 by J. Gibson Pennington, MD, and Jeffrey Guina, MD
by J. Gibson Pennington, MD, and Jeffrey Guina, MD
From Wright-Patterson Air Force Base and Wright State University Boonshoft School of Medicine Department of Psychiatry, Dayton, Ohio
Innov Clin Neurosci. 2016;13(9–10):44–48.
Funding: No funding was provided for the preparation of this article.
Financial Disclosures: The authors have no financial dislosures relevant to the content of this article.
Key Words: Eszopiclone, sedative, hypnotic, parasomnia, drug reaction, benzodiazepine-like, insomnia
Abstract
Eszopiclone is a benzodiazepine-like hypnotic that is commonly prescribed to treat insomnia. However, eszopiclone’s efficacy has been questionable in several clinical trials, and its pharmacologic profile makes its effects on sleep and behavior difficult to predict. We report a case demonstrating an instance of eszopiclone-induced parasomnia involving paranoia and a suicide attempt in a patient taking eszopiclone. We explore possible biochemical explanations examining the pharmacologic profile of eszopiclone and its potential for drug-drug interactions, especially with concomitant administration of monoaminergic medications such as antidepressants. Caution should be exercised when prescribing these medications, and evidence-based treatments for insomnia (e.g., cognitive behavioral therapy, biofeedback, sedating antidepressants) should be considered prior to sedative-hypnotic administration.
Introduction
Benzodiazepines and benzodiazepine-like hypnotics have been known to cause severe thought disturbances and behavioral changes. These effects range from mild[1–3] to life-threatening.[4] These potential adverse effects must be considered and discussed as part of informed consent, considering that hypnotics are routinely prescribed by healthcare providers.[5] In fact, as of 2010, zolpidem and eszopiclone were the two most commonly prescribed medications for treating insomnia.[6] Eszopiclone received United States Food and Drug Administration (FDA) approval for the treatment of insomnia in March 2004. However, the New England Journal of Medicine highlighted the fact that in the largest of the FDA’s three trials, patients receiving eszopiclone still met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for insomnia at the end of the trial.[7] The FDA equivalent in Europe, the European Medicines Agency (EMA), which is notoriously more stringent than the FDA, refused to grant approval for eszopiclone, citing that the drug was essentially pharmacologically and therapeutically similar to its original isometric form, zopiclone.[8] This is a common occurrence in Europe, as the EMA demands that newer versions of previous medications, especially anisomers, must demonstrate significantly improved benefit to patients in order to be marketed. Zopiclone was supposed to represent the next step in the evolution and pharmacologic advancement in the treatment of insomnia; however, it showed no significant difference from benzodiazepines in this area, and some literature suggests it is even less effective.[9] Despite evidence that eszopiclone is no better than its predecessor, it is still prescribed by many providers, and it could have a higher potential for adverse effects than other benzodiazepine-like hypnotics.[6,7] This risk could increase when it is prescribed concomitantly with monoaminergic drugs, such as selective serotonin reuptake inhibitors (SSRIs).[10] We report a case of a life-threatening adverse event in which these factors may have come into play.
While there are several case reports involving zolpidem and parasomnias, an extensive literature search did not find any similar cases involving eszopiclone. We searched PubMed for the years 1950 through June 2015. Search terms included the following: case report, parasomnia, sleep-related amnestic behaviors, sedative, hypnotic, benzodiazepine, paradoxical reaction, and somnambulism. Relevant articles were retrieved, and further sources were found by reviewing related links provided in the database and by reviewing the references of the discovered articles. The results of our literature review were used to provide potential explanations for this case report.
Case Report
A 48-year-old man presented to the trauma center after slicing his own neck with a box cutter. The patient was a former business administrator who recently had been laid off from his place of employment due to corporate cut-backs. The patient had a remote history of some depressive symptoms for approximately two years after the death of his father in 1997; however, these resolved without any treatment. Otherwise, the patient denied any prior mental health history. He specifically denied any history of suicidal ideation, suicide attempts, psychosis, or substance use disorders. The patient did develop a profound depression after being laid off from his job approximately four weeks prior to presentation, but denied any suicidal or morbid ideations. After “dealing” with the symptoms on his own, the patient then presented to his primary care physician two days prior to admission. He was prescribed sertraline 50mg and eszopiclone 2mg, both at bedtime.
The patient’s girlfriend confirmed that the patient took the sertraline and eszopiclone as prescribed for two nights. On the first night, there were no problems. During second night, the patient went to bed around 10:00 PM and, approximately 2.5 hours later, he abruptly awoke from sleep. According to the girlfriend, the patient was fidgeting, agitated, and paranoid. He kept repeating “They’re after me! They are coming for me, and they are going to capture me and torture me!” The girlfriend attempted to calm the patient; however, he was inconsolable. His agitation escalated until he began to sob uncontrollably. He then jumped up and ran out of the bedroom. The girlfriend followed him as he ran down the steps and into the garage, where he began rifling through boxes, his agitation continuing to escalate. The girlfriend pleaded for him to calm down, but her attempts were unsuccessful. The patient then recovered a box-cutter from a box and, looking at his girlfriend, stated, “They’re never going to catch me alive. I won’t let that happen.” He then took the box-cutter and sliced his own neck, collapsing on the garage floor in a pool of blood.
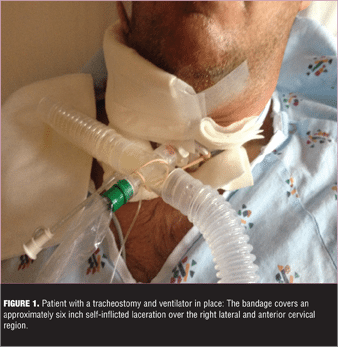
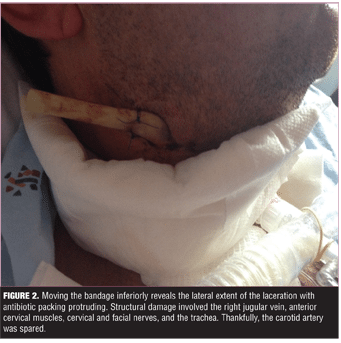
The girlfriend called emergency services immediately and the patient was aeromedically transported to the nearest Level 1 trauma center. On arrival, an emergency tracheotomy (Figures 1 and 2) was performed and the patient received a blood transfusion. The patient was admitted to the intensive care unit before stabilizing two days later. The patient had no recollection of the events that led to his hospitalization.
The patient remained in hospital for two weeks under care of the internal medicine service as well as the ear, nose, and throat surgery service. After extensive evaluation by the psychiatry consultation service, it was determined that the events that led to the patient’s presenting condition where likely the result of an adverse effect of his medications, and did not represent a suicide attempt related to his ongoing depression. The patient was never admitted to an inpatient psychiatric unit, and he remained on the general medical floor until he was discharged home after a total of 15 days in the hospital.
Discussion
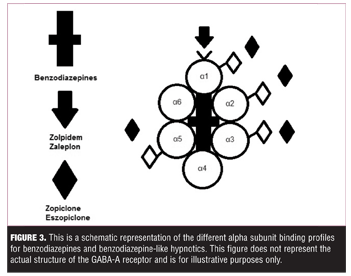
Eszopiclone is a potentiator of three major alpha subunits of gama-aminobutyric acid (anion) receptors (GABAA), the neuropsychiatric roles of which have been generally defined in various studies over the years. Potentiation at alpha-1 is believed to primarily mediate sedation, but is also involved in fear-reduction and anxiolysis; alpha-2 is the main subunit involved in anxiolysis; and alpha-3 is predominantly involved in fear-reduction.[11,12] One major pharmacologic difference between eszopiclone and other popular “Z-drugs,” such as zaleplon and zolpidem, is that eszopiclone is not selective for the alpha-1-GABAA subtype (Figure 3), and thus produces broader effects that are more similar to those produced by benzodiazepines.[8,12]
Benzodiazepines are notorious for adverse side-effects, such as parasomnias and amnesia.[13,14] Benzodiazepines have also been known to cause “paradoxical reactions” (e.g., behavioral disinhibition, impulsivity, agitation) in which patients may engage in uncharacteristic behaviors, such as suicidality, assaults, theft, or sexual indiscretions, without any history of similar behaviors before use or after discontinuation.[15] Benzodiazepines and alcohol are believed to exert depressogenic effects by two mechanisms: 1) by decreasing serum serotonin levels and inhibiting serotonergic function both acutely and chronically 16 and 2) via dopamine depletion (acute) or a “recalibration” (chronic) of baseline dopamine levels in the nucleus accumbens, which is known as the “pleasure center” of the brain.[17] Benzodiazepine-like medications exerting a similar depressogenic effect may explain the acute suicidality in our patient.
While there is a large contention that alpha-1-GABAA is the main player involved in parasomnias and sleep-related amnestic events, more recent research suggests that agonism at all three of these alpha-1-GABAA subtypes (specifically in the frontal and hippocampal lobes) contributes to these adverse reactions.[18] Given eszopiclone’s non-specific affinity for alpha-1-GABAA receptor subtypes, one can hypothesize that a person taking this medication, as opposed to other benzodiazepine-like hypnotics, would be exposed to increased risk for the benzodiazepine-associated side-effects mentioned above.
It is well known that people who suffer from depression commonly have insomnia. In fact, insomnia is significantly correlated with anxiety and depression.[19] Anxiety and depression are commonly treated with monoaminergic medications like SSRIs. Many SSRIs are known inhibitors of the CYP450-mediated drug metabolism. Specifically, sertraline is a clinically significant inhibitor of CYP3A4.[20]
Coincidentally, eszopiclone is metabolized mainly by the CYP3A4 and CYP2E1.[21] Given this fact, concomitant administration of eszopiclone with sertraline could potentially lead to an increased serum level of eszopiclone, increasing the likelihood for adverse effects. Previous research has found statistically significant evidence that sleep-related amnestic behaviors were a real phenomenon in patients taking zolpidem and were more likely to occur in those patients who were also taking monoaminergic medications such as SSRIs.[10] A review of case reports involving benzodiazepine-like hypnotics suggests that drug-drug interactions can play a significant role in hypnotic-induced complex behaviors.[12] Additionally, there is evidence that serotonergic pathways and serotonergic medications themselves may be implicated in parasomnias.[14] The exact role that sertraline played in our case is unknown, but evidence suggests that sertraline may increase the risk of eszopiclone-induced adverse effects, both directly through serotonergic pathways and indirectly by CYP3A4 inhibition.
Only one case report has been published involving eszopiclone and potential psychiatric side effects, and it describes an episode of eszopiclone-induced severe formication.[22] In contrast, there are numerous case reports involving zolpidem-induced adverse events, including suicide attempts.[4,23,24] The disparity in reporting could be due to the fact that eszopiclone was only FDA approved in 2004, while zolpidem was approved in 1987. The most likely reason for our patient’s behavior is an eszopiclone-induced parasomnia; however, eszopiclone-induced intoxication with paranoia and anterograde amnesia is also a viable explanation. Our hypothesis that our patient was suffering from a parasomnia is supported by the pharmacologic profile of eszopiclone, as well as the patient’s girlfriend, who noted in the interview that “it was like he wasn’t there or something” and “it was like he was asleep, but his eyes were open.” To our knowledge, our case represents the first reported incidence of eszopiclone-induced parasomnia with subsequent suicide attempt.
Conclusion
The possibility for adverse effects, including life-threatening events, when taking eszopiclone should be considered by all prescribers. The pharmacological profile of eszopiclone suggests a potential for a greater risk of adverse events than with other benzodiazepine-like hypnotics such as zolpidem, which has a one-percent risk for sleep-related amnestic behaviors.[10] This risk increases further with concomitant administration of monoaminergic drugs like SSRIs. The risk for these behaviors among patients taking eszopiclone is yet to be quantified and presents an opportunity for future research endeavors. Regardless, other evidence-based treatments for insomnia (e.g., cognitive behavioral therapy, biofeedback, sedating antidepressants) should always be considered prior to sedative-hypnotic administration, and caution should be exercised when prescribing these medications.
References
1. Canaday BR. Amnesia possibly associated with zolpidem administration. Pharmacotherapy. 1996;16(4):687–689.
2. Harazin J, Berigan TR. Zolpidem tartrate and somnambulism. Mil Med. 1999;164(9):669–670.
3. Sattar SP, Ramaswamy S, Bhatia SC, Petty F. Somnambulism due to probable interaction of valproic acid and zolpidem. Ann Pharmacother. 2003;37(10):429–1433.
4. Gibson CE, Caplan JP. Zolpidem-associated parasomnia with serious self-injury: a shot in the dark. Psychosomatics. 2011;52(1):88–91.
5. Chong Y, Fryar CD, Gu Q. Prescription sleep aid use among adults: United States, 2005–2010. NCHS data brief, no 127. Hyattsville, MD: National Center for Health Statistics; 2013.
6. Huang MP, Radadia K, Macone BW, et al. Effects of eszopiclone and zolpidem on sleep-wake behavior, anxiety-like behavior, and contextual memory in rats. Behav Brain Res. 2010;210(1):54–66.
7. Schwartz LM, Woloshin S. Lost in transmission – FDA drug information that never reaches clinicians. N Engl J Med. 2009. 361(18): 1717-1720. doi: 10.1056/NEJMp0907708.
8. European Medicines Agency: EMEA/H/C/000895 – Withdrawal Assessment for Lunivia 2009. EMAhttp://www.ema.europa.eu/docs/en_GB/document_library/Application_withdrawal_assessment_report/2010/01/WC500061611.pdf. Accessed July 2015.
9. Holbrook AM, Crowther R, Lotter A, Cheng C, et al. Meta-analysis of benzodiazepine use in the treatment of insomnia. Can Med Assoc J. 2000;162(2):225–233.
10. Jerzy Cubala W, Gabrielsson A. Sleep related amnestic behaviors due to zolpidem. Bull Clin Psychopharmacol. 2014;24(2):189–194.
11. Smith KS, Engin E, Meloni EG, Rudolph U. Benzodiazepine-induced anxiolysis and reduction of conditioned fear are mediated by distinct GABA(?) receptor subtypes in mice. Neuropharmacology. 2012.;63(2):250-258.
12. Dolder CR, Nelson MH. Hypnosedative-induced complex behaviours: incidence, mechanisms, and management. CNS Drugs. 2008;22(12):1021–1036.
13. Jones KA, Nielsen S, Bruno R, etal. Benzodiazepines: their role in aggression and why GPs should prescribe with caution. Aust Fam Physician. 2011;40(11):862–865.
14. Howell MJ. Parasomnias: an updated review. Neurotherapeutics. 2012;9(4):753–775.
15. Longo LP, Johnson B: Addiction: part I. benzodiazepines – side effects, abuse risk and alternatives. Am Fam Phys. 2000;61(7):2121–2128.
16. Tasman A, Kay J, Lieberman JA (eds). Psychiatry, 3rd ed, vol 1. Chichester, England: John Wiley & Sons: 2008;1186–1200, 2603–2615.
17. Zellner M, Watt D, Solms M, and Panksepp J. Affective neuroscientific and neuropsychoanalytic approaches to two intractable psychiatric problems: why depression feels so bad and what addicts really want. Neurosci Biobehav Rev. 2011;35(9):2000–2008.
18. Albrecht B, Staiger PK, Hall K, et al. Benzodiazepine use and aggressive behaviour: a systematic review. Aust N Z J Psychiatry. 2014;48(12):1096–1114.
19. Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? a prospective study in the general population. J Psychosom Res. 2008;64(4):443–449.
20. Masubuchi Y, Kawaguchi Y. Time-dependent Inhibition of CYP3A4 by sertraline, a selective serotonin reuptake inhibitor. Biopharm Drug Dispos. 2013;34(8):423–430.
21. Najib J. Eszopiclone, a nonbenzodiazepine sedative-hypnotic agent for the treatment of transient and chronic insomnia. Clin Ther. 2006;28(4):491–516.
22. Selvaraj V, Skaf M, Sharma A, et al. Eszopiclone-induced psychosis. Innov Clin Neurosci. 2012;9(10):11.
23. Ben-Hamou M, Marshall NS, Grunstein RR, et al. Spontaneous adverse event reports associated with zolpidem in Australia 2001–2008. J Sleep Res. 2011;20:559–568.
24. Mortaz Hejri S, Faizi M, Babeian M. Zolpidem-induced suicide attempt: a case report. Daru. 2013;21(77).





