by Shahid Ali, MD; Shagufta Jabeen, MD; Rebecca J. Pate, MD; Marwah Shahid, MS; Sandhya Chinala, MD; Milankumar Nathani, MD; and Rida Shah, MD
by Shahid Ali, MD; Shagufta Jabeen, MD; Rebecca J. Pate, MD; Marwah Shahid, MS; Sandhya Chinala, MD; Milankumar Nathani, MD; and Rida Shah, MD
Drs. Ali, Chinala, Nathani, and Shah are from Meharry Medical College, Nashville, Tennessee; Drs. Jabeen and Pate are from Veterans Affairs, Nashville, Tennessee; and Ms. Shahid is from Georgetown University, Washington, DC.
Innov Clin Neurosci. 2015;12(5–6):27–33.
Funding: No funding was provided for the preparation of this article.
Financial disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Conversion disorder, hysteria, unconscious conflict, repressed idea, psychoanalytic factors, psychogenic nonepileptic seizures, conversion anesthesia, therapeutic alliance, striatothalamocortical circuits
Abstract: In this article, the authors accentuate the signs and symptoms of conversion disorder and the significance of clinical judgment and expertise in order to reach the right diagnosis. The authors review the literature and provide information on the etiology, prevalence, diagnostic criteria, and the treatment methods currently employed in the management of conversion disorder. Of note, the advancements of neuropsychology and brain imaging have led to emergence of a relatively sophisticated picture of the neuroscientific psychopathology of complex mental illnesses, including conversion disorder. The available evidence suggests new methods with which to test hypotheses about the neural circuits underlying conversion symptoms. In context of this, the authors also explore the neurobiological understanding of conversion disorder.
Introduction
Conversion disorder, also called functional neurological symptom disorder,[1] is defined as a psychiatric illness in which symptoms and signs affecting voluntary motor or sensory function cannot be explained by a neurological or general medical condition.[2] Psychological factors, such as conflicts or stress, are judged to be associated with the deficits.[3] The term conversion disorder was coined by Sigmund Freud, who hypothesized that the occurrence of certain symptoms not explained by organic diseases reflect unconscious conflict.[3] The word conversion refers to the substitution of a somatic symptom for a repressed idea.[3,4]
Common examples of conversion symptoms include blindness, paralysis, dystonia, psychogenic nonepileptic seizures (PNES), anesthesia, swallowing difficulties, motor tics, difficulty walking, hallucinations, anesthesia, and dementia.[5] In patients with conversion disorder, these symptoms are not caused directly by a physiological effect; rather these symptoms are caused by a psychological conflict. Patients diagnosed with conversion disorder are not feigning the signs and symptoms. Despite the lack of a definitive organic diagnosis, the patient’s distress is very real and the physical symptoms the patient is experiencing cannot be controlled at will (i.e., the patient is not malingering an illness). As an example, according to the Medline Medical Dictionary,[6] “…a woman who believes it is not acceptable to have violent feelings may suddenly feel numbness in her arms after becoming so angry that she wanted to hit someone. Instead of allowing herself to have violent thoughts about hitting someone, she experiences the physical symptom of numbness in her arms.”
Patients who convert their emotional problems into physical symptoms spend nine times the cost for healthcare as people who do not, and 82 percent of adults with conversion disorder stop working because of their symptoms.[7] The annual bill for conversion disorder in the United States is $20 billion, not counting absenteeism from work and disability payments.[7] Despite its clinical importance, there has been only marginal progress in our understanding of conversion disorder relative to many other neurological and psychiatric disorders.[8]
In this article, we seek to emphasize the importance of obtaining detailed histories and performing physical examinations of patients who present with symptoms often seen in conversion disorder. We also discuss how to differentiate conversion disorder symptoms from other somatoform disorders. The article expands on psychiatric care, the role of neuroimaging studies in diagnosing conversion disorder, and the importance of therapeutic alliance in order to achieve the best outcome.
Hysteria to Conversion
The notion of hysteria can be traced to the ancient times. In the gynecological treatises of the Hippocratic corpus (5th and 4th centuries before the common era [BCE]), Hippocrates, considered the “father of medicine,” describes an illness in which the uterus dries up and wanders the body in search of moisture. They called this hysteria. Symptoms would then be caused by the uterus pressing on other organs. This theory is the source of the name, which stems from the Greek cognate of uterus, hystera.[9,10] In the 17th century, Rene Descartes postulated mind-body dualism, in which mind and body are two distinct substances that cannot exist in unity, as the body is subjected to mechanical laws and the mind is not.[11] This led to the development of a reductionist medical model with a dualistic outlook influencing management of symptoms.[12] Emerging theories in the 19th century acknowledged the involvement of the central nervous system (CNS) associated with hysterical symptoms. Freud’s psychodynamic theory contributed significantly to the study of hysteria because his account of symptom generation, in which unconscious conflict and effective motive are transformed into bodily complaints, paved the way for the idea of conversion symptoms.[13]
Etiology
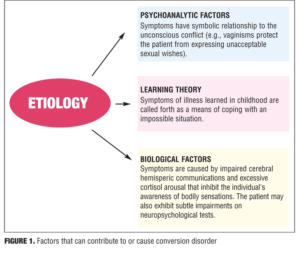
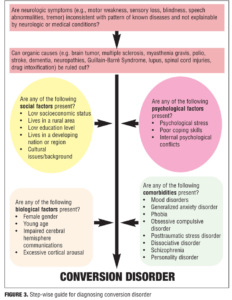
Conversion disorder is associated with conflicts or recent stressors, and its symptoms manifest as a result of unconscious conflict between a forbidden wish of the patient and his or her conscience. The conversion symptoms symbolically represent a partial wish fulfillment without the individual’s full awareness of the unacceptable desire[3] (e.g., vaginismus with sexual desire, syncope with arousal, paralysis with anger). Conversion disorder has been attributed to both nonbiological and biological factors (Figure 1).[3,14]
Signs and Symptoms
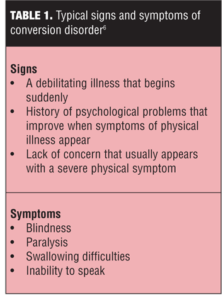
Conversion symptoms typically begin with some stressor, trauma, or psychological distress that manifests itself as a physical deficit. There is no underlying physical cause for the symptom(s), and the affected individual cannot control the symptom(s). Symptoms may vary in severity and may come and go or be persistently present. Table 1 lists typical signs and symptoms of conversion disorder.[6]
Epidemiology
The reported incidence of conversion symptoms varies widely depending on the population studied. Studies have estimated that 20 to 25 percent of patients in a general hospital setting have individual symptoms of conversion, and five percent of patients in this setting meet the criteria for the full disorder.[15,16] Medically unexplained neurological symptoms account for approximately 30 percent of referred neurology out-patients.[17] In a study of 100 randomly selected patients from a psychiatry clinic, 24 were noted to have unexplained neurological symptoms.[17]
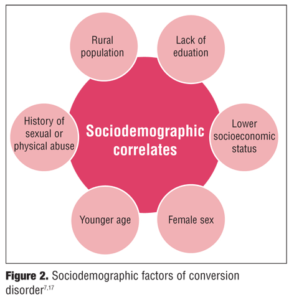
Among adults, women diagnosed with conversion disorder outnumber men by a 2:1 to 10:1 ratio; less educated people and those of lower socioeconomic status are more likely to develop conversion disorder; race by itself does not appear to be a factor.[7] There is a major difference between the populations of developing/third world countries compared to developed countries; in developing countries, the prevalence of conversion disorder may run as high as 31 percent.[7] Figure 2 illustrates the sociodemographic factors common in conversion disorder.
Diagnosis
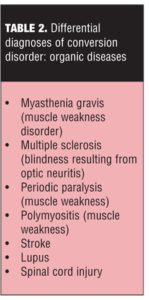
The diagnosis of conversion disorder continues to be a clinical challenge. A thorough psychiatric history and examination is necessary to explicate the onset of symptoms, the presence of stressors, and the presence of comorbid conditions.[5] According to a study, 47.7 percent of the subjects with conversion disorder experienced some type of dissociative disorder.[18] The diagnosis of conversion disorder should be made after establishing positive clinical findings that are incompatible with organic disease or are inconsistent across different parts of the examination19 and after ruling out any medical conditions the symptoms are mimicing (Table 2).[20]
Diagnostic criteria. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5),[21] conversion disorder is characterized by the following:
• One or more symptoms of altered voluntary motor or sensory function
• Clinical findings that show evidence of incompatibility between the symptoms and recognized neurological or medical conditions
• Symptoms or deficit that are not better explained by another medical or mental disorder
• Symptoms or deficit that cause clinically significant distress or impairment in social, occupational, or other important areas of functioning or warrants medical evaluation.
Figure 3 provides an illustrative, stepwise guide to assist clinicians in diagnosing conversion disorder.
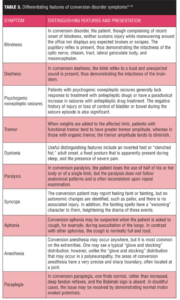
Differential diagnoses. Patients with conversion disorder may present with blindness, deafness, pseudo seizures, dystonia, paralysis, syncope, or other neurological symptoms. The presenting symptoms depend on the cultural milieu, the patient’s degree of medical knowledge (i.e., individuals with a high degree of medical knowledge tend to have more subtle symptoms and deficits that may closely simulate neurological or other general medical conditions, whereas those with less medical knowledge may have more implausible symptoms), and the underlying psychiatric issue(s).[5] Table 3[22–32] lists the differentiating features of conversion disorder symptoms from those of organic disease. The following paragraphs review several examples of psychiatric disorders that should be ruled out before a diagnosis of conversion disorder is made.
Hypochondriasis. Hypochondriasis is the excessive preoccupancy or worry about having one (or more) serious physical illnesses. This debilitating condition is the result of an inaccurate perception of the condition of body or mind despite the absence of an actual medical condition (e.g., “I know I’ve got cancer; they just haven’t done the right test yet”).[33]
Factitious disorder. Factitious disorder is a condition in which a person acts as if he or she has a physical or mental illness when he or she is not really sick. Factitious disorder by proxy is when a person acts as if a person in his or her care has an illness when the person does not. Factitious disorder is considered a mental illness because it is associated with severe emotional difficulties. People with factitious disorder deliberately create or exaggerate symptoms of an illness in several ways. They may lie about or fake symptoms, hurt themselves to bring on symptoms, or alter tests (such as contaminating a urine sample) to make it look like they or the person in their care is sick. Those with factitious disorder have an inner need to be seen as ill or injured without the need to achieve personal or financial gain.[34]
Somatisation. Somatisation is a condition in which a person experiences physical symptoms that are inconsistent with or cannot be fully explained by any underlying general medical or neurological condition. Preoccupation with these symptoms leads to excessive distress in the patient.[35]
Malingering. Malingering is not a mental disorder; however, psychiatrists and neurologists will likely encounter an individual malingering a psychiatric or neurological illness at some point in their careers. Malingering is defined as intentionally feigning the symptoms of a physical, psychiatric, or neurological disorder in order to achieve personal or financial gain. The individual is fully aware that he or she is feigning the symptoms and has clear knowledge of why he or she is doing it (e.g., for financial gain, recognition, or revenge).[10]
Neural Correlates of Conversion disorder
The growing trend to measure structural and functional changes in the brain through imaging has contributed significantly to improving understanding of the neural mechanisms of many psychiatric conditions, including conversion disorder.[13] Functional imaging findings suggest the involvement of prefrontal cortex as a candidate region in conversion disorder.[32,36–39]
Marshall et al[36] performed positron emission tomography (PET) on a woman with chronic left-sided paralysis (without sensory loss) in whom no organic lesion could be found. Regional cerebral blood flow was measured when she tried to move either her paralyzed leg or her other leg. The attempt to move the paralyzed leg failed to activate the right primary cortex. Instead there was activation of the right orbitofrontal and right anterior cingulate gyrus. The authors hypothesized that inhibitory pathways involving the orbitofrontal cortex and anterior cingulate may “disconnect” the premotor areas from the primary motor cortex, preventing the patient’s conscious intention from being translated into action. The authors suggested that the activation seen when this patient was preparing to move her affected limb provides evidence against feigning. The case report also suggests that inhibition of willed movement may play an important role in people with functional paralysis.[36]
Vuilleumier et al32 proposed another hypothesis in which it is argued that patients who exhibit symptoms of conversion disorder have a deficit in volition that involves the left dorsolateral prefrontal cortex (DLPFC) and striatothalamocortical circuits. This explanation implicates different structures and functions in seeking to explain the cause(s) of conversion disorder. It is possible, given the complexity of brain structure and function, that conversation disorder is associated with deficits in both planning and execution (premotor stage).
By beginning to understand the neural mechanisms of conversion disorder we may gain valuable insights into the cognitive processes involved in attention and volition and reduce some of the controversy and stigma associated with this common disorder.
Treatment
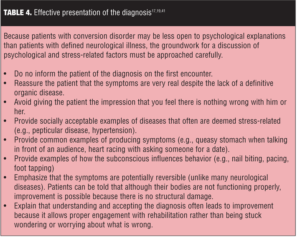
Presenting the diagnosis. Once conversion disorder is confirmed, the key to successful treatment is the establishment of a strong therapeutic alliance with the patient and the incorporation of a goal-oriented treatment program. Many patients who experience conversion disorder are unable to understand the inner conflict, which is perhaps occurring on an unconscious level.[5] Confronting patients about the “psychological nature” of their symptoms can and usually does make the symptoms worse.[3] However, patients can only achieve resolution of the conflict and the physical symptoms once they are able to recognize the connection.[5] Table 4 lists examples of how to present the diagnosis to patients.
Psychotherapy. The cornerstone of treatment for conversion disorder is psychotherapy aimed at elucidating the emotional bases of symptoms.[40] Psychotherapy can include individual or group therapy, behavioral therapy, hypnosis, biofeedback, and relaxation training. Cognitive behavioral therapy (CBT) has shown the highest efficacy in treatment of pseudoseizures.[22] Behavioral interventions should focus on improving self-esteem, increasing the capacity to express emotions, and improving the ability to communicate comfortably with others.[22]
Physical therapy. Research has shown that physical therapy can be an effective method of treatment.[41] Physiotherapy treatment is essential in the management of people with conversion disorder to allow them to overcome their physical symptoms and prevent secondary complications, such as muscle weakness and stiffness, that may occur as a result of inactivity.[41] Progressive exercises that start as simple tasks and move to more challenging ones has shown to be effective in those with neurological disorders as well as conversion disorder. The physical therapist seeks to build the patient’s motor skills by gradually providing less verbal and tactile cueing or other assistance while the patient performs certain tasks.[41]
Medication. Conversion disorder can also be improved through the use of medications to treat underlying psychiatric issues, such as depression and anxiety. Medications may include antidepressants, anxiolytics, or others depending on the psychiatric co-morbidity.[40] Regular follow-up appointments with a neurologist and/or psychiatrist should be provided to the patient to limit emergency room visits and unnecessary diagnostic or invasive tests.[40]
Prognosis. A good prognosis can be expected in patients where conversion disorder had a sudden onset, a short duration, an early identifiable stressor, no ongoing litigation, good premorbid functioning, and lack of comorbid psychiatric disorders.[3]
Conclusion
Conversion disorder is a condition where mental or emotional crises produce stress that converts to a physical problem. People diagnosed with conversion disorder are not feigning the symptoms; the symptoms are real. Therefore, it is important not to label patients with conversion disorder as manipulative. The signs and symptoms of conversion disorder can be difficult to tease out of a multitude of other possible diagnoses, and a thorough understanding of each patient’s pathology should be the first step in establishing the correct diagnosis and effective treatment. It is very important to efficiently and effectively obtain medical and psychiatric history from the patient while being careful about how and when to ask about psychological symptoms. Creating a therapeutic alliance with the patient is essential to a successful outcome.[5] A thorough psychiatric examination is necessary to explicate the onset of symptoms and presence of stressors and comorbid conditions. This would help establish an integrated overall understanding of how abnormal psychological states can convert to a neurological deficit in the absence of somatic pathology. Focusing research on neural correlates of conversion disorder has immense potential for therapy and prevention. In terms of treatment, there is no single method that can be globally recommended. Regular follow-up visits combined with cognitive-behavioral therapy and physiotherapy (for motor symptoms) have shown promising results. Pharmacotherapy may be necessary for any underlying psychiatric disorders.
References
1. American Psychiatric Association. DSM 5 development. Highlights of changes from DSM-IV-TR to DSM 5 http://www.dsm5.org/Documents/changes%20from%20dsm-iv-tr%20to%20dsm-5.pdf. Access date: May 30, 2015.
2. Ballmaier M, Schmidt R. Conversion disorder revisited. May 23, 2005. http://www.functionalneurology.com/materiale_cic/99_XX_3/892_conversion/index.html. Access date: May 30, 2015.
3. Blitzstein S. Recognizing and conversion disorder. Virtual Mentor. 2008;10(3):158–160.
4. Freud S. The neuro-psychoses of defense. In: Freud S, Strachey J, Freud A, Institute of Psycho-analysis (eds). The Standard Edition of the Complete Psychological Works of Sigmund Freud. London: Hogarth Press and the Institute of Psycho-Analysis;1962:45–61.
5. Marshall S, Bienenfeld D. Conversion disorder. Medscape. Drugs and diseases. June 26, 2013. http://emedicine.medscape.com/article/287464-overview. Access date: May 30, 2015.
6. Conversion disorder. www.nlm.nih.gov. URL: http://www.nlm.nih.gov/medlineplus/ency/article/000954.htm. Access date: May 30, 2015.
7. Encyclopedia of mental disorders. Conversion disorder. http://www.minddisorders.com/Br-Del/Conversion-disorder.html#ixzz35zYRNxAA. Access date: May 30, 2015.
8. Nicholson T, Stone J, Kanaan R. Conversion disorder: a problematic diagnosis. J Neurol Neurosurg Psychiatry. 2011; 82(11):1267–1273.
9. The Marshall Protocol Knowledge Base. Psychosomatic explanations for disease. January 2, 2012. http://mpkb.org/home/alternate/psychosomatic. Access date May 28, 2015.
10. Owens C, Dein S. Conversion disorder: the modern hysteria. Adv Psychiatr Treat. 2006;12(2):152–157.
11. Tweyman S (ed). Rene Descartes’ Meditations on First Philosophy in Focus. New York, NY: Routledge; 1993.
12. Soares N, Pataki C. Pediatric conversion disorder. Medscape. Drugs and diseases. March 20, 2014. http://emedicine.medscape.com/article/917864-overview. Accessed on May 30, 2015.
13. Scott R, Anson J. Neural correlates of motor conversion disorder. Motor Control. 2009;13:161–184.
14. Sadock BJ, Kaplan VA. Kaplan and Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 10th Edition. Philadelphia: Lippincott Williams & Wilkins; 2007.
15. Engl GL. Conversion symptoms. In: McBride CM (ed). Signs and Symptoms: Applied Pathologic Physiology and Clinical Interpretation, Fifth Edition. Philadelphia: JB Lippincott; 1970:650–668.
16. Feinstein A. Conversion disorder: advances in our understanding CMAJ. 2011;183(8):915–920.
17. Carson A, Best S, Postma K, et al. The outcome of neurology outpatients with medically unexplained symptoms: a prospective cohort study. J Neural Neurosurg Psychiatry. 2003;74(7): 897–900.
18. Sar V, Akyüz G, Kundakçi T et al. Childhood trauma, dissociation, and psychiatric comorbidity in patients with conversion disorder. Am J Psychiatry. 2004;161(12):2271–2276.
19. Stone J, Sharpe M, Dimsdale J. Conversion disorder in adults: treatment. Wolters Kluwers. Up to date. June 10, 2014. http://www.uptodate.com/contents/conversion-disorder-in-adults-treatment. Access date May 30, 2015.
20. Mayo Clinic. Diseases and conditions. Conversion disorder. www.mayoclinic.org. http://www.mayoclinic.org/diseases-conditions/conversion-disorder/basics/definition/CON-20029533. Accessed on June 2, 2015.
21. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington, VA: American Psychiatric Press, Inc.; 2013.
22. Ali S, Jabeen S, Arain A, et al. How to use your clinical judgment to screen for and diagnose psychogenic nonepileptic seizures without video electroencephalogram. Innov Clin Neurosci. 2011; 8(1): 36–42.
23. Haque R, Alavi Z. Mr. Smith is falling every day: conversion disorder in an elderly man. Ann Longterm Care. 2012; 20(11).
24. Baker A, Silver J. Hysterical paraplegia. J Neurol Neurosurg Psychiatry. 1987;50:375–382.
25. Couprie W, Wijdicks E, Rooijmans H, et al. Outcome on conversion disorder: a follow up study. J Neurol Neurosurg Psychiatry. 1995;58:750–752.
26. Keane J. Wrong-way deviation of the tongue with hysterical hemiparesis. Neurology. 1986;36:1406–1407.
27. Keane J. Hysterical gait disorders: 60 cases. Neurology. 1989;39:586–589.
28. Lang A, Koller W, Fahn S. Psychogenic parkinsonism. Arch Neurol. 1995;52:802–810.
29. Moene F, Spinhoven P, Hoogduin K, et al. A randomized controlled clinical trial on the additional effect of hypnosis in a comprehensive treatment programme for in-patients with conversion disorder of the motor type. Psychother Psychosom. 2002;71:66–76.
30. Roelofs K, Hoogduin K, Keijsers G, et al. Hypnotic susceptibility in patients with conversion disorder. J Abnorm Psychol. 2002;111:390–395.
31. Speed J. Behavioral management of conversion disorder: retrospective study. Arch Phy Med Rehabil. 1996; 77: 147–154.
32. Vuilleumier P, Chicherio C, Assal F, et al. Functional neuroanatomical correlates of hysterical sensorimotor loss. Brain. 2001;124(Pt 6):1077–1090.
33. Avia M, Ruiz M. Recommendations for the treatment of hypochondriac patients. J Contemp Psychother. 2005;35(3):301–313.
34. WebMD. Mental health center. Factitious disorders. http://www.webmd.com/mental-health/factitious-disorders Access date May 30, 2015.
35. Spratt E, Pataki C. Somatoform disorders. Medscape. Drugs and diseases. March 4, 2014. http://emedicine.medscape.com/article/918628-overview Access date June 1, 2015.
36. Marshall J, Halligan P, Fink G, et al. The functional anatomy of hysterical paralysis. Cognition. 1997; 64(1):B1–B8
37. Spence S, Crimlisk H, Cope H, et al. Discrete neurophysiological correlates in prefrontal cortex during hysterical and feigned disorder of movement. Lancet. 2000;355:1243–1244.
38. Tiihonen J, Kuikka J, Viinamaki H, et al. Altered cerebral blood flow during hysterical paresthesia. Biol Psychiatry. 1995;37:134-137.
39. Harvey S, Stanton B, David A. Conversion disorder: towards a neurobiological understanding; Neuropsychiatr Dis Treat. 2006;2(1):13–20.
40. Stonnington C, Barry J, Fisher R. Conversion disorder. Am J Psychiatry. 2006;163:1510–1517.
41. Kaur J, Garnawat D, Ghimiray D, et al. Conversion disorder and physical therapy; Delhi Psychiatry J. 2012;15(2):394–397.