 by Yousra BENMAKHLOUF, PhD; Zeineb ZIAN, PhD; Kaoutar BEN MAKHLOUF; Naima GHAILANI NOUROUTI, PR; Amina BARAKAT, PR; and Mohcine BENNANI MECHITA PR
by Yousra BENMAKHLOUF, PhD; Zeineb ZIAN, PhD; Kaoutar BEN MAKHLOUF; Naima GHAILANI NOUROUTI, PR; Amina BARAKAT, PR; and Mohcine BENNANI MECHITA PR
Drs. Benmakhlouf, Zian, Ghailani Nourouti, Barakat, and Bennani Mechita are with Biomedical Genomics and Oncogenetics Research Laboratory, Faculty of Sciences and Techniques of Tangier, at Abdelmalek Essaadi University, Morocco, in Tétouan, Morocco. Dr. Ben Makhlouf is with Boudra Fertility Center for Assisted Reproduction in Fez, Morocco.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Objective. Intellectual disability (ID) is a heterogeneous group of disorders characterized by a congenital limitation in intellectual functioning and adaptive behavior. Our present work aimed to describe the demographic and clinical characteristics in a series of Moroccan individuals with ID living in Fez city and its regions.
Design. It was a prospective and descriptive exploratory monocentric study carried out between October 2014 and July 2019. We selected 186 patients diagnosed with ID at three different centers in Fez city. The data were processed and analyzed using the IBM SPSS version 24.
Results. Our data revealed a high frequency of male patients with ID (67.2% in male patients vs. 32.8% in female patients). The male-to-female ratio was 2.04. The mean age of our patients was 15.52 ±6.59 years (mean±SD), ranging between 2 and 36 years. The mean age of fathers and mothers at the birth of their child with ID was 36 and 28 years, respectively. Several abnormal behaviors were observed: 23.1 percent delayed language learning, 17.7 percent anxiety, 12.9 percent aggressiveness, 19.18 percent concentration problems, and 5.4 percent hyperactivity. Epileptic seizures were the most common mental health disorder (21.72%) observed in our patients. Approximately 25 percent of patients with epilepsy took antiepileptic and/or neuroleptics to prevent the occurrence of seizures.
Conclusion. A significant correlation was observed between ID associated to genetic causes and the increase of consanguinity rate.
Keywords: Demographic characteristics, clinical characteristics, Morocco, intellectual disability, consanguinity
Innov Clin Neurosci. 2020;17(10–12):
Mental disorders are currently known as leading causes of morbidity that affect human populations worldwide. They are diseases of medical, educational, and social importance. Intellectual disability (ID), previously named “mental retardation,” is a neurodevelopmental disorder that, in childhood, is characterized by cognitive deficits and overall level of intelligence, including cognitive functions, language, motor skills, and social performance.1 According to the American Psychiatric Association, in Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), people with ID were classified based on daily skills and diagnosis criteria rather than on a specific intelligence quotient (IQ) score. Thus, five forms of ID were distinguished: 1) individuals with profound ID (IQ<20) are characterized by significant delays in the development of all areas and obvious physical and congenital abnormalities, 2) individuals with severe ID (IQ 20–34) are characterized by considerable developmental delays in communication, 3) individuals with moderate ID (IQ 35–49) are characterized by noticeable developmental delays in speech and motor skills and could have some physical signs of impairment, like a thick tongue, 4) individuals with mild ID (IQ 50–70) are slower than typical in all developmental areas, and they are characterized by their ability to learn practical life skills and blend in socially, and finally, 5) adults with borderline ID (IQ 70–80) who live in supported residential settings, either independently or with others.
ID is a heavy load for the individuals’ families and the society.2–4 Its prevalence is estimated at three percent, and its etiology is particularly heterogeneous with causes that are diverse and poorly identified.2 Thus, its etiopathogenesis is still unexplained in almost 50 percent of cases,5 which limits its therapeutic and preventive resources and presents a challenge for physicians.
According to Curry’s 1997 census,7,8 factors causing ID are classified into two categories: innate and acquired causes. These latter are less frequent than the innate causes. Depending on its etiology, ID can be syndromic (S-ID) if it is associated with other clinical, metabolic, or radiological features, and nonsyndromic (NS-ID) when it is the only manifestation of the disorder. Reduced intellectual abilities are the dominant feature of this disorder.2,3 According to the World Health Organization (WHO),8 individuals with an Intelligence Quotient score of less than 70 (IQ<70) are considered intellectually disabled. Thus, based on IQ score, ID is classified into five categories: profound, severe, moderate, mild, and borderline intellectual functioning. Mild ID (IQ 50–70) was reported in 75 to 90 percent of individuals.9
To the best of our knowledge, very few studies have studied ID in the North African population and especially in Moroccan patients. Only one retrospective study about chromosomal abnormalities in Moroccan patients with ID has been published recently.10 The main objective of this pilot study was to describe the demographic and clinical characteristics of Moroccan patients with ID living in the city of Fez and its regions.
Subjects and Methods
Patients. This was a descriptive and prospective study carried out between October 2014 and July 2019. We selected 186 subjects with ID at three mental health centers in Fez city: Attawassol center for mentally retarded, Mafatih Arrahma, and Prince Moulay Abdellah foundation. The selection of patients was done following the guidelines of the Ethics Committee and based on family and clinical history and patient care. Their ages ranged from 2 to 36 years, and their IQs were 70 or lower. We have excluded from our cohort the patients presenting Down Syndrome or autism to prevent the overstatement of the etiologic diagnosis level.
Tutors of the participants and center directors, in the case of orphan subjects, have signed written consent. Ethics approval for this work was obtained from the University Hospital Ethics Committee in the Faculty of Medicine and Pharmacy in Fez city, Morocco.
Statistical analysis. The data were processed and analyzed using the IBM SPSS version 24 Statistical Package for the Social Sciences software. The results were expressed in percentages. A two-sided P value <0.05 was considered statistically significant.
Results
Demographic information. This study included urban and rural Moroccan patients living in Fez city and its regions and shared overall similar socioeconomic conditions and lifestyle. Most (67.2%) of our patients were male, while female patients represented only 32.8 percent. It was a young population, consisting of children, adolescents, and adults aged between 2 and 36 years old. The mean age of our patients was 15.52 ± 6.59 years (mean±SD). More than half of the patients belonged to the 2-to-22-year age groups (38.2% were between 2 and 12 years, 46.2% were between 13 and 22 years). The male-to-female ratio was 2.04. Table 1 shows the patients’ demographic information.
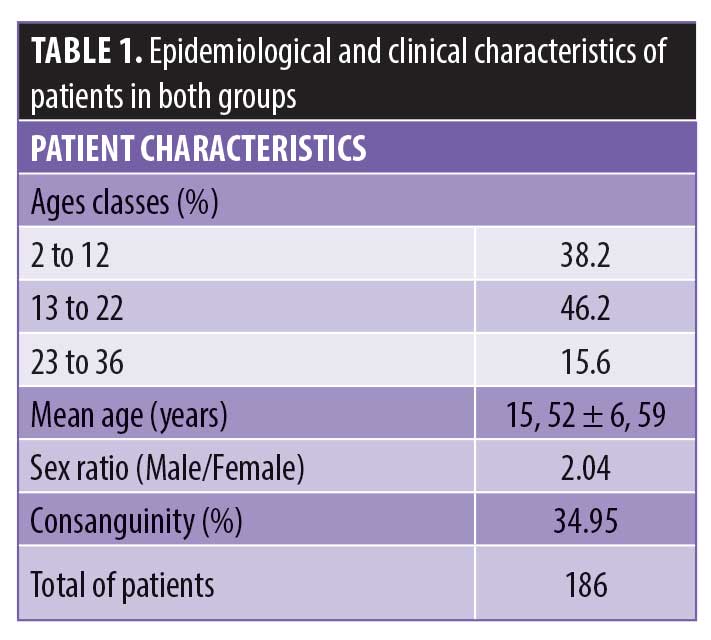
The father’s age at the birth of their child with ID ranged between 20 and 74 years. The mean age was 36±8.25 years. The mother’s age at the birth of their child with ID was 17 to 41 years. The mean age was 28±7.4 years. The majority of mothers (85.1%) had between 17 and 37 years. This showed that most mothers were young.
Approximately 43 percent of fathers worked in the unstructured sector and 32.2 percent in the structured sector, while 13 percent were merchants, 6.8 percent were unemployed, and 5.1 percent were teachers. Regarding the mothers, 79.8 percent were housewives, 9.3 percent were in the unstructured sector, 5.5 percent were teachers, 3.8 percent were in the structured sector, 1.1 percent were in healthcare, and 0.5 percent were merchants.
Clinical characteristics. All patients of our series were diagnosed with mild (55<IQ<70) and NS-ID. The IQ was evaluated using Wechsler standardized tests or a questionnaire established by the receiving center. The diagnosis of patients with ID has been established using a parent questionnaire that evaluates the adaptive skills of the patient in the four domains of the Vineland Adaptative Behavior Scale (communication, daily living skills, socialization, and motor skills). Several abnormal behaviors of ID were observed in our patients. The most common behavioral signs in our series were delayed language learning (23.1%) and concentration problems (19.18%) (Table 2). Epileptic seizures were the most common mental health disorder (21.72%) observed in our patients. There is a relationship between ID and aggressiveness, anxiety, epileptic seizures, memory, and delayed language learning.
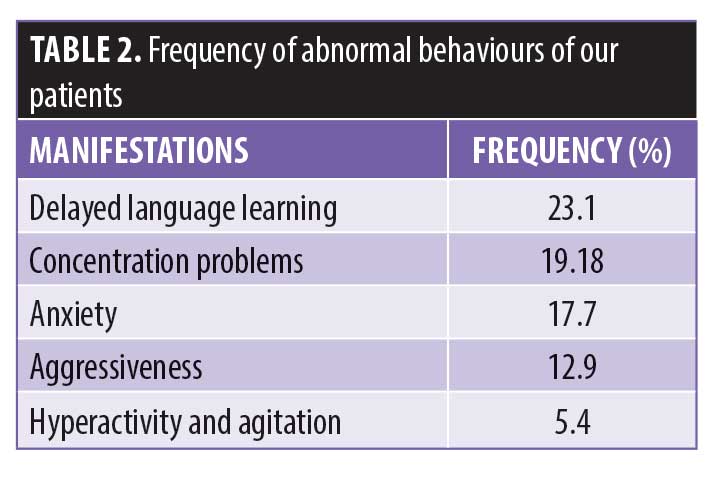
These symptoms were evaluated by a specialist in the center after interviewing parents to obtain a medical and a family history of psychiatric problems. The specialist observed the person’s skills and behavioral signs, such as the interaction between the individual with ID and their family, the ability to communicate with and understand others. The common behavioral signs in our series were delayed language learning, concentration problems, anxiety, aggressiveness, hyperactivity, and agitation.
There are various risk factors that are responsible for or influence the disease, either genetic (heredity, syndromes), environmental (prematurity, infections, accidents, and trauma), or unexplained. In our study, a positive family history of ID has been noted in more than half (59%) of patients, of which 34.95 percent were due to consanguinity. We found that 41 percent of our patients had environmental factors (9.8% were prenatal, 17.4% were perinatal, and 13.6% were postnatal) (Table 3).
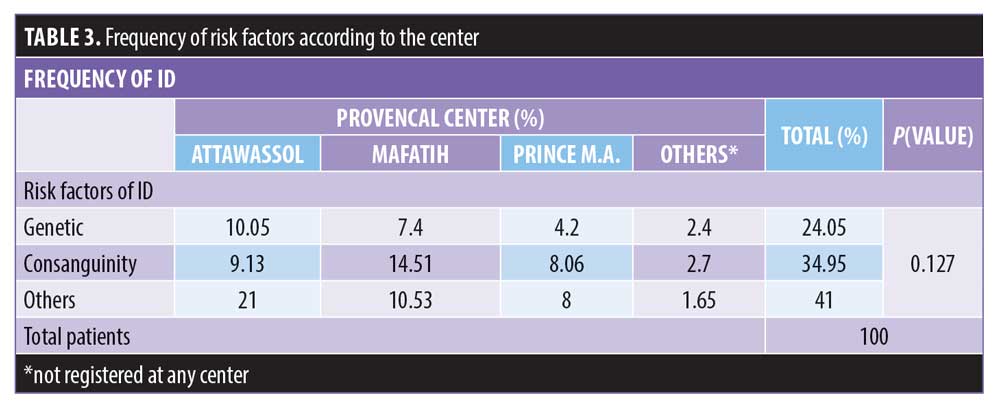
There is a heterogeneity of risk factors responsible for ID, and the rate of consanguinity is higher in patients enrolled at the “Mafatih Arrahma” center.
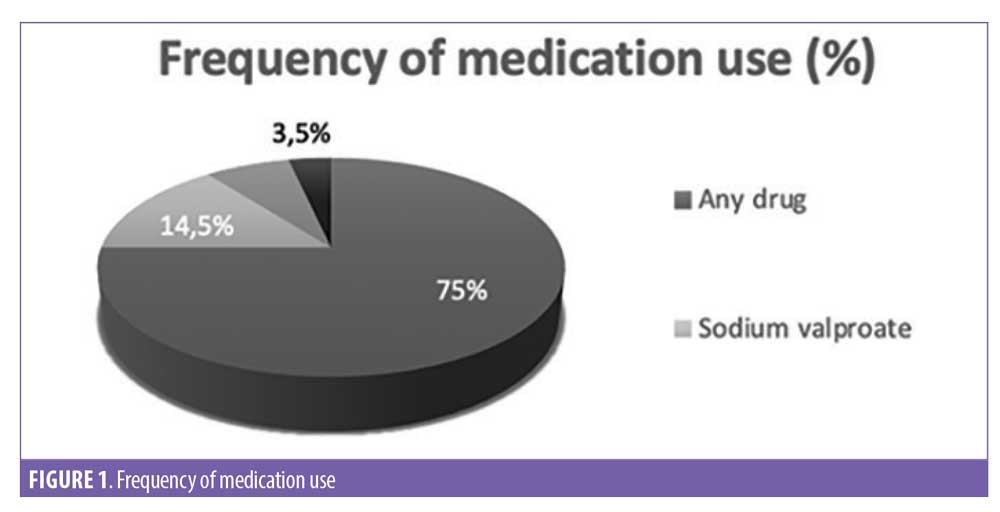
Psychotropic medications. In general, the treatments of ID were symptomatic and not curative. While the ID cannot be treated, per se, co-occurring mental health conditions/disorders are treatable. The majority of medications prescribed for the population studied were neuroleptics and neurodepressants to alleviate epileptic seizures. We found that 75 percent of patients with epilepsy did not take medication or they stopped treatment after decreasing seizures. Among the 25 percent of patients with epilepsy that regularly took their medication, 14.5 percent were monotherapy, seven percent were ditherapy, and 3.5 percent were polymedic (3 to 4 different molecules per day). Association between more than one drug was described only if the frequency of seizures was increasing (Figure 1).
Discussion
Intellectual disability is a serious problem of public health that affects many people from several countries around the world, including African countries. In Morocco, this kind of disorder has not reached great importance at this point in time. Due to the insufficient knowledge of this disease, and to enrich the literature of ID in our country, our research aimed to describe the demographic and clinical characteristics of ID in a series of Moroccan patients native and/or resident in Fez city and its regions. Our study includes 186 urban and rural Moroccan patients with ID enrolled at three mental health centers in Fez city and its regions: “Attawassol center for mentally retarded,” “Mafatih Arrahma,” and “Prince Moulay Abdellah Foundation”. This population group overall shared similar socioeconomic conditions and lifestyles.
In accordance with literature data, a high male predominance is observed (67.2% vs. 32.8%) in our series, with a sex ratio of 2.04.12,13 This excess of male patients could be explained by mutations in X-linked genes13 and the fact that mothers can transmit the X chromosome, causing ID to their child.14 However, some reports showed that this slanting male-to-female ratio cannot be entirely explained by the X-linked gene defects.4 There are other factors proposed, such as behavioral differences, the perinatal vulnerability in men, or risk factors related to the X chromosome causing ID.15 Some gene mutations have also been proposed to be the cause of marginal IQ decrease and shift its distribution to the left in male patients, which would be sufficient to account for the strong male excess observed in mild ID.4 Data analysis showed that almost all (98.9%) of our patients visited the center for mental health after the age of 7 years (legal age of education) to benefit from integration and education. In fact, in Morocco, individuals with ID did not have medical coverage for diagnosis, treatment, and rehabilitation. Moreover, there are no public specialized institutions guaranteed to take them, and only some nongovernmental organizations (NGOs)—partially supported or not supported by the state—are available, as well as some educational associations. Nevertheless, this remains limited and insufficient.
Although its etiology remains unknown in more than 60 percent of the cases,6 genetic, environmental, and unexplained factors can be involved in ID. Our results showed that 41 percent of the ID causes were environmental, during prenatal or postnatal stage (prematurity, infections, accidents, and trauma), or unexplained, leading to brain damage occurring at a critical stage of development. Generally, in our country, there are 25.9 percent of births carried out without any medical or paramedical assistance.16 This rate reaches 43.3 percent in rural areas. Among these distributions, 1 in 6 are complicated cases. Thus, the newborn could present many physical, sensory, and neurological risks.16 Stevenson17 and Rogers6 have described these factors as follows: 18 percent were environmental causes, 29 percent were genetic causes, and 56 percent were unexplained causes. In industrialized countries, studies have consistently revealed that prenatal and genetic causes predominated.18,19 Our results showed that 73.6 percent of our patients with ID were from urban areas and 26.4 percent were from rural areas. In fact, access to technological interventions, advanced medical care, and advanced diagnostic tests might not be available in the same way throughout all groups in society and especially in rural areas.15 In Morocco, the prevalence of disability is relatively higher in rural than in urban areas (5.5%: 727,833 persons vs. 8%: 975,591 persons).20
As it has been mentioned above, 59 percent of our patients had a familial form of ID, and consanguinity is noted in 34.95 percent of this group. We observed that the rate of consanguinity (first degree) was higher in patients enrolled at the “Mafatih Arrahma” center, which is located in a popular region from Fez city. This rate (34.95%) remains lower than that reported in Tunisian patients with ID (52.4%) who were born from consanguineous parents (more than 60% were first cousins).21 In fact, the national frequency of consanguinity in Morocco ranged between 19.81 and 28 percent.22 Moreover, interfamily marriages are considered a sociocultural practice in our population. This rate remains comparable with that reported in some Arab countries of the Middle East–North Africa (MENA) region, such as Algeria, Egypt, Lebanon, and Tunisia.23,24 It was reported that consanguinity contributes considerably to the occurrence of brain disorders since a child of consanguineous parents has an increased risk to have common mood disorders and psychoses.25 Indeed, avoiding this practice, by discouraging close consanguinity by awareness programs or during premarital counseling, could have a significant impact by decreasing the rate of ID in our country.
The mean age of the children’s mother and father in our series was 28 and 36 years, respectively. A child whose father was 45 years old at birth is 3.5 times more likely to have autism and 13 times more likely to have attention problems than a child whose father was 24 years.26, 27 Previous studies suggested that as aging occurs, increased de novo mutations in men’s sperm might play an important role in increasing rates of cognitive disability.29,31 Although parents of our patients were young at the birth of their child, this latter suffered from ID. Our statistical analysis demonstrated that there was a weak correlation (r=0.101) between the fathers’ age at the birth of their first child and the number of brothers with ID. Similarly, the majority of mothers were young (17–41 years old) in our series. The increase in the mother’s age can also lead to several mental health problems, including common psychiatric disorders.29 We also found a weak correlation (r=0.101) between the mothers’ age at the birth of her first baby and the number of brothers suffering from the disease. In contrast to some studies that reported that the type of parent function, leading to poisoning (plumb) or exposure to ionizing products, can influence the fetus development during pregnancy,30 we found that a parent’s occupations did not have any impact on the disease since all parents worked in sectors without chemical or toxic products.
Delayed language learning was the most common symptom (23.1%) found in our series. This is in accordance with prior reports that suggested a correlation between ID and disorder severity in patients with ID and delayed language learning.31 The frequency of epileptic seizures (21.72%) observed in our group of patients with ID was in agreement with the literature data (20–40%),32 and comparable to the Tunisian patients with epilepsy and ID (21.72% vs. 27.5%). Aggressiveness was found in 12.9 percent of our patients. This behavior is a form of communication. It might be in response to psychological distress or a biomedical condition (medical, psychiatric, neuropsychiatric, genetic). Psychopharmacological (antipsychotic drugs) and psychological treatments are often prescribed to treat the aggressive behavior in ID. Thus, anxiety and anger are both causes of the “fight or flight” response.33 A quarter of our patients with epilepsy took antiepileptic and/or neuroleptics drugs to prevent the occurrence of crises. This could lead to adverse or severe side effects related to drug interactions, which might then escalate to a negative impact on a patient’s life.34
Limitations. Our study had some limitations. Intellectual disability is generally unknown by the Moroccan population, which probably influenced the size of our series. The monocentric character of this work is due to the lack of ID health centers in our country, and because none of the patients with ID had free medical coverage that allows them the gratuity of care and transport. The lack of detailed clinical information of patients, because of the high cost of analysis, makes their diagnosis difficult and incomplete. In fact, in emerging countries such as Morocco, there is a high rate of illiteracy, low socioeconomic status, and low disease recognition, which is related to low awareness of the disease at primary points of care and an inadequate number of specialists. According to the 2014 population census results,34 12.5 percent of citizens in Morocco live under the national poverty line (the proportion is 7.9% in urban and 19.4% in rural areas). In addition, unemployment rates are high, and only 17 percent of individuals have health insurance. All these factors make access to healthcare limited, which contributes substantially to the small number of patients that the medical center received. Thus, our results should be taken carefully, and no firm conclusions could be drawn from our work. More investigations with extra samples from patients with ID from multiple other centers are needed to validate these preliminary findings and to confirm them.
In fact, screening, diagnosis, and monitoring of ID is a major challenge that needs a multidisciplinary collaboration of pediatricians, geneticists, orthophonists,11 psychiatrists, psychologists, and child neurologists.35 Neurological, psychometric, and complementary examinations (karyotypes, brain imaging indicated, scanner, or magnetic resonance imaging [MRI]) can be indicated according to the profile of each patient. Parents also should consult more precociously to ensure a rapid and efficient search for the etiology.
Conclusion
As far as we know, studies about ID in the Moroccan population are scarce. Our results showed some particularities of demographic and clinical features of ID in our country. The consanguinity rate was significantly increased in our series; hence, the follow-up of pregnancies resulting from this type of marriage is necessary. These findings could enrich the literature of ID among the studied region of Morocco by given data for comparison to other research centers.
Due to the high cost of diagnosis and treatment, difficulties in follow-up, socioeconomic factors of the population, and establishing of prenatal diagnosis, which could reduce the risk of having a child with the ID, represents a serious challenge in Morocco.
Acknowledgments
The authors would like to acknowledge Association of “Espace Femme Marocaine”, “Entraide Nationale”, “Attawassol Center for the mentally retarded”, “Mafatih Arrahma”, “Prince Moulay Abdellah Foundation” in Fez, for their collaboration and help to facilitate the recruitment of the patients.
References
- Institut national de la santé et de la recherche médicale (Inserm) site. Déficiences Intellectuelles. Collection Expertise collective. Montrouge: EDP Sciences;2016 :15–1157 – http://hdl.handle.net/10608/6816. Accessed 14 November 2020.
- Miot S, Jeandel C, Baghdadli C, Blain H. Le vieillissement des personnes en situation de handicap mental et le cas particulier du syndrome de down. NPG Neurol Psychiatr (Gériatrie). 2018;18(104):69–77.
- Spitzer RL, Endicott J, Micoulaud Franchi JA. Medical and mental disorder: Proposed definition and criteria. Ann Méd Psychol Rev Psychiatr. 2018;176(7):656–665.
- Ropers HH. X-linked mental retardation: Many genes for a complex disorder. Curr Opin Genet Dev. 2006;16(3):260–269.
- Iqbal M, Baig MA, Bhinder MA, Zahoor MY. Factors causing mental retardation. Asian J Appl Sci. 2016;5:11.
- Rogers RC, Stevenson RE, Simensen RJ, et al. Finding new etiologies of mental retardation and hypotonia: X marks the spot. Dev Med Child Neurol. 2008;50(2)104–111.
- Abedini SS, Kahrizi K, Behjati F, et al. Mutational screening of ARX gene in Iranian families with x-linked intellectual disability. Arch Iran Med. 2012;15(6):361–365.
- Bussy G. Approche inter-syndromique des processus cognitifs en jeu dans la déficience intellectuelle et la dyspraxie verbale: Vitesse de traitement de l’information, mémoire de travail et apprentissage procédural. 2010. Université Lumière Lyon 2. http://theses.univ-lyon2.fr/documents/lyon2/2010/bussy_g#p=0&a=top. Accessed 14 November 2020.
- Toniolo D. In search of the MRX genes. Am J Med Genet. 2000:97:221–227
- Belkady B, Elkhattabi L, Elkarhat Z, Zarouf L. Chromosomal abnormalities in patients with intellectual disability: a 21-year retrospective study. Hum Hered. 2018;83(5):274–282.
- Stevenson RE, Procopio-Allen A, Schroer JR, Collins SJ. Genetic syndromes among individuals with mental retardation. Am J Med Genet A. 2003;(1):29–32.
- Rogers CR, Roger ES, Simensen R, et al. Finding new etiologies of mental retardation and hypotonia: X marks the Spot. Dev Med Child Neurol. 2008;50(2):104–111.
- Raymond FL. X linked mental retardation: A clinical guide. J Med Genet. 2005;43(3):193–200.
- Goldenberg A, Saugier-Veber P. Retards mentaux d’origine génétique. Pathol Biol. 2010;58(5):331–342.
- Leonard H, Wen X. The epidemiology of mental retardation: challenges and opportunities in the new millennium. Ment Retard Dev Disabil Res Rev. 2002;8(3):117–134.
- Ministère de la Solidarité, de la Femme, de la Famille et du Développement Social. La prévention des handicaps liés à la grossesse et à l’accouchement. (In.) Guide d’information et de sensibilisation: 2017:48.
- Stevenson RE, Procopio-Allen AM, Schroer RJ, Collins JS. Genetic syndromes among individuals with mental retardation. Am J Med Genet. 2003;123A(1)29–32.
- Hunter GW. Outcome of the routine assessment of patients with mental retardation in a genetics clinic. Am J Med Genet. 2000;90:60–68
- Jauhari P, Boggula R, Bhave A, et al. Aetiology of intellectual disability in paediatric outpatients in Northern India: aetiology of intellectual disability. Dev Med Child Neurol. 2011;53(2)167–172.
- HCP site. Les indicateurs sociaux du Maroc. 2018. HCP-Maroc https://www.hcp.ma/downloads/Indicateurs-sociaux_t11880.html. Accessed 14 November 2020.
- Trabelsi M, Chelly I, Maazoul F, et al. Epidemiologic and clinical characteristics of 458 Tunisian patients with intellectual deficiency and a reconsidered diagnostic strategy. Eur J Med Genet. 2013;56(1)13–19.
- Talbi J, Khadmaoui AE, Soulaymani AEM, Chafik AEA. Etude de la consanguinité dans la population marocaine. Impact sur le profil de la santé. Antropo. 2007;15:1-11.
- Maguire A, Tseliou F, O’Reilly D. Consanguineous marriage and the psychopathology of progeny: a population-wide data linkage study. JAMA Psychiatry. 2018;75(5):438.
- Benkou F, Metri AA, Chaif O. Caractérisation anthropososio-culturelle de la population endogame des Monts de Traras (Beni Ouarsous) dans l’Ouest Algérien par la consanguinité et le lien de parenté. Antropo. 2018;39:49–58.
- Maguire A, Tseliou F, O’Reilly D. Consanguineous marriage psychopathology of progeny: A population-wide data linkage study. JAMA Psychiatry. 2018;75(5):438.
- Kong A, Frigge ML, Masson G, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature. 2012;488(7412):471–475.
- Das M, Al-Hathal N, San-Gabriel M, et al. High prevalence of isolated sperm DNA damage in infertile men with advanced paternal age. J Assist Reprod Genet. 2013;30(6)843–848.
- Neelam T, Savitri V. An epidemiological study of mental retardation without a common genetic cause in the population of himachal pradesh, India. Int J Environ Ecol Fam Urban Stud. 2017;7(5)23–32.
- Wong WSW, Solomon BD, Bodian DL, et al. New observations on maternal age effect on germline de novo mutations. Nat Commun. 2016;7:10486.
- Yazbecka C, Cheymolc BJ, Dandresd AM, Barbéry-Courcoux AL. Intoxication au plomb chez la femme enceinte et le nouveau-né: bilan d’une enquête prospective. Pediatrics. 2007;14:15–19
- Platt JM, Keyes KM, McLaughlin KA, Kaufman AS. Intellectual disability and mental disorders in a US population representative sample of adolescents. Psychol Med. 2019;49(6):952–961.
- Espie CA. Psychopathology in people with epilepsy and intellectual disability; An investigation of potential explanatory variables. J Neurol Neurosurg Psychiatry. 2003;74(11):1485–1492.
- White P, Chant D, Edwards N, et al. Prevalence of intellectual disability and comorbid mental illness in an Australian community sample. Aust NZJ Psychiatry. 2005;39(5):395–400.
- Kaur H, Kumar B, Medhi B. Antiepileptic drugs in development pipeline: A recent update. eNeurologicalSci. 2016;4:42–51.
- Tylenda B, Beckett J. Assessing mental retardation using standardized intelligence tests. Int Rev Res Ment Retard. 2007;34:27–97.





