 by Samuel R. Weber, MD
by Samuel R. Weber, MD
Dr. Weber is with Intermountain Healthcare in Logan, Utah.
FUNDING: No funding was provided for this study.
DISCLOSURES: The author has no conflicts of interest relevant to the content of this article.
ABSTRACT: Depersonalization and derealization symptoms are common and often transient. Recurrent, persistent symptoms can result in a diagnosis of depersonalization/derealization disorder (DDD). This is a diagnosis with little evidence available regarding effective interventions, and there are currently no pharmacological treatments for DDD approved by the United States Food and Drug Administration (FDA). Here, we reported a case of an adult female whose presentation was consistent with DDD. Her DDD symptoms notably reduced after treatment with mixed amphetamine salts. We also reviewed the limited research examining the efficacy of lamotrigine, benzodiazepines, antidepressants, naltrexone, and antipsychotics in DDD. Given the lack of evidence-based interventions for patients with DDD, additional research into the potential benefit of using psychostimulants might be warranted.
KEYWORDS: Dissociative disorders, depersonalization, derealization, psychostimulants
Innov Clin Neurosci. 2020;17(45–48)
Dissociative symptoms are common in the general population and can include experiences of depersonalization and derealization. The Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) defines depersonalization as “experiences of unreality, detachment, or being an outside observer with respect to one’s thoughts, feelings, sensations, body, or actions (e.g., perceptual alterations, distorted sense of time, unreal or absent self, emotional and/or physical numbing).” Derealization is defined as encompassing “experiences of unreality or detachment with respect to surroundings (e.g., individuals or objects are experienced as unreal, dreamlike, foggy, lifeless, or visually distorted).”1 One survey found a one-year prevalence of 19 percent for depersonalization symptoms and 14 percent for derealization symptoms. Another study found that 46 percent of college students had at least one episode of depersonalization in the past year. These symptoms might be transient and appear to occur most commonly among adolescents and young adults. Depersonalization and derealization symptoms can be triggered by seizures, migraines, head injury, and illicit drug use.2
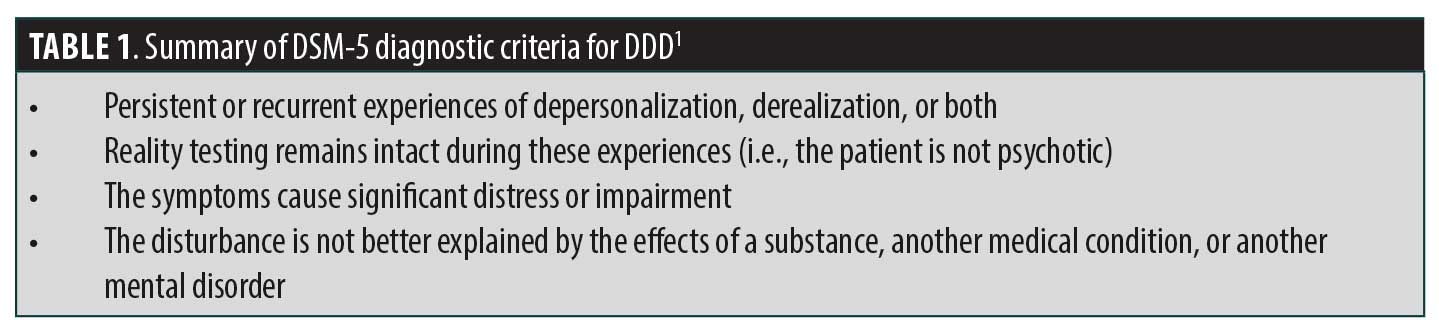
When symptoms of depersonalization and/or derealization become recurrent or persistent, a person might be diagnosed with depersonalization/derealization disorder (DDD). This diagnosis was formerly termed depersonalization disorder under DSM-4. For the sake of brevity, when referencing either diagnosis, the abbreviation DDD will be used in this report. The DSM-5 criteria for diagnosing DDD are summarized in Table 1. DDD is a disorder with a scant evidence base regarding effective interventions, and the diagnosis currently lacks any medication interventions approved by the United States Food and Drug Administration (FDA). In this report, we present the case of an adult female patient who showed symptoms consistent with DDD and responded well to treatment with mixed amphetamine salts.
Case Presentation
A 35-year-old woman seen by her primary care physician (PCP) for medication management presented to the psychiatric clinic to establish care. The patient provided written authorization to have this case report published. Patient identity was disguised by omission or alteration of nonessential information. Notes from her PCP indicated a concern for anxiety and, potentially, a dissociative disorder. A physical examination and laboratory workup were unrevealing. The patient had previously been prescribed 150mg of venlafaxine XR daily and 0.5mg of clonazepam twice daily for anxiety. During the initial psychiatric interview, the patient reported that her primary concern involved experiencing symptoms of dissociation.
The patient’s dissociative symptoms had begun in high school and described these experiences as feeling like her surroundings were “unreal” or “off.” Feeling as though she was “inside [her] head,” watching herself and difficulty distinguishing dreams from real life were also reported. Symptoms tended to worsen in the context of severe life stressors such as the death of a family member. The symptoms were described as pervasive, “all day, every day.”
The patient did endorse some depressive symptoms upon psychiatric review, but they were insufficient for a major depressive disorder diagnosis. The patient also endorsed symptoms consistent with generalized anxiety disorder and reported occasionally hearing a female voice speak to her in times of elevated stress or anxiety but wondered aloud whether this might have been her own voice. Otherwise, reality testing was intact, and the patient did not exhibit other symptoms consistent with a thought disorder and did not meet criteria for posttraumatic stress disorder (having no history of abuse or trauma), and presentation was not consistent with borderline personality disorder. The patient was screened for attention-deficit hyperactivity disorder (ADHD) using the Adult ADHD Self-Report Scale and clinical interview but did not meet criteria for this diagnosis either.
In terms of psychiatric history, the patient had been seen by a psychiatrist in the past but had never before engaged in psychotherapy and denied any psychiatric hospitalizations and any history of suicide attempts or self-injury. Family history was notable only for a first-degree relative having emotional problems who had apparently never received a formal diagnosis. In terms of social history, the patient graduated high school, worked part-time outside of the home, and lived with her spouse and four children. There wasn’t any current or past history of substance abuse.
The patient’s mental status examination was mostly within normal limits. General appearance was normal; she was alert and oriented to person, place, time, and situation; recent and remote memory appeared to be intact; and speech was normal. Her mood was depressed and anxious, but affect was full and reactive. Thought process was logical and goal-directed, and concentration appeared intact. The patient’s thought content was notable for the aforementioned difficulty distinguishing reality from dreams as well as her occasional negative self-talk. She denied both suicidal and homicidal ideation.
At the conclusion of the initial appointment, the patient was diagnosed with unspecified depressive disorder, generalized anxiety disorder, and DDD. The patient reported some benefit from the venlafaxine prescribed by a PCP but found it didn’t control her symptoms. She used one tablet of clonazepam on average one to two times weekly and noted that a previous psychiatrist had, at one time, prescribed mixed amphetamine salts, which had been a helpful intervention. The patient was then advised to discontinue the use of clonazepam, continue use of venlafaxine, start lamotrigine with a target dose of 100mg daily, and was referred to begin a course of cognitive–behavioral therapy.
After one week of taking the lamotrigine, the patient contacted the office complaining of severe headaches and itching skin with the starting dose of 25mg daily. We instructed the patient to discontinue the lamotrigine and increase the dose of venlafaxine to 225mg daily.
At the follow-up appointment nearly two months later, the patient reported feeling “happier” and less anxious with the higher dose of venlafaxine. She had begun psychotherapy with a focus on “living in the present.” Despite these improvements, the patient continued to complain of pervasive dissociative symptoms, commenting: “looking at you right now, I feel like I’m in a movie.” She added, “I can live like this, but I don’t enjoy it,” and expressed interest in a retrial of mixed amphetamine salts given her past benefit from the medication. We agreed to a trial and a prescription for 10mg of extended-release mixed amphetamine salts daily was given.
At the next follow-up appointment nearly two months later, the patient reported a rapid improvement in her dissociative symptoms since beginning the mixed amphetamine salts. The dose was titrated up to 15mg daily after the first month, then up to 20mg daily roughly three months later. Although dissociative symptoms did not fully resolve, the patient reported a notable reduction in the frequency and intensity of her symptoms as well as improved functioning and quality of life.
Discussion
This case demonstrates a potential benefit from the use of psychostimulant medication in a condition for which no FDA-approved medications exist. When a patient presents complaining of dissociative symptoms, the first step is to establish a clear diagnosis. It is important to rule out diagnoses for which dissociation can be a symptom, including posttraumatic stress disorder and borderline personality disorder. Psychotic disorders should be given consideration, as reported symptoms of depersonalization/derealization can sound similar to delusions or hallucinations. The presence of depersonalization/derealization symptoms among psychiatric in patients with schizophrenia have been reported at rates ranging from 23 to 66 percent.3 The presence of intact reality testing regarding the depersonalization/derealization experiences helps to differentiate DDD from psychotic disorders.1 Substance abuse must also be ruled out, particularly in the case of a patient specifically requesting a prescription for a controlled substance. In patients for whom psychostimulant medication has provided benefit in the past, ADHD should also be considered. If there is a prominence of somatic symptoms, conversion disorder should be considered given that dissociative symptoms are common in this context.1 Accuracy and consistency in diagnosis can be challenging, and some physicians express disbelief in the existence of certain dissociative disorders.4 However, the potential costs of DDD on the individual and on society are not insignificant. Patients with DDD might have severe impairments in interpersonal and occupational functioning.1,2 Underscoring the need for effective treatments is the established link between dissociative disorders and an increased risk of self-harm and suicidality.5
Psychotherapy should be considered in the treatment of DDD, although the evidence base supporting this to date is small and no studies have yet compared therapeutic modalities. One study showed benefit from using cognitive–behavioral therapy, noting improvements in measures of depersonalization/derealization severity.6 Another study suggested that mindfulness-based approaches could reduce the severity of depersonalization.7 Other psychotherapies applied in the treatment of DDD include psychodynamic treatment and supportive psychotherapy. There is insufficient data to support the use of eye movement desensitization and reprocessing at present.2 Our patient did note some benefit from participation in psychotherapy.
As mentioned above, no FDA-approved treatments exist for the management of DDD. There is limited evidence supporting the use of several medications off-label. A randomized, controlled trial suggested some promising results might be achieved when using lamotrigine in patients with DDD, but this article was later retracted by the journal due to concerns about plagiarism.8 A retrospective study of 32 patients with DDD reported on a significant number of patients who responded to lamotrigine augmentation as measured by a reduced Cambridge Depersonalization Scale score.9 However, a placebo-controlled, cross-over trial of lamotrigine did not demonstrate the superiority of lamotrigine over a placebo.10 In our case, the patient was unable to tolerate even a small dose of lamotrigine due to problematic side effects, so no comment can be made regarding its efficacy (or lack thereof) in this instance.
In a retrospective report of 35 patients with DDD taking benzodiazepines, 10 reported feeling “definitely better,” eight reported feeling “slightly better,” and 17 reported feeling “[the] same/worse.”11 There is some concern that the use of benzodiazepines can exacerbate dissociative symptoms,12 which contributed to the decision to discontinue clonazepam in our case.
Regarding antidepressants, one uncontrolled trial showed that two of seven patients with DDD experienced improvement following an eight-week course of treatment with clomipramine,13 but a randomized trial comparing fluoxetine with placebo in 50 patients did not demonstrate any difference between the two groups.14 In our case, the use of the serotonin–norepinephrine reuptake inhibitor venlafaxine did produce benefits for anxiety and depressive symptoms, but the patient’s dissociative symptoms persisted even at high doses.
One uncontrolled trial indicated an average 30-percent reduction in symptoms among 14 subjects treated with naltrexone.15 In a sample of patients with DDD where 13 were treated with antipsychotics and seven were treated with atypical antipsychotics, 100 percent of the patients reported feeling the same or worse after treatment.11 Our patient did not receive a trial of naltrexone or antipsychotics.
Ours is not the first case report to note benefits from the use of psychostimulant medication in the treatment of a dissociative disorder. An uncontrolled, retrospective study noted that, among nine patients with DDD receiving unspecified stimulant medication, two reported a slight improvement and the remaining seven reported feeling the same or worse.11 One case report documented a young woman who had attempted suicide and was diagnosed with DDD. After multiple medication trials with limited success, she was eventually treated with long-acting methylphenidate titrated up to a dose of 54mg, which produced a dramatic improvement in her depersonalization symptoms. Although the symptoms never completely resolved, treatment resulted in significant improvements in her academic/occupational functioning.16 Another case report discussed a female patient with a history of complex emotional illness with significant dissociative symptoms, including difficulty recalling many details of her daily life. No specific dissociative disorder diagnosis was described in this report but, following a trial of extended-release mixed amphetamine salts, (initially 10mg daily, later 10mg three times daily) there was marked improvement in the patient’s dissociative symptoms, including her ability to recall recent events. Despite this improvement, though, some dissociative symptoms persisted.17 Our case is unique in its use of mixed amphetamine salts specifically for DDD. Similar to in other case reports, our patient achieved significant but incomplete improvements in the patient’s DDD symptoms with stimulant use. Given a high degree of co-occurrence between dissociative disorders and psychotic disorders,18 special caution should be taken if psychostimulant therapies are considered, since these medications can exacerbate psychosis. Fortunately, our patient did not experience any psychotic symptoms when taking mixed amphetamine salts.
Psychostimulants such as mixed amphetamine salts potentiate dopaminergic and noradrenergic neurotransmission in the brain. Chronic stress has been shown to lead to a depletion of dopamine systems. This has been posited as a possible mechanism by which psychostimulants can alleviate symptoms of DDD—that is, by correcting a hypodopaminergic state induced by chronic stress.17
Conclusion
This case demonstrates that a patient with DDD, an illness lacking treatments with a solid evidence base and FDA approval, benefited from a trial of mixed amphetamine salts. As with any treatment, the potential benefits of stimulant use must be weighed against the risks, and further research is needed to provide more generalizable results.
References
- American Psychiatric Association, Spitzer R (ed). Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013: 302–306.
- Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s Comprehensive Textbook of Psychiatry, Vol. 1. 9th ed. Philadelphia, PA: Wolters Kluwer Health Lippincott Williams & Wilkins; 2009; 1995–1998.
- Hunter ECM, Sierra M, David AS. The epidemiology of depersonalisation and derealization: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2004;39(1):9–18.
- Coons PM. The dissociative disorders: rarely considered and underdiagnosed. Psychiatr Clin North Am. 1998;21(3):637–648.
- Foote B, Smolin Y, Neft DI, Lipschitz D. Dissociative disorders and suicidality in psychiatric outpatients. J Nerv Ment Dis. 2008;196(1):29–36.
- Hunter EC, Baker D, Phillips ML, et al. Cognitive-behaviour therapy for depersonalization disorder: an open study. Behav Res Ther. 2005;43(9):1121–1130.
- Michal M, Koechel A, Canterino M, et al. Depersonalization disorder: disconnection of cognitive evaluation from autonomic responses to emotional stimuli. PLoS One. 2013;8(9):e74331.
- Aliyev NA, Aliyev ZN. Lamotrigine in the immediate treatment of outaptients with depersonalization disorder without psychiatric comorbidity: randomized, double-blind, placebo-controlled study. J Clin Pscyhopharmacol. 2011;31(1):61–65.
- Sierra M, Baker D, Medford N, et al. Lamotrigine as an add-on treatment for depersonalization disorder: a retrospective study of 32 cases. Clin Neuropharmacol. 2006;29(5):253–258.
- Sierra M, Phillips ML, Ivin G, et al. A placebo-controlled, cross-over trial of lamotrigine in depersonalization disorder. J Psychopharmacol. 2003;17(1):103–105.
- Simeon D, Knutelska M, Nelson D, Guralnik O. Feeling unreal: a depersonalization disorder update of 117 cases. J Clin Psychiatry. 2003;64(9):990–997.
- Gentil JP, Dillon KS, Gillig PM. Psychotherapy and pharmacotherapy for patients with dissociative identity disorder. Innov Clin Neurosci. 2013;10(2):22–29.
- Simeon D, Stein DJ, Hollander E. Treatment of depersonalization disorder with clomipramine. Biol Psychiatry. 1998;44(4):302–303.
- Simeon D, Guralnik O, Schmeidler J, Knutelska M. Fluoxetine therapy in depersonalisation disorder: randomised controlled trial. Br J Psychiatry. 2004;185:31–36.
- Simeon D, Knutelska M. An open trial of naltrexone in the treatment of depersonalization disorder. J Clin Psychopharmacol. 2005;25(3):267–270.
- Foguet Q, Alvarez MJ, Castells E, Arrufat F. Methylphenidate in depersonalization disorder: a case report. Actas Esp Psiquiatr. 2010;39(1):75–78.
- Scarella TM, Franzen JR. Case report: improvement in dissociative symptoms with mixed amphetamine salts. J Trauma Dissociation. 2017;18(5):649–662.
- Renard SB, Huntjens RJ, Lysaker PH, et al. Unique and overlapping symptoms in schizophrenia spectrum and dissociative disorders in relation to models of psychopathology: a systematic review. Schizophr Bull. 2017;43(1):108–121.





