Innov Clin Neurosci. 2025;22(7–9):32–39.
by Ray M. Merrill, PhD, MPH
Dr. Merrill is with the Department of Public Health in the College of Life Sciences at Brigham Young University in Provo, Utah.
FUNDING: No funding was provided for this article.
DISCLOSURES: The author declares no conflicts of interest relevant to the content of this article.
A growing number of studies have linked intoxicating components of cannabis, notably tetrahydrocannabinol (THC), with cognitive impairment. Recent cannabis use (within 24 hours) has an immediate impact on attention, thinking, memory, movement, coordination, and time perception.1 The effects of cannabis on cognitive abilities can also last a long time and may be permanent.2 The Dunedin Study was a prospective cohort study of 1,037 individuals followed from birth in the early 1970s to the age of 38 years. It showed that persistent cannabis use correlated with neuropsychological decline, with adolescent-onset cannabis users showing poorer attention, memory, and learning ability.2 Cessation of cannabis among adolescent-onset users did not fully restore neuropsychological functioning.
Executive function, a set of skills that include proficiency in planning, working memory, adaptable thinking, self-monitoring, self-control, time management, and organization can be compromised by cannabis use. A review article found evidence that cannabis has acute effects (0–6 hours after last use), residual effects (7–20 days after last use), and long-term effects (3 weeks or longer) after last use.3 Specifically, the study found that attention/concentration and working memory tended to be restored over time, but long-term deficits appeared in decision-making, concept formation, and planning. Cannabis has mixed effects on inhibition/impulsivity and verbal fluency in the long-term. The most enduring deficits occur in chronic, heavy cannabis users, but even occasional cannabis users can acutely experience impaired attention/concentration, decision-making, inhibition/impulsivity, and working memory.
Research has shown that the regular use of cannabis during adolescence has adverse cognitive (eg, thinking, reasoning, or remembering) effects. Adverse effects associated with short-term use include impaired short-term memory, impaired motor coordination, altered judgement, and, in high doses, paranoia and psychosis. The effects on long-term or heavy use include altered brain development, poor educational outcome, cognitive impairment (with lower intelligence quotient), diminished life satisfaction and achievement, symptoms of chronic bronchitis, and increased chronic psychosis (including schizophrenia).4–6 Frequent users of cannabis might also have impaired movement speed and balance.7
The National Institute on Drug Abuse summarizes the detrimental effects of cannabis as altered senses, altered sense of time, change in mood, impaired body movement, difficulty with thinking and problem solving, impaired memory, temporary hallucinations, temporary paranoia, delusions, psychosis, and worsening symptoms in patients with schizophrenia.8 Physical effects include breathing problems and increased heart rate.8,9
Despite the known deleterious consequences of cannabis use, especially in adolescent-onset cannabis users, there are certain clinical conditions and symptoms that can be relieved through treatment with the cannabis plant, such as glaucoma, nausea, acquired immunodeficiency syndrome (AIDS)–associated anorexia and wasting syndrome, chronic pain, inflammation, multiple sclerosis, epilepsy, poor sleep quality, high blood pressure, and chemotherapy side effects.6,10–14 Research has also found that cannabis use can lower the risk of obesity.15–19
Although we have learned much about the harms and benefits of cannabis use in recent years, more research is needed to fully understand these effects, especially in the long-term. Important confounders complicate our ability to establish cause-effect relationships (eg, co-occurring use of other drugs, chronic disease, and mental illness). Nevertheless, there has been a movement among United States (US) states and territories to legalize cannabis for personal consumption. Although cannabis is illegal under federal law, most Americans live in an area that has legalized its use. A Pew Research Center study reported that in the US in 2024, 24 states and the District of Columbia have legalized cannabis for recreational and medical use, and another 14 states have legalized the drug for medical use only.20
Many physical and mental illnesses have been linked to difficulty concentrating, remembering, and making decisions. For example, stroke, cerebrovascular, and coronary artery diseases can impair executive function and memory.21–26 Rheumatoid arthritis may have a negative effect on memory, attention, and mental focus.27 Patients with diabetes are at greater risk of cognitive problems.28 Cancer treatments (eg, chemotherapy) can cause difficulty with thinking, concentrating, and memory.29 Epidemiological studies have linked asthma to increased risk of cognitive impairment and dementia.30–32 Furthermore, cognitive impairment is often found in patients with chronic kidney disease.33
Several studies have shown that stress and depression cause changes in the brain that impair memory.34,35 Depression also makes it difficult to pay attention and make decisions.36,37 In a series of 129 cases from the United Kingdom Medical Cannabis Registry, cannabis-based medical products were associated with reduced depression severity at one, three, and six months.38 However, this was not a controlled study, and the study design did not allow for conclusions to be drawn about causality.
Due to the similar effects of cannabis use and chronic diseases on cognitive ability, the current study explored their independent and co-occurring effects on concentrating, remembering, and making decisions in the US population. This is particularly relevant because of the high prevalence of cannabis use and chronic disease today.
Methods
Data. The Behavioral Risk Factor Surveillance System (BRFSS) is a national system of health-related telephone surveys that collects state and territory data about US residents regarding their health-related risks behaviors, chronic health conditions, and use of preventive services. BRFSS completes over 400,000 adult surveys each year. The cross-sectional survey design uses random probability samples of the adult (aged ≥18 years) population. The questionnaire consists of three parts: 1) core questions on demographics and current health-related conditions and behaviors adopted by all states and US territories; 2) optional modules on specific topics (eg, cannabis use) that states may choose to use; and 3) state-added questions developed by states for their own use.39 Overall, the median response rate for participating areas in 2022 was 45.1 percent.40
Survey questions on cannabis use were first added to the BRFSS in 2016 as an optional module. The current study includes participants administered the cannabis use module in the 2022 BRFSS surveys. Participating US states and territories (and current cannabis use in the past month) included Oregon (22.4%), Maine (21.9%), Montana (20.4%), Nevada (19.5%), New Mexico (16.8%), Connecticut (16.0%), Illinois (15.6%), Delaware (13.9%), Guam (13.6%), Virginia (13.1%), Indiana (12.4%), Wisconsin (12.2%), Hawaii (11.8%), Mississippi (13.4%), Virgin Islands (10.4%), North Dakota (9.8%), Nebraska (9.7%), and Wyoming (9.0%); the overall prevalence of cannabis use in the past month was 14.9 percent.41
All participants provided informed consent prior to the interview. Information about the BRFSS survey design, questionnaires, and data collection methods is publicly available.40,41 This study was determined to be exempt from human subjects research review by the author’s institutional review board because BRFSS provides publicly available deidentified data.
Measures. The primary dependent variable was determined from response to the question, “Because of a physical, mental, or emotional condition, do you have serious difficulty concentrating, remembering, or making decisions?”
Cannabis use was determined from the question, “During the past 30 days, on how many days did you use marijuana or cannabis?” Individuals who used cannabis at least one day in the past 30 days were considered monthly cannabis users, and those who used it at least 20 days in the past 30 days were considered daily users.42 The percentage of respondents who did not know, were not sure, or refused to answer was 1.24 percent.
Medical comorbidity was assessed by the question, “Has a doctor, nurse, or other health professional ever told you that you had any of the following?” with answers including stroke, heart attack, coronary heart disease, asthma, chronic obstructive pulmonary disease (COPD), diabetes, arthritis, kidney disease, skin cancer, other types of cancer, and depressive disorder. Any medical condition was based on responding that they had one or more of these conditions. The number of medical conditions was also categorized as zero, one, two, or three or more. Other variables included sex (male, female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and other), education level (<high school, high school, some college, and college), annual income (<$25,000, $25,000–49,999, $50,000–74.999, and ≥$75,000 US dollars), employment status (employed, not employed, not in workforce), and smoked over 100 cigarettes in lifetime (yes, no).
Statistical analysis. Difficulty concentrating, remembering, or making decisions; cannabis use; medical conditions; and other variables were estimated by taking the survey stratum, primary sampling units, and sampling weights into consideration. Differences in difficulty according to the status of chronic medical conditions, cannabis use, and other variables were assessed by the Rao-Scott χ2 test. Multiple logistic regression was used to identify whether there were associations after adjusting for age, sex, marital status, race/ethnicity, education, annual household income, employment, smoking, legalization, and any medical insurance. Variable effects were assessed for statistical significance in the model using the F test. Statistical significance was based on two-sided tests and the 0.05 level. Statistical analyses were conducted using Statistical Analysis System (SAS) software, version 9.4 (SAS Institute, Inc.; Cary, North Carolina, 2012).
Results
The estimated prevalence of monthly cannabis use among adults in the US was 14.9 percent (standard error [SE]: 0.24%) and that of daily cannabis use was 7.4 percent (SE: 0.18%), based on the 2022 BRFSS survey. The prevalence of one or more chronic medical conditions among adults was 59.2 percent (SE: 0.32%). The prevalence of monthly cannabis use was significantly higher for those with a chronic medical condition compared to those without a chronic medical condition (16.3% [SE: 0.33%] vs.12.9% [SE: 0.36%], Rao-Scott p<0.00001). The prevalence of daily cannabis use was also higher for those with a chronic medical condition versus those without one (8.4% [SE: 0.26%] vs. 6.0% [SE: 0.26%], Rao-Scott p<0.0001). The prevalence of monthly cannabis use tended to increase with the number of chronic medical conditions (12.9% for 0, 15.9% for 1, 17.0% for 2, and 16.2% for ≥3; Rao-Scott p<0.0001). Corresponding values for daily use were 6.0, 8.0, 8.9, and 8.9 percent, respectively (Rao-Scott p<0.0001).
Chronic medical conditions impact the ability to concentrate, remember, or make decisions. The prevalence of cognitive difficulty concentrating, remembering, or making decisions because of physical, mental, or emotional conditions among adults was 12.7 percent (SE: 0.21%). The prevalence of such difficulty was higher for those with a chronic medical condition compared to those without a chronic medical condition (17.6% [SE: 0.31%] vs. 5.7% [SE: 0.25%], Rao-Scott p<0.0001).
The combined influence of using cannabis and having a chronic medical condition may uniquely influence ability to concentrate, remember, or make decisions. The prevalence of such cognitive difficulty was higher for those who used cannabis in the past month and had a chronic medical condition compared to those who used cannabis in the past month but did not have a chronic medical condition (24.4% [SE: 0.731%] vs. 10.7% [SE: 0.21%], Rao-Scott p<0.0001). Corresponding results for daily cannabis users were 29.1 percent (SE: 1.12%) and 11.4 percent (SE: 0.21%), respectively (Rao-Scott p<0.0001).
Cognitive difficulty concentrating, remembering, or making decisions is presented according to having a chronic medical condition and cannabis use in Table 1. Greater cognitive difficulty for those with a chronic medical condition was accentuated by cannabis use; daily cannabis use (vs. nonuse) was associated with 145-percent higher prevalence of cognitive difficulty, and monthly cannabis use (vs. nonuse) was associated with a 76-percent higher prevalence of cognitive difficulty. For those without a medical condition, the prevalence of cognitive difficulty was 183- and 97-percent higher in daily and monthly cannabis users (vs. nonusers), respectively.
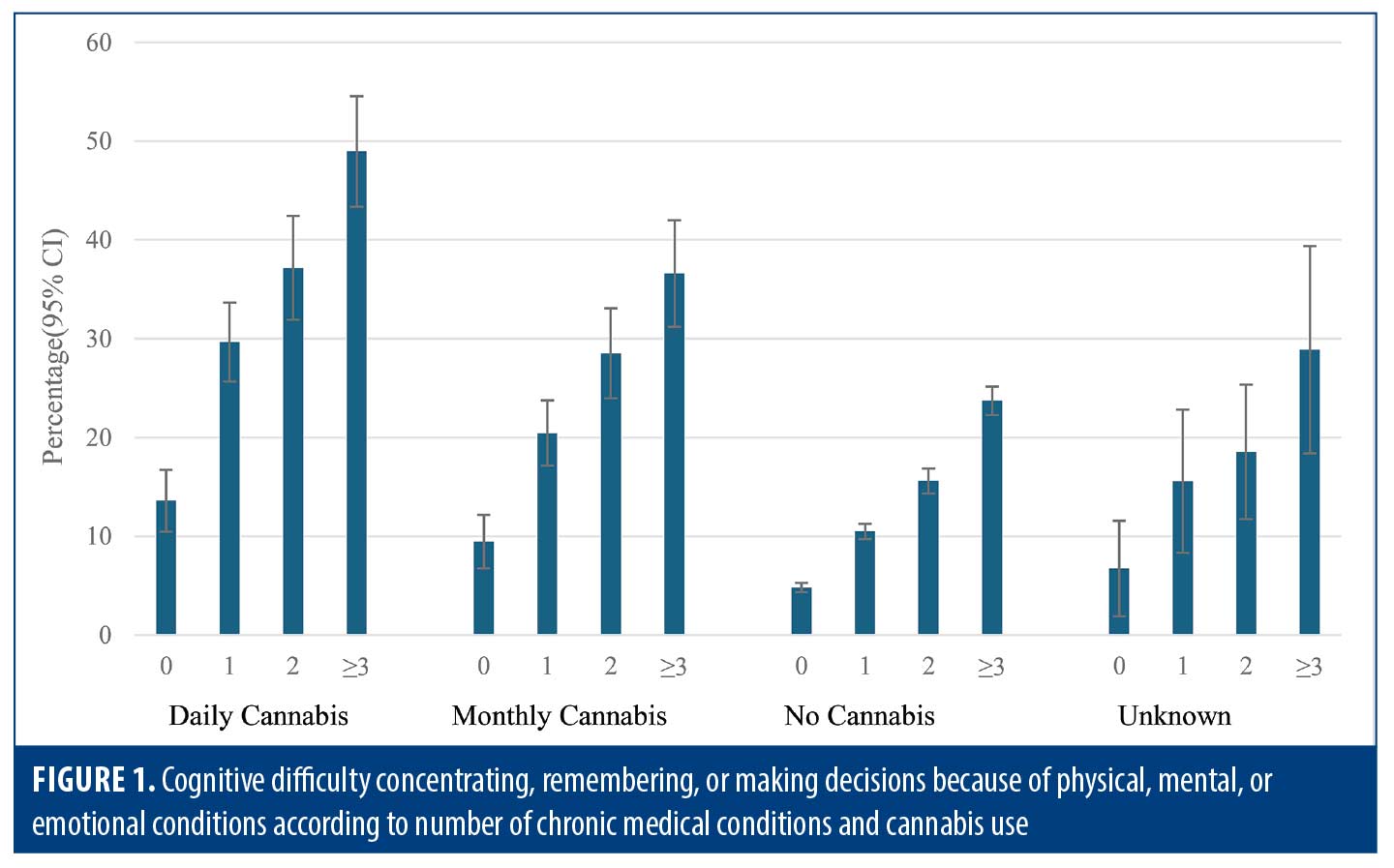
The prevalence of cognitive difficulty concentrating, remembering, or making decisions significantly increased with the number of chronic medical conditions and was more pronounced among daily and then monthly cannabis users (Figure 1). Moving from zero to three or more chronic medical conditions resulted in an increase of cognitive difficulty by 260 percent for daily cannabis users, 287 percent increase for monthly cannabis users, and 329 percent increase for noncannabis users.
A fully adjusted logistic regression model identified the association between cognitive difficulty concentrating, remembering, or making decisions and chronic medical conditions, cannabis use, and other variables (Table 2). Both chronic medical conditions and cannabis use independently correlated with difficulty, after adjusting for several variables. Presence of a chronic medical condition had the strongest association with cognitive difficulty, followed by age, and then cannabis use.
Cognitive difficulty concentrating, remembering, or making decisions by specific chronic medical condition and cannabis use appears in Table 3. Those with a chronic medical condition (vs. no condition) had a higher prevalence of cognitive difficulty (513% for depression, 373% for COPD, 348% for stroke, 280% for asthma, 272% for kidney disease, 254% for heart attack, 216% for coronary heart disease, 200% for arthritis, 163% for diabetes, 132% for nonskin cancer, and 71% for skin cancer). Cannabis use in the past month significantly increased difficulty for each chronic medical condition. Compared with the reference group for each chronic medical condition, the increase of difficulty with daily cannabis or monthly cannabis use ranged considerably; for example, the increase was 58 percent and 33 percent for depression and 229 percent and 80 percent for nonskin cancer, respectively. There was an inverse association between level of difficulty concentrating, remembering, or making decisions for chronic medical conditions and the additional difficulty attributed to monthly or daily cannabis use (Pearson correlation coefficient: –0.682, p=0.021). The increase in difficulty for monthly or daily cannabis users was generally less pronounced than for those with no chronic medical conditions.
Discussion
Cannabis use and chronic diseases both negatively affect perceived cognitive difficulty concentrating, remembering, or making decisions. The current study explored their independent and co-occurring effects on cognitive difficulty concentrating, remembering, and making decisions. This study comes at a time of rising cannabis use and high prevalence of chronic medical conditions in the US population.
In general, cannabis use is increasing as more and more states and territories in the US opt for legalization.43 In the current study, the prevalence of cannabis use was significantly higher for those with a chronic medical condition. This result is consistent with findings from a national survey from 2016 to 2017 of cannabis use among individuals in the US with chronic medical conditions.44
The prevalence of cognitive difficulty concentrating, remembering, or making decisions was significantly higher for those with a chronic medical condition. This result is consistent with several studies showing an association between medical conditions, such as stroke, rheumatoid arthritis, cancer, asthma, chronic kidney disease, stress, and depression, and increased risk of impaired cognitive function.21–37 While cannabis can be used for medical reasons, such as chronic pain, inflammation, depression, multiple sclerosis, epilepsy, improving sleep quality, weight loss, high blood pressure, and managing chemotherapy side effects,6,10–19, 38 persistent use is correlated with poorer attention, memory, and learning ability;2 a decline in executive function;3 and other cognitive impairments and adverse physical effects.4–9
Greater cognitive difficulty concentrating, remembering, or making decisions for those with a chronic medical condition was accentuated by cannabis use in this study. The results showed that daily cannabis users (vs. nonusers) had a 145-percent higher prevalence of difficulty and monthly cannabis users (vs. nonusers) had a 76-percent higher prevalence of difficulty. For those without a medical condition, the corresponding higher prevalence of difficulty with daily and monthly cannabis use (vs. nonuse) was 183 percent and 97 percent, respectively. The prevalence of differences in cognitive difficulty among cannabis users versus nonusers was smaller for those with chronic medical conditions, possibly because the baseline rate for the reference group (chronic medical condition, no use) was much higher than the baseline rate in the other reference group (no chronic medical condition, no use). The model also confirmed independent effects of chronic medical conditions and cannabis use on difficulty concentrating, remembering, or making decisions.
The prevalence of cognitive difficulty concentrating, remembering, or making decisions sharply increased with the number of chronic medical conditions. For zero, one, two, or three or more chronic medical conditions, the prevalence of cognitive ability was higher for those who used cannabis daily, followed by monthly, and then never. However, the increase in cognitive difficulty for those with more chronic medical conditions was less pronounced for those who used cannabis daily and more pronounced for those who never used cannabis; this might be because cannabis helped to relieve the symptoms of certain chronic medical conditions and, thus, lowered cognitive difficulty in some patients.
Chronic medical conditions significantly increased the risk of cognitive difficulty concentrating, remembering, or making decisions for each chronic medical condition considered in the study, from a 513-percent higher risk for depression to a 71-percent higher risk for skin cancer. It is well established that depression is associated with poor concentration.45 Memory loss associated with depression may occur because irregular brain activity manifested in depressive symptoms can impact parts of the brain that control memory.46 Corresponding conditions, such as lack of sleep or side effects of antidepressant medication for patients with depression, can also impair the ability to remember.47,48 Furthermore, some of the high risk associated with depression might be because patients with depression tend to underestimate their cognitive performance.49 There is also likely a mood component that can inflate self-reports of cognitive difficulties beyond the influence of a formal diagnosis of depression. Additionally, some medical conditions (eg, stroke, COPD, asthma, heart attack, and coronary heart disease) can restrict blood flow to the brain, reducing needed oxygen and nutrients.50–55
Cannabis use increases cognitive difficulty concentrating, remembering, or making decisions at different levels for the chronic medical conditions considered. It has a smaller effect on depression, possibly because cannabis can help relieve depressive symptoms.38 While cannabis use increases cognitive difficulty concentrating, remembering, or making decisions at a higher level, it is generally more pronounced for those without a chronic medical condition. This is likely because the level of difficulty is comparatively low at the outset for those without a chronic medical condition. It may be that the form of cannabis used for medical conditions is different, but such a claim would require further study.
Limitations. First, because BRFSS data are cross-sectional, causal associations cannot be established. Hence, we do know whether some of the psychological effect of cannabis use is explained by the presence of psychological precursors to cannabis that persisted after use. Further research is needed to consider this using longitudinal data. Second, different areas participated in the cannabis module each year. However, the percentage of participating states legalizing cannabis for medical and recreational purposes was similar to the percentage in the entire US in 2022. Hence, we assume the participating areas are representative of the US. Third, data in this study are self-reported and may be mood- and cognitive-dependent and prone to social desirability bias.56,57 Yet, a systematic review of publications assessing the reliability and validity of BRFSS data found that BRFSS prevalence rates were similar to other national surveys involving self-reports.58 Fourth, the BRFSS does not currently account for the type of cannabis (ie, medical versus recreational, cannabidiol vs. THC) or duration of THC cannabis used, which can impact tolerance for the drug and reduce the effects of its intoxication.59
Conclusion
Cognitive difficulty concentrating, remembering, or making decisions was significantly higher for those with a chronic medical condition. For each chronic medical condition, difficulty significantly increased with cannabis use, more so for daily cannabis users. The greater difficulty with cannabis use was less pronounced for chronic medical conditions associated with higher cognitive difficulty, such as depression. For those without a chronic medical condition, cannabis use had a larger increasing effect on cognitive impairment.
References
- National Academies of Sciences, Engineering, and Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. The National Academies Press; 2017.
- Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109(40):E2657–E2664.
- Crean RD, Crane NA, Mason BJ. An evidence-based review of acute and long-term effects of cannabis use on executive cognitive functions. J Addict Med. 2011;5(1):1–8.
- Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–2227.
- Whitlow CT, Liguori A, Livengood LB, et al. Long-term heavy marijuana users make costly decisions on a gambling task. Drug Alcohol Depend. 2004;76(1):107–111.
- Hermann D, Lemenager T, Gelbke J, et al. Decision making of heavy cannabis users on the Iowa gambling task: stronger association with THC of hair analysis than with personality traits of the Tridimensional Personality Questionnaire. Eur Addict Res. 2009;15(2):
94–98. - Hitchcock LN, Tracy BL, Bryan AD, et al. Acute effects of cannabis concentrate on motor control and speed: smartphone-based mobile assessment. Front Psychiatry. 2021;11:623672.
- National Institute on Drug Abuse. Cannabis (marijuana). Sep 2024. Accessed 25 Mar 2024. https://nida.nih.gov/publications/drugfacts/cannabis-marijuana
- Datta S, Ramamurthy PC, Anand U, et al. Wonder or evil?: multifaceted health hazards and health benefits of Cannabis sativa and its phytochemicals. Saudi J Biol Sci. 2021;28(12):7290–7313.
- Silva L. Health benefits of cannabis, according to experts. Forbes Health. Updated 7 Sep 2023. Accessed 25 Mar 2024 https://www.forbes.com/health/cbd/health-benefits-of-cannabis/
- Henson JD, Vitetta L, Hall S. Tetrahydrocannabinol and cannabidiol medicines for chronic pain and mental health conditions. Inflammopharmacology. 2022;30(4):1167–1178.
- Carley DW, Prasad B, Reid KJ, et al. Pharmacotherapy of apnea by cannabimimetic enhancement, the PACE clinical trial: effects of dronabinol in obstructive sleep apnea. Sleep. 2018;41(1):zsx184.
- Farabi SS, Prasad B, Quinn L, Carley DW. Impact of dronabinol on quantitative electroencephalogram (qEEG) measures of sleep in obstructive sleep apnea syndrome. J Clin Sleep Med. 2014;10(1):49–56.
- Vallée A. Association between cannabis use and blood pressure levels according to comorbidities and socioeconomic status. Sci Rep. 2023;13(1):2069.
- Le Strat Y, Le Foll B. Obesity and cannabis use: results from 2 representative national surveys. Am J Epidemiol. 2011;174(8):929–933.
- Alshaarawy O, Anthony JC. Are cannabis users less likely to gain weight? Results from a national 3-year prospective study. Int J Epidemiol. 2019;48(5):1695–1700.
- Smit E, Crespo CJ. Dietary intake and nutritional status of US adult marijuana users: results from the Third National Health and Nutrition Examination Survey. Public Health Nutr. 2001;4:781–786.
- Clark TM, Jones JM, Hall AG, et al. Theoretical explanation for reduced body mass index and obesity rates in cannabis users. Cannabis Cannabinoid Res. 2018;3(1):259–271.
- Sansone RA, Sansone LA. Marijuana and body weight. Innov Clin Neurosci. 2014;11(7–8):
50–54. - Pew Research Center. Most Americans now live in a legal marijuana state – and most have at least one dispensary in their county. 29 Feb 2024. Accessed 25 Mar 2024. https://www.pewresearch.org/short-reads/2024/02/29/most-americans-now-live-in-a-legal-marijuana-state-and-most-have-at-least-one-dispensary-in-their-county/#:~:text=Since%20Colorado%20and%20Washington%20became,drug%20for%20medical%20use%20only
- Marinho V, Pinto GR, Bandeira J, et al. Impaired decision-making and time perception in individuals with stroke: Behavioral and neural correlates. Rev Neurol (Paris). 2019;175(6):367–376.
- Chen DT, Meschia JF, Brott TG, et al. Stroke genetic research and adults with impaired decision-making capacity: a survey of IRB and investigator practices. Stroke. 2008;39(10):2732–2735.
- Povroznik JM, Ozga JE, Vonder Haar C, Engler-Chiurazzi EB. Executive (dys)function after stroke: special considerations for behavioral pharmacology. Behav Pharmacol. 2018;29(7):638–653.
- Singh-Manoux A, Sabia S, Lajnef M, et al. History of coronary heart disease and cognitive performance in midlife: the Whitehall II study. Eur Heart J. 2008;29:2100–2107.
- Knopman DS. Cerebrovascular pathology in cognitive impairment: new (in)sights. Neurology. 2012;78(14):1032–1033.
- Roy E. Cognitive function In: Gellman MD, Turner JR (eds). Encyclopedia of Behavioral Medicine. Springer New York, 2013;448–449.
- Kang W, Whelan E, Malvaso A. Understanding cognitive deficits in people with arthritis. Healthcare (Basel). 2023;11(9):1337.
- Ab-Hamid N, Omar N, Ismail CAN, Long I. Diabetes and cognitive decline: challenges and future direction. World J Diabetes. 2023;14(6):795–807.
- Whittaker AL, George RP, O’Malley L. Prevalence of cognitive impairment following chemotherapy treatment for breast cancer: a systematic review and meta-analysis. Sci Rep. 2022;12(1):2135.
- Caldera-Alvarado G, Khan DA, Defina LF, et al. Relationship between asthma and cognition: the Cooper Center Longitudinal Study. Allergy. 2013;68(4):545–548.
- Peng YH, Wu BR, Su CH, et al. Adult asthma increases dementia risk: a nationwide cohort study. J Epidemiol Community Health. 2015;69(2):123–128.
- Chen MH, Li CT, Tsai CF, et al. Risk of dementia among patients with asthma: a nationwide longitudinal study. J Am Med Dir Assoc. 2014;15(10):763–767.
- Xie Z, Tong S, Chu X, et al. Chronic kidney disease and cognitive impairment: the kidney-brain axis. Kidney Dis (Basel). 2022;8(4):
275–285. - Klier C, Buratto LG. Stress and long-term memory retrieval: a systematic review. Trends Psychiatry Psychother. 2020;42(3):284–291.
- Zhang FF, Peng W, Sweeney JA, et al. Brain structure alterations in depression: psychoradiological evidence. CNS Neurosci Ther. 2018;24(11):994–1003.
- Keller AS, Leikauf JE, Holt-Gosselin B, et al. Paying attention to attention in depression. Transl Psychiatry. 2019;9(1):279. Erratum in: Transl Psychiatry. 2020;10(1):64.
- Leykin Y, Roberts CS, Derubeis RJ. Decision-making and depressive symptomatology. Cognit Ther Res. 2011;35(4):333–341.
- Mangoo S, Erridge S, Holvey C, et al. Assessment of clinical outcomes of medicinal cannabis therapy for depression: analysis from the UK Medical Cannabis Registry. Expert Rev Neurother. 2022;22(11–12):995–1008.
- US Department of Health and Human Services. Behavioral Risk Factor Surveillance System (BRFSS). Accessed 25 Mar 2024. https://health.gov/healthypeople/objectives-and-data/data-sources-and-methods/data-sources/behavioral-risk-factor-surveillance-system-brfss
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: 2022 summary data quality report. 8 Aug 2023. Accessed 25 Mar 2024. https://www.cdc.gov/brfss/annual_data/2022/pdf/2022-dqr-508.pdf
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Accessed 25 Mar 2024. https://www.cdc.gov/brfss/
- Azofeifa A, Mattson ME, Schauer G, et al. National estimates of marijuana use and related indicators: National Survey on Drug Use and Health, United States, 2002–2014. MMWR Surveill Summ. 2016;65(11):1–28.
- Han B, Compton WM, Blanco C, Jones CM. Trends in and correlates of medical marijuana use among adults in the United States. Drug Alcohol Depend. 2018;186:120–129.
- Dai H, Richter KP. A national survey of marijuana use among US adults with medical conditions, 2016–2017. JAMA Netw Open. 2019;2(9):e1911936.
- Trifu SC, Trifu AC, Aluaş E, et al. Brain changes in depression. Rom J Morphol Embryol. 2020;61(2):361–370.
- Moica T, Gligor A, Moica S. The relationship between cortisol and the hippocampal volume in depressed patients – a MRI pilot study. Procedia Technology. 2016;22:1106–1112.
- Henry A, Katsoulis M, Masi S, et al. The relationship between sleep duration, cognition and dementia: a Mendelian randomization study. Int J Epidemiol. 2019;48(3):849–860.
- Eizadi-Mood N, Akouchekian S, Yaraghi A, et al. Memory impairment following acute tricyclic antidepressants overdose. Depress Res Treat. 2015;2015:835786. doi: 10.1155/2015/835786. Epub 2015 Jan 14.
- Schwert C, Stohrer M, Aschenbrenner S, et al. Biased neurocognitive self-perception in depressive and in healthy persons. J Affect Disord. 2018;232:96–102.
- Premilovac D, Sutherland BA. Acute and long-term changes in blood flow after ischemic stroke: challenges and opportunities. Neural Regen Res. 2023;18(4):799-800. doi: 10.4103/1673-5374.350699.
- Wijnant SRA, Bos D, Brusselle G, et al. Comparison of cerebral blood flow in subjects with and without chronic obstructive pulmonary disease from the population-based Rotterdam Study. BMJ Open. 2021;11(12):e053671.
- Bian R, Zhang Y, Yang Y, et al. White matter integrity disruptions correlate with cognitive impairments in asthma. J Magn Reson Imaging. 2018.
- Xie H, Yung WH. Chronic intermittent hypoxia-induced deficits in synaptic plasticity and neurocognitive functions: a role for brain-derived neurotrophic factor. Acta Pharmacol Sin. (2012) 33:5–10.
- Ovsenik A, Podbregar M, Fabjan A. Cerebral blood flow impairment and cognitive decline in heart failure. Brain Behav. 2021;11(6):e02176.
- Mueller K, Thiel F, Beutner F, et al. Brain damage with heart failure: cardiac biomarker alterations and gray matter decline. Circ Res. 2020;126(6):750–764.
- Kruger J, Dunning D. Unskilled and unaware of it: How difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol.1999;77(6):1121–1134.
- Van der Elst W, Van Boxtel MP, Van Breukelen GJ, Jolles J. A large-scale cross-sectional and longitudinal study into the ecological validity of neuropsychological test measures in neurologically intact people. Arch Clin Neuropsychol. 2008;23(7–8):787–800.
- Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol. 2013;13:49.
- WebMD. How to avoid a high tolerance to cannabis. Reviewed 28 May 2023. Accessed 10 Oct 2024. https://www.webmd.com/mental-health/addiction/how-avoid-high-tolerance-cannabis.