by Shahid Ali, MD; Shagufta Jabeen, MD; and Farzana Alam, MD
by Shahid Ali, MD; Shagufta Jabeen, MD; and Farzana Alam, MD
Dr. Ali is Associate Professor of Clinical Psychiatry, Meharry Medical College, Nashville, Tennessee; Dr. Jabeen is Adjunct Associate Clinical Professor of Clinical Psychiatry, Vanderbilt University, and Staff Psychiatrist, Veterans Administration Hospital, Nashville, Tennessee; Dr. Alam is from Meharry Medical College, Nashville, Tennessee.
Innov Clin Neurosci. 2015;12(1–2):12–20.
Funding: No funding was provided for the preparation of this article.
Financial disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Malingering, posttraumatic stress sisorder, PTSD, malingered PTSD, factitious disorder, Diagnostic and Statistical Manual of Mental Disorders
Abstract: The primary aim of this article is to aid clinicians in differentiating true posttraumatic stress disorder from malingered posttraumatic stress disorder. Posttraumatic stress disorder and malingering are defined, and prevalence rates are explored. Similarities and differences in diagnostic criteria between the fourth and fifth editions of the Diagnostic and Statistical Manual of Mental Disorders are described for posttraumatic stress disorder. Possible motivations for malingering posttraumatic stress disorder are discussed, and common characteristics of malingered posttraumatic stress disorder are described. A multimodal approach is described for evaluating posttraumatic stress disorder, including interview techniques, collection of collateral data, and psychometric and physiologic testing, that should allow clinicians to distinguish between those patients who are truly suffering from posttraumatic disorder and those who are malingering the illness.
Introduction
Posttraumatic stress disorder (PTSD) was first described in the Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM III) in 1980.[1] Since its introduction in the DSM III, PTSD has become a common basis for civil lawsuits and occupational claims, likely because almost all of its diagnostic elements are based on self-report, which makes malingering more easily accomplished.[2–6] According to Guriel et al,[2] by 1989, the diagnosis of PTSD was referred to as the “diagnosis of choice” in civil litigation. At this time, 14 percent of all occupational injury claims are based on PTSD or other stress-related diagnoses.[2–6]
Malingering of PTSD is the intentional production of false or grossly exaggerated physical and/or psychological symptoms associated with the diagnosis of PTSD in order to obtain external incentives (e.g., financial and/or personal gains).[2]
This article seeks to aid clinicians in differentiating true PTSD from malingered PTSD. Characteristics of true PTSD and malingered PTSD are described, and a multimodal approach for evaluating PTSD that aids clinicians in identifying those individuals who are malingering the illness is provided.
Definitions and Prevalence
PTSD. According to the fifth edition of the DSM (DSM 5),[7] the trigger to PTSD is “…exposure to actual or threatened death, serious injury or sexual violation.” The DSM 5 further states, “The exposure must result from one or more of the following scenarios, in which the individual directly experiences the traumatic event; witnesses the traumatic event in person; learns that the traumatic event occurred to a close family member or close friend (with the actual or threatened death being either violent or accidental); or experiences first-hand repeated or extreme exposure to aversive details of the traumatic event (not through media, pictures, television or movies unless work-related). The disturbance, regardless of its trigger, causes clinically significant distress or impairment in the individual’s social interactions, capacity to work or other important areas of functioning. It is not the physiological result of another medical condition, medication, drugs or alcohol.”[7]
Using the diagnostic criteria for PTSD?as established by the fourth edition, text revision (DSM-IV-TR),[8] PTSD prevalence estimates are variable, with a lifetime prevalence rate of 1 to 14 percent but an at-risk prevalence rate of 3 to 58 percent.[2] Prevalence rates appear to vary significantly with the type of trauma experienced. For example, the prevalence rate among combat soldiers is 20 to 30 percent, whereas among the general public, it is 12 to 15 percent.[6,9] Prevalence rates also appear to be higher among women than men, and prevalence increases with multiple traumatic event exposure.[10] Research suggests that based on the revised diagnostic criteria for PTSD in the DSM 5, prevalence rates should be similar to those found using DSM-IV criteria.[7,10,11]
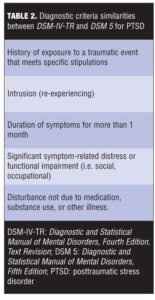
Tables 1 and 2 describe the similarities and differences between DSM-IV-TR and DSM 5 diagnostic criteria for PTSD.
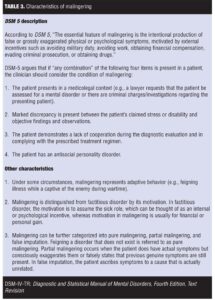
Malingering. Malingering is not considered a mental disorder by the DSM 5. It is categorized under “other conditions that may be a focus of clinical attention.” Table 3 lists characteristics of malingering as described by DSM 5 and elsewhere in the literature.[2,7,8,12,13] Hall et al[3] described the following characteristics seen in malingerers that may help differentiate them from true sufferers of PTSD: 1) Malingerers are more often encountered in outpatient settings (true PTSD sufferers are more often encountered in hospitals); 2) Malingerers are often uncooperative with exams and are unwilling to undergo clinical procedures or medication trials; and 3) Malingerers often have histories of previous lawsuits; run-ins with the law; acting-out behavior in school, workplace, or the military; sporadic employment and attendance at work; substance use; turning down jobs that accommodate or accept their professed “partial” disability; and few, if any, longstanding financial responsibilities.[3] Additionally, malingerers have difficulty elaborating on their symptoms; may have decreased capacity to work but increased ability to enjoy recreational activities; often have histories of lack of improvement in their condition over time; and lack objective evidence of concentration deficits, hyper-vigilance, irritability, and avoidance (especially avoidance of trauma-related topics during the interview), all of which are commonly experienced in true PTSD?cases.[3,9,12]
To date, no exact prevalence rates for malingering exist. According to Rogers,[14] practitioners do not typically scrutizine the accuracy of client reports, and, consequently, formal assessments for malingering are not often carried out. The few studies that have been done on prevalence of malingering indicate a considerable variation in prevalence rates.[15–19] One forensic study estimated 15.7 percent in forensic evaluations and 7.4 percent in non-forensic evaluations.[15] Estimates of malingering psychological symptoms after personal injury range from one percent to over 50 percent.[17,18] In one study, it was reported that as many as 20 to 30 percent of personal injury claimants feign posttraumatic disturbances in an attempt to receive financial compensation.[2,18] One study estimated that 75 percent of Vietnam veterans who received PTSD compensation through the Veterans Administration (VA) either exaggerated their degree of impairment (partial malingering) or feigned their condition (pure malingering).[6,19]
Motivations to Malinger PTSD
The diagnosis of PTSD relies heavily on a patient’s subjective self-report of symptoms, making the diagnosis of PTSD particularly vulnerable to malingering. Symptoms seen in PTSD, such as re-experiencing of a trauma, avoidance, negative alterations in cognitions and mood, and content of dreams are difficult to verify. Moreover, variable symptom profile and high comorbidity with a variety of clinical and personality disorders make detection of malingered PTSD challenging.[2]
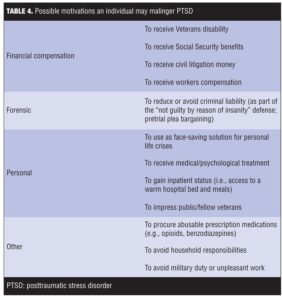
Financial gain. Rosen et al[20] point out that it is important as an evaluating physician to be wary of potential malingering when patients claiming PTSD are in a situation where “financial remuneration, benefit eligibility and or forensic determination” are involved. Most commonly, PTSD is feigned to obtain financial compensation either from governmental agencies, such as VA or Social Security, or from civil litigation.[17,21,22] The filing of personal injury lawsuits in federal court increased by more than 50 percent in the decade after PTSD was included in the DSM-III in 1980.[13]
Combat veterans diagnosed with PTSD are often rewarded financially, making malingered PTSD a means to a potentially profitable end. According to Burkett et al,[23] a veteran who qualifies for a 100-percent service-connected disability due to PTSD may be eligible for lifelong, tax-free compensation from $36,000 to $40,000 per year, in addition to other military benefits.
Financial compensation can take on different meanings for different people. Knoll points out that to some individuals money represents security but to others it may represent revenge against a hated employer or perceived aggressor. Seeking financial compensation through civil litigation may also be a last ditch effort by a claimant whose physical injury claims have thus far been unsuccessful.[12]
Personal gains. Some patients malinger PTSD to justify their level of functioning to others, such as when they have a history of failed relationships, poor occupational functioning, or legal problems. An official determination of disability due to PTSD may provide a face-saving solution for personal life crises separate from the alleged trauma (e.g., “It’s not my fault. I’m not to blame. It’s all due to what happened back in ‘Nam”).[12,24] And some individuals may feign combat-related PTSD to impress the general public or to gain the attention and the respect of fellow veterans.[25,26]
Table 4 lists other gains, in addition to financial and personal ones, that may motivate an individual to malinger PTSD.[2,17,25,27,28]
Should Malingering be investigated in all PTSD Claimants?
It is important to evaluate for malingering in PTSD cases for several reasons. First, undetected malingering can negatively impact diagnosis and treatment planning for any true mental illnesses the patient may have. Furthermore, not only will PTSD treatment in a case of malingering be ineffective and a waste valuable resources, it also exposes the patient to treatment that not only is inappropriate but may even be harmful to the patient.[29–31] Taylor et al[25] describe a case of a man who admitted to malingering after his military records revealed he had never been in combat. The patient’s treatment plan was to include imagery exposure. Had the patient not admitted to malingering prior to the start of treatment, the authors believe this form of therapy could have led to making the traumatic “memories” the patient had made up believable to him, which in turn might actually have caused the patient to develop true PTSD.
Second, because malingering is by its very definition based on deception, its presence can negatively impact the therapeutic alliance between the clinician and the patient, creating a barrier to proper care. Furthermore, clinicians who regularly work with traumatized populations who have high rates of suspected but undetected malingering may become suspicious of the motives of all their patients, rather than the smaller subset who are actually malingering. If more attention is placed on detecting malingering populations, it may result in greater confidence and improved therapeutic alliances with patients who are not malingering.[29]
Third, undetected malingering negatively impacts the economy. LoPiccolo et al[32] point out that in 1995, the total cost of insurance fraud in the United States was estimated to be $85.3 billion, and most was due to health insurance fraud that included malingering of PTSD. Another example is the policy of the VA to offer psychiatric disability compensation for eligible veterans, for which PTSD is one of the most highly compensated disabilities.[33] Thus, there is a large financial incentive to chronically malinger PTSD, which ultimately and unfortunately diverts money and proper care away from those individuals who legitimately are in need of them.[29]
Fourth, undetected malingering creates inaccuracies in medical databases, which can negatively impact ongoing research on PTSD.[34] In an expert consensus statement, Charney et al[35] called to eliminate those suspected of PTSD malingering from clinical trials in order to lower the risk for underestimation of the observed efficacy of PTSD treatment. Taylor et al[28] state it is unreasonable in clinical trials to expect that cases of malingered PTSD would respond to PTSD treatment. Taylor points out that until malingering is eliminated there will be a risk of underestimating the value of PTSD treatments, leading researchers, healthcare policy makers, and treating clinicians to discard treatments that may actually be useful.
Finally, a validated assessment tool(s) specifically for detection of malingering in PTSD needs to be developed. Despite multiple visits with a patient, a clinician may still miss the signs of malingering. Without a frank confession from the patient or videotaped surveillance that can catch a patient suspected of malingering “in the act,” there is no clinical assessment tool available that has been designed to definitively identify malingering in PTSD.[29]
Evaluation Techniques for Detecting Malingered PTSD
We offer the following guidances on interview techniques, collection of collateral data, and psychometric/physiologic testing that can be integrated into the standard PTSD evaluation process to help the clinician determine if malingering is present.
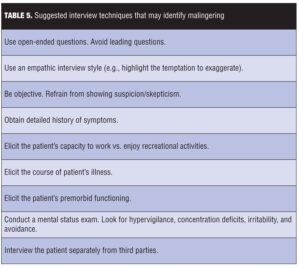
Interview techniques. There are several interview techniques that may help uncover or reveal malingering (Table 5). First, clinicians should begin the interview using open-ended questions (e.g., “How have you been been feeling lately?”) as opposed to leading questions (e.g., “Have you been feeling anxious?” The clinician should avoid interrupting the patient as he or she answers these open-ended questions—this is because the more opportunity a malingerer is given to talk, the more likely the malingerer will contradict his or her own story.[36]
Sometimes an empathic interview style can lead to larger and more easily detected lies.[36] Resnick et al[37] suggest that if malingering is brought to the patient’s attention, it should be done in a sympathetic and understanding way (i.e., the clinician could highlight how understandably tempting it might be to the patient to exaggerate). This gives the patient the chance to admit the truth and “save face.”[3,37] If malingering is suspected, however, it is in the clinician’s best interest to refrain from showing suspicion and to proceed with the evaluation in an objective manner free of verbal or nonverbal communications of skepticism. Knoll[12] warns that failure to do so might cause the patient to become defensive or perceive a need to exaggerate symptoms and thwart efforts to detect evidence of malingering.
Hall[3] states that it is important to obtain a detailed patient history, which, in addition to medical history, can include school grades, work evaluations, and psychological tests that can be compared to the self-report for confirmation. A malingerer may be able to easily recite the DSM symptoms of PTSD, but may have difficulty elaborating on the symptoms with convincing personal life details. Fabricated symptoms are more likely to have a vague quality.[12] Additionally, distinguishing a patient’s capacity to work versus his or her ability to enjoy recreation can be very revealing. A detailed description of the course of the patient’s PTSD illness should also be obtained. The clinician should be suspicious in cases where there has been no improvement in the patient’s condition over time. It will also be important later in the interview, when questions become more specific and less open, to gain an appreciation for the patient’s premorbid functioning.[9]
As one interviews the patient, special attention should be paid to evidence of concentration deficits, hyper-vigilance, irritability, and avoidance (especially avoidance of trauma-related topics during the interview), which are symptoms of true PTSD. A mental status exam should be part of the interview process to detect the presence of these symptoms. It should be noted that individuals who have survived a traumatic experience are often more willing to share their feelings and experiences with fellow survivors than with family members or clinicians initially. Thus, a reduced level of detail may be provided by fellow survivors/victims to the clinician when gathering history compared to details provided by family members or other clinicians, which may indicate avoidance behavior in the fellow survivor/victim as opposed to unreliability in the story.[3]
Knoll et al[12] advises that the patient be interviewed alone, without the presence of any third parties. Third-party presence 1) precludes those individuals as independent sources of verification for the patient’s history and symptoms; and (2) reduces the possibility that a patient will acknowledge malingering if the psychiatrist chooses to confront the issue.[12]
Collateral data (Table 5). Knoll et al[12] report that collection of collateral data is a critical step in offsetting the subjectivity of self-reported PTSD symptoms. To be most helpful, collateral data should be gathered before the evaluation so that patient can be queried on any contradictions between self-reported history and the records on hand. This is especially important given the phenomenon of biased retrospective recall in trauma victims, in which individuals who allege greater PTSD symptom severity amplify their memory for the traumatic event over time.[38] Collateral data should include police reports on the traumatic event and any eye witness statements, if available. Past mental health records should be reviewed with particular attention paid to actual progress notes versus summary letters (as summary letters written by the treating physician may be unconsciously biased).
If medical records are reviewed, the clinician should keep in mind primary care health records have been found to underestimate the occurrence of psychiatric disorders. Employment files and tax returns also may give perspective to the patient’s daily functioning, (e.g., ability to hold a job). In interviewing spouses, coworkers, close friends, and family members for corroborating (or contradicting) evidence of the patient’s self-reported history and symptoms, it should be kept in mind that they may also stand to benefit from the patient’s claims, and thus are not always reliable. For combat veterans, military records and eye witness accounts are among the only ways to verify validity of a stressor; however, third party accounts are hard to acquire and military records can be easily forged. The DD214 form or discharge paperwork that is used most commonly to verify military service can be easily forged. Knoll et al[12] suggest two ways to avoid receiving forged documents: 1) obtain military records yourself directly from the National Personnel Records Center in St. Louis, Missouri; and 2) consult with a confirmed veteran and/or other military personnel who are familiar with the traumatic event and/or the PTSD?claimant.
Psychometric/physiologic testing. Psychometric testing. While there is no gold standard method or single instrument, thus far, for detecting malingering PTSD, a few tests have been validated as reliable for the general detection of malingering. These include the Structured Interview of Reported Symptoms (SIRS), the Minnesota Multiphasic Personality Inventory, Second Edition (MMPI-2), and the Miller Forensic Assessment of Symptoms Test (M-FAST).[12,39,40]
The SIRS,[12] which detects malingered psychiatric illness, takes 30 to 60 minutes to administer. It detects malingering through use of questions about rare symptoms, uncommon symptom pairing, atypical symptoms, and other indices of excessive symptom reporting. It has shown consistently high accuracy in detection of malingering with inpatient, forensic, and correctional populations.[12]
The MMPI-239 is the test used most frequently to detect malingering. Its most commonly analyzed scales are the F-scale and F-K index. Psychiatrists using this test need to consult the literature to determine the cutoff scores that constitute a positive test.[12,39]
The M-FAST[40] is a brief and reliable screen for malingered mental illness, and has an administration time of 10 to 15 minutes. It measures rare symptom combinations, excessive reporting, and atypical symptoms.
The current gold standard in PTSD assessment is the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5), a 30-item structured interview.[41]
Physiologic testing. To date, physiologic testing for PTSD has primarily been used for research purposes but conceivably could be used in clinical practice. Currently, the two most well studied psycho-physiologic methods are script-driven imagery[42,43] and sudden loud tones.[44]
In the script-driven method, subjects engage in script-driven mental imagery of their traumatic event while certain physical responses are measured and analyzed together with the patient’s self-report responses to the Responses to Script-Driven Imagery Scale (RSDI). Research using script-driven mental imagery has shown that severity of state posttraumatic symptoms (e.g., avoidance and dissociation) positively correlates with certain neural activiation.[43]
Using the sudden loud tones method, subjects are exposed to sudden (unexpected) loud tones while heart rate, skin conductance, and orbicularis oculi electromyogram responses are measured. Research using sudden loud tones has shown that larger heart rate responses to sudden, loud tones represent an acquired sign of PTSD.[44]
Although psychometric and psycho-physiologic methods of assessment are helpful when assessing for genuine or malingered PTSD, they cannot be used as the sole determinant of whether a patient is malingering and should be interpreted in the context of a comprehensive evaluation.[12]
Integration of Findings
Without an admission by the patient, the detection of malingering is a probabilistic judgment by the clinican based on the information collected from various sources during the evaluation process of the patient. At times, inconsistencies will require collecting additional information to get a clearer picture. Rather than administering a full battery of malingering assessments, which would be time consuming and expensive, Taylor[29] suggests that clinicians start with the 5- to 10-minute M-FAST and followed by a full diagnostic interview. Next, Taylor recommends that available collateral data, such as previous clinical records, be reviewed, and informants, such as spouses, be interviewed. For those patients in whom such methods provide hints of malingering, Taylor[29] then suggests conducting a more in-depth psychometric evaluation using SIRS, MMPI-2, or both. Finally, if measures up to this point are still insufficient to confidently determine whether malingering is present, Taylor[29] suggests using psycho-physiologic methods (e.g., script-driven imagery, sudden loud tones).
Taylor[29] warns that throughout the process of evaluation, the clinician should be wary of his or her own biases that may influence decisions. Before reaching a final decision on whether a patient is malingering PTSD, Taylor[29] suggests that the clinician draw four boxes on a piece of paper, and then create four lists, one per box, of the following: 1) evidence for genuine PTSD, 2) evidence against genuine PTSD, 3) evidence for malingering, and 4) evidence against malingering. The clinician should then examine each list of evidence as objectively as possible before reaching a final decision. If a clinician suspects a case of malingering but is unwilling to make such a determination, Taylor[29] suggests using a multidisciplinary team approach in which the team uses the available evidence to arrive at a consensus regarding the likelihood of malingering. If malingering is determined to exist, the clinician and/or treatment team will then need to devise a plan to manage the malingering patient.[24]
Conclusion
Malingered PTSD has become a growing concern primarily due to the subjective self-report nature of PTSD symptoms. The most prominent reason patients malinger PTSD is for the financial incentives. Given the negative impact malingered PTSD can have on physician-patient relationships, the economy, the research on PTSD, and on the malingerer him- or herself, it is of high importance that malingered PTSD be identified and managed separately from those patients with true PTSD. We recommend incorporating malingering assessment into all PTSD evaluations. We believe by careful and objective evaluation of information collected via specific interview techniques, collateral data, and psychological testing, clinicians should be able to identify those patients who are truly suffering from PTSD and those who are malingering the disorder, with the ultimate goal being proper and effective treatment for all patients (Figure 1).
References
1. American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders, Third Edition. Washington, DC: American Psychiatric Press Inc.; 1980.
2. Guriel J, Fremouw W. Assessing malingered posttraumatic stress disorder: a critical review. Clin Psychol Rev. 2003;23:881–904.
3. Hall R, Hall R. Malingering of PTSD: forensic and diagnostic considerations, characteristics of malingerers and clinical presentations. Gen Hos Psychiatry. 2006;28:525–535.
4. McHugh P, Treisman G. PTSD: a problematic diagnostic category. J Anxiety Disorders. 2007;21(2):211–222.
5. Wilson J. The historical evolution of PTSD diagnostic criteria: from Freud to DSM-IV. J Trauma Stress 1994;7(4):681–698.
6. Hall R, Hall R. Detection of malingered PTSD: an overview of clinical, psychometric, and physiological assessment: where do we stand? J Forensic Sci. 2007;52(3):717–725.
7. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Press Inc;, 2014.
8. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Arlington, VA: American Psychiatric Press Inc., 2000.
9. Ingram TA, Dowben JS, Froelich KD, Keltner NL. Biological perspectives: detecting malingering of post-traumatic stress disorder (PTSD) in adults. Perspect Psychiatr Care. 2012;48(2):70–75.
10. Kilpatrick D, Resnick HS, Milanak ME, et al. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013 Oct;26(5):537-47.
11. Miller MW, Wolf EJ, Kilpatrick DG, et al. The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in U.S. national and veteran samples. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;6(5).
12. Knoll J, Resnick P.J. The detection of malingered posttraumatic stress disorder. Psychiatr Clin N Am 2006;29:629–647.
13. Olson W. The Litigation Explosion. New York: Dutton; 1991.
14. Rogers R. Diagnostic, explanatory, and detection models of Munchausen by proxy: extrapolations from malingering and deception. Child Abuse & Neglect. 2004;28(2):225–238.
15. Rogers R, Sewell KW, Goldstein A. Explanatory models of malingering: A prototypical analysis. Law Hum Behav. 1994;18:543–552.
16. Blanchard EB, Hickling EJ, Malta LS, et al. Prediction of response to psychological treatment among motor vehicle accident survivors with PTSD. Behavior Therapy. 2003;34(3):351–363.
17. Resnick PJ. Malingering of posttraumatic disorders. In: Rogers R (ed). Clinical assessment of Malingering and Deception, Secon Edition. New York: Guilford Press; 2003:130–152.
18. Lees-Haley PR. MMPI-2 base rates for 492 personal injury plaintiffs: Implications and challenges for forensic assessment. J Clin Psychol. 1997;53:745–755.
19. McHugh PR, Treismann G. PTSD: a problematic diagnostic category. J Anxiety Disorder. 2007;21:211–222.
20. Rosen G, Powel J. Use of a symptom validity test in the forensic assessment of posttraumatic stress disorder. J Anxiety Disorder. 2003; 17(3):361–367.
21. Guriel J, Fremouw W. Assessing malingered posttraumatic stress disorder: a critical review. Clin Psychol Rev. 2003;23:881–904.
22. Lees-Haley PR. Efficacy of MMPI-2 validity scales and MCMI-II modifier scales for detecting spurious PTSD claims: F, F_K, Fake Bad Scale, Ego Strength, Subtle–Obvious subscales, DIS, and DEB. J Clin Psychol. 1992;48, 681–689.
23. Burkett B, Whitley G. Stolen Valor: How the Vietnam Generation was Robbed of its Heroes and its History. Dallas, TX: Verity Press; 1998.
24. Elhai JD, Gold PB, Sellers AH, Dorfman WI. The detection of malingered posttraumatic stress disorder with MMPI-2 Fake Bad indices. Assessment. 2001;8:221–236.
25. Taylor S, Frueh BC, Asmundson GJG. Detection and management of malingering in people presenting for treatment of posttraumatic stress disorder: methods, obstacles, and recommendations. J Anxiety Disorder. 2007;21:22–41.
26. Lacoursiere RB. Diverse motives for fictitious post-traumatic stress disorder. J Traumatic Stress. 1993;6:141–149.
27. Baer RA, Miller J. Underreporting of psychopathology on the MMPI-2: a meta-analytic review. Psychologic Assess. 2002;14:16–26.
28. Melton GB, Petrila J. Poythress NG, Slobogin C. Psychological Evaluations for the Courts, Second Edition. New York: Guilford Press; 1997.
29. Taylor S. Clinician’s Guide to Treating PTSD: A Cognitive-Behavioral Approach. New York: Guilford; 2006.
30. Taylor S, Thordarson D. Behavioral treatment of posttraumatic stress disorder associated with recovered memories. Cognit Behav Ther. (2002)31:8–17.
31. McNally RJ. Remembering trauma. Cambridge, MA: Harvard University Press; 2003.
32. LoPiccolo CJ, Goodkin K, Baldewicz TT. Current issues in the diagnosis and management of malingering. Ann Med. 1999;31:166–174.
33. Oboler S. Disability evaluations under the Department of Veterans Affairs. In: Rondinelli RD, Katz RT (eds). Impairment Rating and Disability Evaluation. Philadelphia, PA: W. B. Saunders; 2000:187–217.
34. Rosen GM. DSM’s cautionary guideline to rule out malingering can protect the PTSD data base. J Anxiety Disorders. 2006;20:530–535.
35. Charney DS, Davidson JRT, Friedman M, et al. A consensus meeting on effective research practice in PTSD. CNS Spectrums. 1998;3(Suppl. 2):7–10.
36A. Primary Psychiatry. Determination of malingering in disability evaluations. December 1, 2005. http://primarypsychiatry.com/determination-of-malingering-in-disability-evaluations/. Accessed February 1, 2015.
36. Wiley S. Deception and detection in psychiatric diagnosis. Psychiatric Clin North Am. 1998;21(4):869–893.
37. Resnick P. Guidelines for the evaluation of malingering in posttraumatic stress disorder. In: Simon R (ed). Posttraumatic stress disorder in litigation: guidelines for forensic assessment. Washington, DC: American Psyciatric Press Inc.; 1995:117–134.
38. Harvey A, Bryant R. Memory for acute stress disorder and posttraumatic stress disorder: a 2-year prospective study. J Nerv Ment Dis. 2000;188:602–607.
39. Graham JR. MMPI-2: Assessing Personality and Psychopathology. New York: Oxford Press; 2000.
40. Ahmadi K, Lashani Z, Afzali MH, et al. Malingering and PTSD: detecting malingering and war-related PTSD by Miller Forensic Assessment of Symptoms Test (M-FAST). BMC Psychiatry. 2013;13(154):1–5.
41. Weathers FW, Blake DD, Schnurr PP, et al. Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). US Department of Veterans Affairs. PTSD: National Center for PTSD. Professional. http://www.ptsd.va.gov/professional/assessment/adult-int/caps.asp. Accessed February 1, 2015.
42. Hopper JW, Frewen PA, van der Kolk BA, Lanius RA. Neural correlates of reexperiencing, avoidance, and dissociation in PTSD: symptom dimensions and emotion dysregulation in responses to script-driven trauma imagery. J Trauma Stress. 2007;20(5):713-25.
43. Hopper JW, Frewen PA, Sack M, et al. The Responses to Script-Driven Imagery Scale (RSDI): assessment of state posttraumatic symptoms for psychobiological and treatment research. J Psychopathol Behav Assess. 2007;29:249–268.
44. Orr SP, Metzger LJ, Lasko NB, et al. Physiologic responses to sudden, loud tones in monozygotic twins discordant for combat exposure: association with posttraumatic stress disorder. Arch Gen Psychiatry. 2003;60(3):283–288.