolerability of mirtazapine versus citalopram: a double-blind randomised study in patients with major depressive disorder: Nordic Antidepressant Study Group. Int Clin Psychopharmacol. 1999;14:329–337.
19. Lydiard R B, Stahl S M, Hertzman M, Harrison W M. A double-blind, placebo-controlled study comparing the effects of sertraline versus amitriptyline in the treatment of major depression. J Clin Psychiatry. 1997;58:484–491.
20. Russell JM, Koran LM, Rush J, et al. Effect of concurent anxiety in response to sertraline and imipramine in patients with chronic depression. Depress Anxiety. 2001;13:18–27.
21. Wheatley DP, van Moffaert M, Timmerman L, Kremer CM. Mirtazapine: efficacy and tolerability in comparison with fluoxetine in patients with moderate to severe major depressive disorder. Mirtazapine-Fluoxetine Study Group. J Clin Psychiatry. 1998;59:306–312.
22. Trompenaars FJ, Masthoff ED, Van Heck G L, et al. Relationship between mood related disorders and quality of life in a population of Dutch adult psychiatric outpatients. Depress Anxiety. 2006;23:353–363.
23. IsHak WW, Greenberg J M, Balayan K, et al. Quality of life: The ultimate outcome measure of interventions in major depressive disorder. Harv Rev Psychiatry. 2011;19:229–239.
24. Rush AJ, Trivedi MH. Treating depression to remission. Psychiatr Ann. 1995;25:704–709.
25. Zimmerman M, Mattia JI, Posternak MA. Are subjects in pharmacological treatment trials of depression representative of patients in routine clinical practice? Am J Psychiatry. 2002;150:459–473.
26. Angst J, Kupfer DJ, Rosenbaum JF. Recovery from depression: risk or reality? Acta Psychiatrica Scandinaviaca. 1996;93(6):413–419
27. Acil AA, Dogan S, Dogan O. The effects of physical exercises to mental state and quality of life in patients with schizophrenia. J Psychiatr Ment Health Nurs. 2008;15(10):808–815.
28. Larun L, Nordheim L V, Ekeland E, et al. Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database Syst Rev. 2006;3:CD004691.
29. Nyklicek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: Is increased mindfulness indeed the mechanism? Ann Behav Med. 2008;35(3):331–340.
30. Hamre HJ, Witt CM, Glockmann A, et al. Rhythmical massage therapy in chronic disease: a 4-year prospective cohort study. J Altern Compliment Med. 2007;13(6):635–642.
31. Marziali E, McDonald L, Donahue P. The role of coping humor in the physical and mental health of older adults. Aging Mental Health. 2008;12(6):713–718.
32. Fortner MR, Brown K, Varia IM, et al. Effect of bupropion SR on the quality of lIfe of elderly depressed patients with comorbid medical disorders. Prim Care Compan J Clin Psychiatry. 1999;1(6):174–179.
33. Dunner DL, Kwong WJ, Houser TL, et al. Improved health-related quality of life and reduced productivity loss after treatment with bupropion sustained release: a study in patients with major depression. J Clin Psychiatry. 2001;3(1):10–16.
34. van der Watt G, Laugharne J, Janca A. Complementary and alternative medicine in the treatment of anxiety and depression. Curr Opin Psychiatry. 2008;21(1):37–42.
35. Wong DF. Cognitive and health-related outcomes of group cognitive behavioural treatment for people with depressive symptoms in Hong Kong: randomized wait-list control study. Aust N Z J Psychiatry. 2008;42(8):702–711.
36. Swan A, Watson HJ, Nathan PR. Quality of life in depression: an important outcome measure in an outpatient cogntive-behavioural therapy group programme? Clin Psychol Psycother. 2009(16):485–496.
37. Boyd J, Zimbardo P. Time perspective, health, and risk taking, in understanding behavior in the context of time. In: Strathman A, Joireman J (eds). Mahwan, NJ: Lawrence Erlbaum Associates; 2005.
38. Lowenstein G, Weber E, Hsee C, Welch N. Risk as feelings. Psychol Bull. 2001;127:267–286.
39. Sohl SJ, Moyer A. Refining the conceptualization of an important future-oriented self-regulatory behavior: proactive coping. Pers Individ Dif. 2009;47(2):139–144.
40. Hollandsworth JG. Subjective well-being and behavior therapy: challenge, opportunity, or dead end? Behav Ther. 1987;3:65–68.
41. de Leval N. Scales of depression, ill-being, and the quality of life–is there any difference? an assay in taxonomy. Qual Life Res. 1995;4:259–269.
42. Moore M, Hofer S, McGee H, Ring L. Can the concepts of depression and quality of life be integrated using a time perspective? Health Qual Life Outcomes. 2005;3(1):1–10.
43. MacLeod A, Tata P, Tyrer P, et al. Personality disorder and future-directed thinking in parasuicide. J Personal Disord. 2004;18(5):459–466.
44. Emmons RA. Abstract versus concrete goals: personal striving level, physical illness, and psychological well-being. J Pers Soc Psychol. 1992;62(2):292–300.
45. Der-Avakian A, Markou A. The neurobiology of anhedonia and other reward-related deficits. Trends in Neuroscience. 2012;35(1):68–77.
46. Dichter GS, Kozink RV, McClernon FJ, Smoski MJ. Remitted major depression is characterized by reward network hyperactivation during reward anticipation and hypoactivation during reward outcomes. J Affect Disord. 2012;136(3):1126–1134.
47. Smoski MJ, Ritternberg A, Dichter GS. Major depressive disorder is characterized by greater reward network activation ot monetary than pleasant imgage rewards. Psychiatry Res Neuroimag. 2011;194(3):263–270.
48. Vilhauer J, Young S, Kealoha C, et al. Treating major depression by creating positive expectations for the future: a pilot study for the effectiveness of future directed therapy (FDT) on symptom severity and quality of life. CNS Neurosci Therapeut. 2011:1–8.
49. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33.
50. Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583.
51. Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the Hopelessness scale. J Consult Clin Psychol. 1974;42(6):861–865.
52. Endicott J, Nee J, Harrison W, Blumenthal R. Quality of life enjoyment and satisfaction questionnaire: a new measure. Psychopharmacol Bull. 1993;29(2):321–326.
53. Munoz R, Miranda J. Group Therapy Manual for Cognitive-Behavioral Treatment of Depression. Los Angeles, CA:?Rand Corp.; 1996.
54. Salim A, Mackinnon A, Christensen H, Griffiths K. Comparison of data analysis strategies for intent-to-treat analysis in pre-test-post-test designs with substantial dropout rates. Psychiatry Res. 2008;160:335–345.
55. IBM, SPSS Software, IBM http://www-01.ibm.com/software/analytics/spss/
56. SAS, http://www.sas.com/, SAS institute Inc.: Cary, North Carolina.
57. Schechter D, Endicott J, Nee J. Quality of life of normal; controls: association with lifetime history of mental illness. Psychiatry Res. 2007;152(1):45–54.
58. MacLeod A, Cropley M. Depressive future-thinking: the role of valence and specificity. Cog Ther Res. 1995;19(1):35–50.
59. MacLeod A, Byrne A. Anxiety, depression, and the anticipation of future positive and negative experiences. J Abnorm Psychol. 1996;105(2):286–289.
60. MacLeod A, Salaminiou E. Reduced positive future-thinking in depression: cognitive and affective factors. Cog Emot. 2001;15(1):99–107.
61. MacLeod A, Tata P, Kentish J, Jacobsen H. Retrospective and prospective cognitions in anxiety and depression. Cog Emot. 1997;11(4):467–479.
62. Stöber J. Prospective cognitions in anxiety and depression: replication and methodological extension. Cog Emot. 2000;14(5):725–729.
63. O’Connor R, Cheyne W. Hopelessness: the role of depression, future directed thinking and cognitive vulnerability. Psychol Health Med. 2000;5(2):155–161.
64. Emmons RA, Diener E. A goal–affect analysis of everyday situational choices. J Res Person. 1986;20(3):309–326.
65. MacLeod A, Coates E, Hetherton. Increasing well-being through teaching goal-setting and planning skills: results of a brief intervention. J Happiness Stud. 2008;9:185–196.
66. Hess LM. Predictors of life staisfaction and symptoms of depression in dysthymic disorder Dissertation Abstracts International: Section B: The Sciences and Engineering 2002;63(4-B):2058.
67. Mak WS, Ng IS, Wong C. Resilience: enhancing well-being through the positive cognitive triad. J Couns Psychol. 2011;58(4):610–617.
68. Sheehan D, Lecrubier Y, Sheehan K, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33.
69. Ezquiaga E, Garcia-Lopez A, de Dios C, et al. Clinical and psychosocial factors assoicated with the outcome of unipolar major depression: a one year prospective study. J Affect Disord. 2004;79:63–70.
70. Roberts G, Wolfson P. The rediscovery of recovery: open to all. Adv Psychiatr Treat. 2004;10:37–49.
71. Seligman MEP. Positive psychology, positive prevention, and positive therapy. In: Handbook of Positive Psychology. Snyder CR, Lopez SJ (eds). New York, NY: Oxford University Press; 2002:3–9.
72. Leichsenring F. Randomized controlled versus naturalistic studies: a new research agenda. Bull Menninger Clin. 2004;68(2):137–151.
73. Malm UF, Fedovskiy K, Gothenberg J. Naturalistic studies-Researching the everyday clinical world. Informa Health Care. 2009;63(2):100–101.
74. Nathan PE, Gorman JM. A Guide to Treatments That Work, Second Edition.Oxford University Press; 2002.
75. Ben-Porath DD. Strategies for securing commitment to treatment from individuals diagnosed with borderline personality disorder. J Contemp Psychother. 2004;34(3):247–263.
76. McMurran M, Huband N, Overton E. Non-completion of personality disorder treatments: a systematic review of correlates, consequences, and interventions. Clin Psychol Rev. 2010;30:277–287.
77. Elkin I, Shea MT, Watkins JT, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry. 1989;46:971–982.
78. Elkin I. The National Institute of Mental Health Treatment of Depression Collaborative Research Program: where we began and where we are. In: Bergin AE, Garfield SL (eds). Handbook of Psychotherapy and Behavior Change, Fourth Edition. 1994:114–139.
79. Hollon SD, DeRubeis RJ, Evans MD, et al. Cognitive therapy and pharmacotherapy for depression: singly and in combination. Arch Gen Psychiatry. 1992;49:773–781.
80. Baekeland F, Lundwall L. Dropping out of treatment: a critical review. Psychologic Bull. 1975;82(5):738–783.
81. Persons JB, Burns DD, Perloff JM. Predictors of dropout in cognitive therapy for depression in a private practive setting. Cog Ther Res. 1988;12:557–575.
82. Pekarik G. Post treatment adjustment of clients who drop out early vs. late in treatment. J Clin Psychol. 1992;48:379–387.
83. Wierzbicki M, Pekarik G. A meta-analysis of psychotherapy dropout. J Profess Psychol Res Pract. 1993;24(2):190–195.
84. Oei TPS, Kazmierczak T. Factors associated with dropout in a group cognitive behavior therapy for mood disorders. Behav Res Ther. 1997;35(11):1025–1030.
85. Brogan MM, Prochaska JO, Prochaska JM. Predicting termination and continuation status in psychotherapy using the Transtheoretical Model. Psychotherapy. 1999;36:105–113.
86. Principe JM, Marci CD, Glick DM, Ablon J S. The relationship among patient contemplation, early alliance and continuation in psychotherapy. Psychother Theory Res Pract Train. 2006;43:238–243.
87. Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3–S11.
88. MacLeod A, Pankhania B, Lee M, Mitchell D. Parasuicide, depression, and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973–977.
89. Smith SK, Crespi CM, Petersen T, et al. The impact of cancer and quality of life for post-treatment non-Hodgkin lymphoma survivors. Psychooncology. 2010;19:1259–1267.
90. Holtzman S, Abbey SE, Stewart DE, Ross HJ. Pain after heart transplantation: prevalence and implications for quality of life. Psychosomatics. 2010;51:230–236