 by Randy A. Sansone, MD, and Lori A. Sansone, MD
by Randy A. Sansone, MD, and Lori A. Sansone, MD
R. Sansone is a professor in the Departments of Psychiatry and Internal Medicine at Wright State University School of Medicine in Dayton, OH, and Director of Psychiatry Education at Kettering Medical Center in Kettering, OH. L. Sansone is a civilian family medicine physician at the Primary Care Clinic at Wright-Patterson Air Force Base in Dayton, OH. The views and opinions expressed in this article are those of the authors and do not reflect the official policy or position of the United States Air Force, Department of Defense, or United States Government.
Innov Clin Neurosci. 2015;12(5–6):34–37.
Funding: There was no funding provided for the preparation of this article.
Financial disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Abuse, childhood abuse, emotional abuse, gastrointestinal, irritable bowel syndrome, physical abuse, sexual abuse
Abstract: Irritable bowel syndrome is allegedly the most common gastrointestinal diagnosis in the United States. The etiology of this syndrome appears to entail the interaction of both genes and the environment. One potential environmental contributory factor to irritable bowel syndrome is abuse in childhood. Of the various forms of abuses previously examined, sexual abuse in childhood appears to be the most patent contributor. However, both emotional and physical abuses may also contribute to irritable bowel syndrome, although less distinctly. Studies examining a combined childhood-abuse variable (i.e., sexual, emotional, and/or physical abuses) in relationship to irritable bowel syndrome also indicate inconsistent results. Given the presence of childhood abuse as a potential factor in the development of irritable bowel syndrome, a number of pathophysiological events are postulated to explain this relationship, including alterations in norepinephrine and serotonin levels as well as dysregulation of the hypothalamic-pituitary-adrenal axis. Only future research will clarify the specific abuse elements (i.e., further clarification of the individual types of abuse, duration of abuse, roles of the perpetrator/victim) and the pathophysiological changes that culminate in irritable bowel syndrome.
This ongoing column is dedicated to the challenging clinical interface between psychiatry and
primary care—two fields that are inexorably linked.
Introduction
According to Wald, irritable bowel syndrome (IBS) is the most commonly diagnosed gastrointestinal condition in the United States.[1] IBS is a syndrome characterized by chronic abdominal bloating, cramping, and pain as well as altered bowel habits (e.g., diarrhea/constipation)—all in the absence of any organic cause. Rey and Talley indicate that the world-wide prevalence of IBS varies due to the criteria used for diagnosis, and ranges from 2.1 to 22 percent.[2] According to these authors, women are more frequently diagnosed with IBS than men, and contributory factors may include both genetic components and environmental components such as childhood abuse. In this edition of The Interface, we probe into the empirical relationships between abuse in childhood and IBS.
Studies of Abuse in Childhood among IBS Patients
A number of investigators have studied relationships between various types of abuse in childhood and IBS. As a preamble, in a review of the PubMed literature from 1966 through 2007, Chitkara et al[3] concluded that abuse in childhood was patently associated with the development of IBS in adulthood. We now review studies that have examined relationships between various types of abuse in childhood and IBS, including methodological formats and corresponding findings.
Sexual abuse in childhood and IBS. Without doubt, sexual abuse is the most studied form of childhood abuse in relationship to IBS. We will present these studies in chronological order.
In a 1993 study, Walker et al[4] administered structured psychiatric interviews to 28 patients with IBS and 19 patients with inflammatory bowel disease, and compared childhood-abuse histories. In this study, patients with IBS reported significantly higher rates of severe childhood sexual abuse compared to participants with inflammatory bowel disease (11% vs. 0%).
In a 1995 study that compared 71 patients with IBS to 40 patients with inflammatory bowel disease, Walker et al[5] examined the prevalence of sexual abuse in childhood using structured interviews. In this study, molestation and rape in childhood were significantly higher among participants with IBS.
In a 2001 study, Heitkemperet al[6] examined histories of childhood sexual abuse among 167 IBS sufferers and controls, using a combination of self-report measures and interviews. In comparison with controls (women without IBS), women participants with IBS had statistically significantly higher rates of unwanted sexual contact during childhood, such as touching of one’s sexual organs.
In a 2002 study, Blanchard et al [7] examined 71 men and women with IBS who were seeking psychological treatment. In this sample, 57.7 percent of participants reported either sexual or physical abuse in childhood.
In a 2003 study, Salmon et al[8] compared 64 patients with IBS to 61 patients with bowel symptoms explained by physical disease. Using self-report questionnaires, the researchers found that sexual abuse in childhood was statistically significantly more common among IBS participants compared with physical-disease participants.
In a 2005 study by Ross,[9] which utilized both self-report surveys and interviews, participants were categorized into three groups: 1) those with IBS, 2) those with inflammatory bowel disease, and 3) those with other gastrointestinal disorders. The rates for childhood sexual abuse among IBS, inflammatory bowel, and other-syndrome participants were 37.9 percent, 9.1 percent, and 11.6 percent, respectively—a notable difference.
In a 2010 study using self-report questionnaires, Beesley et al[10] compared 75 patients with IBS to 76 patients with Crohn’s disease regarding their histories of childhood sexual abuse. After controlling for gender, sexual abuse in childhood was reported significantly more often by patients with IBS compared with those with Crohn’s disease.
In a final study from 2012, Bradford et al[11] examined 294 patients with IBS and 435 controls using self-report measures. In comparing these two cohorts with regard to childhood “sexual events,” rates were significantly higher in the IBS subsample (31.2% vs. 17.9%).
Emotional abuse in childhood and IBS. In addition to studies examining sexual abuse in childhood, three studies have examined emotional abuse in childhood in relationship to IBS. In support of a relationship, in a 2010 study, Tietjen et al[12] examined 418 IBS patients who were culled from a large group of patients with migraine headaches. In this atypical study sample, using self-report measures, investigators found that emotional abuse was associated with IBS. In a 2012 study, Bradford et al[11] compared 294 patients with IBS to 435 controls, using self-report measures. Compared to controls, the cohort with IBS reported a statistically significantly higher prevalence of emotional abuse (54.9% vs. 27.0%).
In contrast to the preceding findings, in a study from 2003, Salmon et al[8] found no between-group differences in emotional abuse when comparing IBS patients to patients with physical evidence of gastrointestinal disease. While the findings from these three studies clearly differ, this may be due to an erratic relationship between childhood emotional abuse and IBS and/or the study methodology (i.e., how the queries were actually posed to participants, variations in the duration of the abuse, relationship variability between the perpetrator and victim, presence or not of other forms of childhood maltreatment).
Physical abuse in childhood and IBS. Again, in contrast to the relatively consistent findings encountered with sexual abuse, the relationship between physical abuse in childhood and IBS is less patent. As for a positive association, Salmon et al[8] confirmed a relationship between physical abuse in childhood and IBS. In addition, Blanchard et al[7 ]reported high rates of physical abuse in childhood, but this was in conjunction with sexual abuse, and sexual abuse may have been the predominant influence.
In contrast to these positive associations, in a 1994 study by Tally et al,[13] there was no statistically significant difference in rates of physical abuse between patients with IBS and controls. In a study by Walker et al,[5] there was no difference in the prevalence of reported histories of physical abuse between participants with IBS and participants with inflammatory bowel disease. Heitkemper et al[6] found no differences between women with IBS and controls with regard to the prevalence of physical abuse in childhood. Finally, Ross9 found no difference in the prevalence of childhood physical abuse among participants with IBS, inflammatory bowel disease, or other gastrointestinal disorders.
Studies reporting relationships between combined abuse variables and IBS. Among IBS samples, three studies have combined individual childhood trauma variables into a single global trauma variable. As for positive findings, in a 1994 study using a mailed-survey methodology, Talley et al[13] examined 919 residents in Olmsted county, Minnesota. Symptoms of IBS were reported by 14 percent of the study sample. Researchers found a significant association between combined forms of abuse in childhood and IBS.
As for negative findings, in a 1995 survey study of 997 consecutive outpatients, Talley et al[14] identified 277 participants with IBS and compared these with the remainder of the sample. With regard to abuse in childhood (i.e., a combination of sexual, emotional, and physical abuses), there were no statistically significant differences between those with versus those without IBS. Similarly, Talley, Boyce, and Jones[15] reported analogous findings when using a combined trauma-variable approach among a random community sample of 730 Australians. The obvious difficulty with the combined-variable approach is that, according to the preceding studies, while sexual abuse evidences strong associations with IBS, emotional and physical abuses demonstrate more erratic relationships, with physical abuse being the least associated. Therefore, by combining trauma variables, significant findings risk being washed out.
Summary. According to the available studies, there appears to be a distinct relationship between a history of childhood sexual abuse and IBS. However, relationships between histories of emotional or physical abuses and IBS are inconsistent, with physical abuse in childhood demonstrating the most fragmentary association. Given these observations, studies that combine individual trauma variables into a single abuse variable may unintentionally obscure potentially significant findings.
Pathophysiological Explanations
The majority of findings to date indicate a relationship between sexual abuse in childhood and IBS, and perhaps relationships with both emotional abuse and physical abuse in childhood. What might explain these associations from a pathophysiological perspective?
Several authorities have suggested partial explanations. For example, O’Malley et al[16] posit that dysfunction in the brain-gut axis is fundamental to the development of IBS, and is attributable to the development of a maladaptive stress response that occurs through the activation of the immune system due to inflammation. Kendall-Tackett[17] maintains that trauma may alter brain function and culminate in a state of chronic hyperarousal. In keeping with these associations, Mulvihill[18] suggests that posttraumatic stress disorder may be a mediator between abuse in childhood and IBS in adulthood.
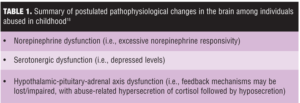
As for postulated abnormalities, Keeshin et al[19] contend that a number of changes in brain systems occur in individuals exposed to abuse, including relatively higher levels of norepinephrine, relatively lower levels of serotonin, and dysregulation of the hypothalamic-pituitary-adrenal (HPA) system. These investigators also indicate that hypothalamically secreted corticotropin-releasing hormone is associated with colonic dysmotility. In addition, studies of participants who were abused in childhood indicate abnormalities in cortisol regulation. Both of these latter findings reinforce the premise of HPA dysregulation among individuals who have been abused. These pathophysiological aberrancies may subsequently influence pain recognition, resulting in alterations in the processing of pain in abused individuals, with either hypersensitivity or hyposensitivity to pain.
Table 1 summarizes the pathophysiological explanations for the relationship between childhood abuse, in particular se and IBS.
Conclusion
IBS is purportedly the most common gastrointestinal dysfunction in the United States. While a number of genetic and environmental factors may contribute to IBS, current data indicate that abuse in childhood, particularly sexual abuse, is one relevant environmental factor. As for pathophysiological relationships between childhood abuse and IBS, there appears to be subsequent alterations in norepinephrine and serotonin levels as well as dysregulation of the HPA system. These changes may subsequently affect gut motility as well as distort pain recognition. Further avenues for research might include examining relationships between witnessing violence and IBS, assessing treatment responses to IBS among those with versus without childhood trauma, and additionally teasing out the pathophysiological mechanisms that mediate this complex relationship. Clearly, the relationship between childhood abuse and IBS is pertinent clinical territory for both psychiatrists and primary care clinicians.
References
1. Wald A. Clinical manifestations and diagnosis of irritable bowel syndrome. http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-irritable-bowel-syndrome?source=search_result&search=irritable+bowel+syndrome&selectedTitle=2%7E150. Accessed on May 2, 2012.
2. Rey E, Talley NJ. Irritable bowel syndrome: novel views on the epidemiology and potential risk factors. Dig Liver Dis. 2009;41:772–780
3. Chitkara DK, van Tilburg MA, Blois-Martin N, Whitehead WE. Early life risk factors that contribute to irritable bowel syndrome in adults: a systematic review. Am J Gastroenterol. 2008;103:765–774.
4. Walker EA, Katon WJ, Roy-Byrne PP, et al. Histories of sexual victimization in patients with irritable bowel syndrome or inflammatory bowel disease. Am J Psychiatry. 1993;150:1502–1506.
5. Walker EA, Gelfand AN, Gelfand MD, Katon WJ. Psychiatric diagnoses, sexual and physical victimization, and disability in patients with irritable bowel syndrome or inflammatory bowel disease. Psychol Med. 1995;25:1259–1267.
6. Heitkemper M, Jarrett M, Taylor P, et al. Effect of sexual and physical abuse on symptom experiences in women with irritable bowel syndrome. Nurs Res. 2001;50:15–23.
7. Blanchard EB, Keefer L, Payne A, et al. Early abuse, psychiatric diagnoses and irritable bowel syndrome. Behav Res Ther. 2002;40:289–298.
8. Salmon P, Skaife K, Rhodes J. Abuse, dissociation, and somatization in irritable bowel syndrome: towards an explanatory model. J Behav Med. 2003;26:1–18.
9. Ross CA. Childhood sexual abuse and psychosomatic symptoms in irritable bowel syndrome. J Child Sex Abuse. 2005;14:27–38.
10. Beesley H, Rhodes J, Salmon P. Anger and childhood sexual abuse are independently associated with irritable bowel syndrome. Br J Health Psychol. 2010;15:389–399.
11. Bradford K, Shih W, Videlock EJ, et al. Association between early adverse life events and irritable bowel syndrome. Clin Gastroenterol Hepatol. 2012;10:385–390.
12. Tietjen GE, Brandes JL, Peterlin B, et al. Childhood maltreatment and migraine (Part III). Association with comorbid pain conditions. Headache. 2010;50:42–51.
13. Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Gastrointestinal tract symptoms and self-reported abuse: a population-based study. Gastroenterology. 1994;107:1040–1049.
14. Talley NJ, Fett SL, Zinsmeister AR. Self-reported abuse and gastrointestinal disease in outpatients: association with irritable bowel-type symptoms. Am J Gastroenterol. 1995;90:366–371.
15. Talley NJ, Boyce PM, Jones M. Is the association between irritable bowel syndrome and abuse explained by neuroticism? A population based study. Gut. 1998;42:47–53.
16. O’Malley D, Quigley EM, Dinan TG, Cryan JF. Do interactions between stress and immune responses lead to symptom exacerbations in irritable bowel syndrome? Brain Behav Immun. 2011;25:1333–1341.
17. Kendall-Tackett KA. Physiological correlates of childhood abuse: chronic hyperarousal in PTSD, depression, and irritable bowel syndrome. Child Abuse Negl. 2000;24:799–810.
18. Mulvihill D. The health impact of childhood trauma: an interdisciplinary review, 1997–2003. Issues Compr Pediatr Nurs. 2005;28:115–136.
19. Keeshin BR, Cronholm PF, Strawn JR. Physiologic changes associated with violence and abuse exposure: an examination of related medical conditions. Trauma Violence Abuse. 2012;13:41–56.