 by Sushma Dahal, MPH; Meghnath Dhimal, PhD; Sagun Ballav Pant, MD; Pawan Sharma, MD; Kedar Marahatta, MD; Nagendra Luitel, MA; Suraj Shakya, PhD; Sweta Labh, BSc Nursing; Saroj Prasad Ojha, MD; Anjani Kumar Jha, MD; and David V Sheehan, MD, MBA, DLFAPA
by Sushma Dahal, MPH; Meghnath Dhimal, PhD; Sagun Ballav Pant, MD; Pawan Sharma, MD; Kedar Marahatta, MD; Nagendra Luitel, MA; Suraj Shakya, PhD; Sweta Labh, BSc Nursing; Saroj Prasad Ojha, MD; Anjani Kumar Jha, MD; and David V Sheehan, MD, MBA, DLFAPA
Drs. Dhimal and Jha and Ms. Dahal and Ms. Labh are with the Nepal Health Research Council in Kathmandu, Nepal, and are members of the Technical Working Group, National Mental Health Survey, in Nepal. Drs. Pant, Shakya, and Ojha are members of the Technical Working Group, National Mental Health Survey, in Nepal and are with the Department of Psychiatry and Mental Health, Institute of Medicine at Tribhuvan University in Kathmandu, Nepal. Dr. Sharma is a member of the Technical Working Group, National Mental Health Survey, in Nepal and with the Patan Academy of Health Sciences in Lalitpur, Nepal. Dr. Marahatta is a member of the Technical Working Group, National Mental Health Survey, in Nepal. Mr. Luitel is a member of the Technical Working Group, National Mental Health Survey, in Nepal and is with the Transcultural Psychosocial Organization Nepal in Kathmandu, Nepal. Dr. Sheehan is with the University of South Florida College of Medicine in Tampa, Florida.
FUNDING: This study was funded by the Government of Nepal and the World Health Organization Country Office for Nepal.
DISCLOSURES: David V Sheehan is the author and copyright holder of the MINI tool used in this survey. He receives royalties through multiple tiers for its licensing and use. Dr. Sheehan did not receive any revenue for this study. All the authors declare no conflict of interest.
ABSTRACT: Objective. Learning from pilot studies is crucial for the successful implementation of large-scale surveys. In this manuscript, we present the lessons learned for instrumentation and survey methods from a pilot national mental health survey conducted in Nepal.
Design. We conducted a cross-sectional study among 1,647 participants aged 13 years and older in three districts of Nepal. We used the Nepali translated standard adult and adolescent versions of the Mini International Neuropsychiatric Interview (MINI) 7.0.2 for Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) to do face-to-face structured diagnostic interviews. In addition, we included questionnaires on help-seeking behavior and barriers in accessing care.
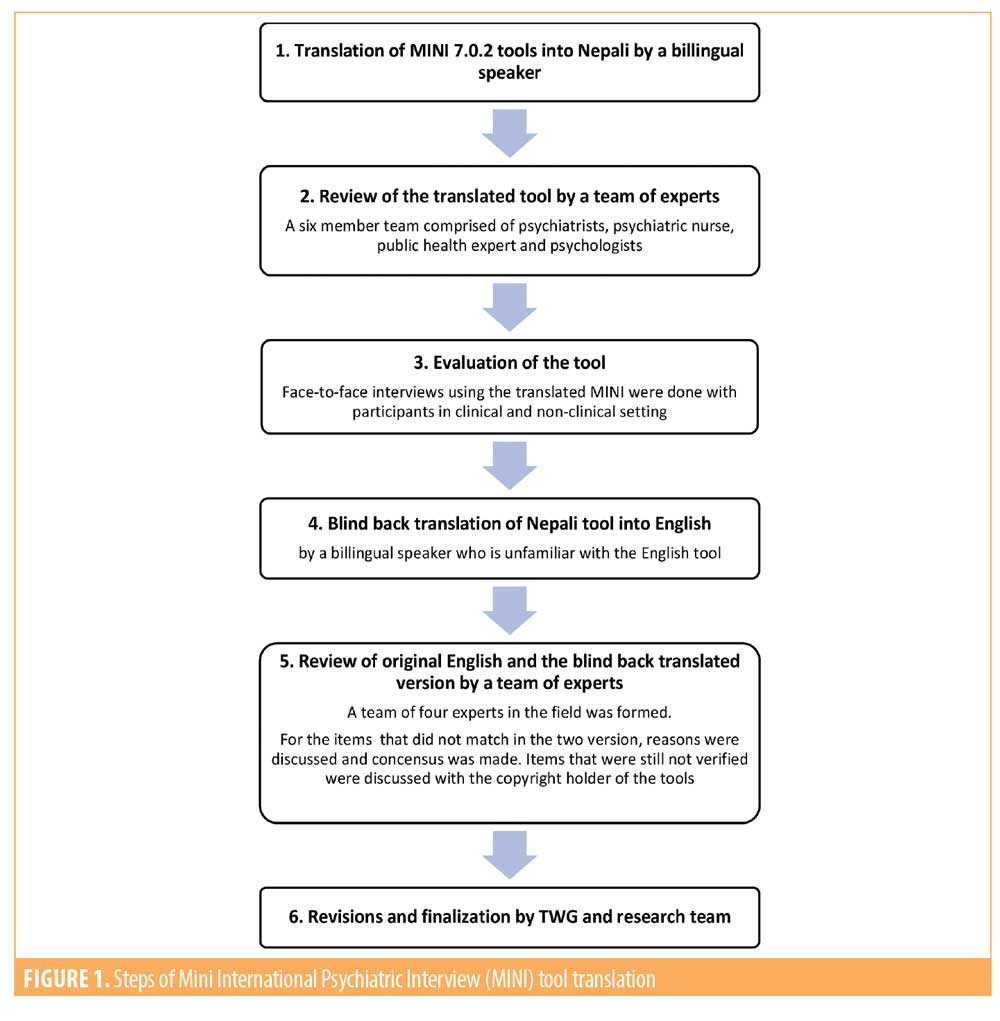
Results. We used a six-step procedure to translate and fit the tools in the context of Nepal. We conducted pretesting to evaluate the Nepali translated tools and adaptations, such as the addition of bridging sentences at the start of different modules. We identified different challenges during the tools administration and the ways to minimize reporting bias during data collection.
Conclusion. The pilot survey identified the areas for improvement in survey tools, techniques, and methodology. The lessons learned from the pilot survey and the resulting corrective recommendations helped in more successful implementation of the Nepal national mental health survey.
Keywords: Diagnostic interview, Epidemiology, Lessons learned, Mental health survey, Nepal, Pilot survey, Study instruments
Innov Clin Neurosci. 2020;17(10–12):
Mental health is an emerging global health problem. More than 85 percent of the world’s population lives in low- and middle-income countries (LMICs), and more than 80 percent of people who have mental disorders reside in these countries.1 Despite the increased vulnerability of developing mental health disorders among Nepalese people,2–5 nationally representative data on the prevalence of mental disorders is lacking. Previous studies conducted in Nepal used either limited nonrepresentative samples or included few mental disorders, such as depression and anxiety only. There was no homogeneity in the use of diagnostic tools, limiting the ability to compare the findings. To fill this gap, the Nepal Health Research Council (NHRC) began planning the first national-level mental health survey in 2017. This national survey aimed to a) investigate the prevalence of mental disorders among adolescents and adults in Nepal, and b) assess help-seeking behavior and barriers to seeking care among those with the disorders.
As a first step, we selected an internationally validated structured diagnostic interview, the Mini International Psychiatric Interview (MINI) 7.0.2 for Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5),6, 7 as a major tool of data collection for this study. Then, we conducted a pilot survey to assess the feasibility of undertaking the full-scale national epidemiology study. We wanted to test survey tools and techniques, evaluate participants’ response rate, identify practical problems in the field; determine the human resource need/time and cost for the national survey, and to estimate the prevalence of mental disorders in the selected pilot survey areas. This paper discusses the lessons learned from the pilot survey and their implications for the national-level study.
Materials and Methods
Study design. This was a cross-sectional descriptive pilot study using face-to-face interviews in a sample of noninstitutionalized residents of Nepal. The study was designed to explore potential problems that might be encountered in advance of a large national epidemiological study of mental disorders in Nepal.
Study setting. The Federal Democratic Republic of Nepal is a landlocked country in South Asia. Nepal has a diverse ethnic composition with 125 castes and 123 languages recorded in 2011. Nepali is spoken by 77.4 percent of the population (44.6% as the first language and 32.8% as the second language).8 Geographically, Nepal spans three ecological belts: The Northern-Range Mountain, the Mid-Range Hill, and the Southern-Range Terai (flat land). Nepal has seven provinces, 77 districts, and 753 municipalities (local governments). The districts are divided into rural and urban municipalities, which are then divided into wards.9 This pilot study was conducted in three districts (Dhanusha, Bhaktapur, and Dolakha) chosen to represent the Terai (flat land), Hill, and Mountain regions of Nepal, respectively.
Subjects and sampling. Our subjects included 1,647 participants who were noninstitutionalized, aged 13 years and older, from the three districts of Nepal. Among the participants, 276 were adolescents, aged 13 to 17 years, and 1,371 were adults, aged 18 years and older. In view of the absence of nationwide prevalence data on mental disorders from Nepal and the similarity of cultural practices between Nepal and India, we used the prevalence estimates from the recent mental health survey from India conducted using the same diagnostic tool (MINI) to estimate the sample size.10 The sample size for each district was proportionate to the total number of households in the selected districts with the wards considered as the primary sampling units (PSUs), as per Nepal’s census report of 2011.11 A probability proportionate to size (PPS) method was applied to identify PSUs at the district level. From the selected PSUs, we made a household listing with the help of female community health volunteers (FCHVs). We then randomly selected 30 households per PSU for adults and six households for adolescents (randomly selected from 30 households for adults) using random number tables. If more than one eligible adult and adolescent were present in the household, we used a lottery method to select the participant. Ninety-nine percent of those contacted agreed to participate. The final sample was 1,647 (276 adolescents, aged 13 to 17 years, and 1,371 adults, aged 18 years and older).
Study instruments. The primary measures for collecting data on mental disorders for adults were the paper version of the MINI 7.0.2 for DSM-5 for adults and the Mini International Neuropsychiatric Interview (MIN-Kid) 7.0.2 for DSM-5 for adolescents.6,12 The MINI assesses psychiatric disorders using DSM-5 criteria. One of the most widely used psychiatric structured diagnostic interview instruments in the world, the MINI has been used in national level mental health surveys of many countries including India,10 Thailand,13 Morocco,14 and Egypt.15 We licensed the use of the paper version of MINI and MINI-Kid from the developer and copyright holder. As recommended by the study’s Technical Working Group (TWG), we included all the mental disorders relevant in the Nepalese setting for a total of 15 and 23 mental disorders for adults and adolescents, respectively. We planned to revise the number of disorders in the final survey based on the findings from the pilot study. A detailed list of the mental disorders included in the pilot survey has been published elsewhere.16
Other medical disorders, such as epilepsy and dissociative conversion disorder, that are important in the Nepalese context were added as modules to the standard MINI interview for adults. Similarly, epilepsy, dissociative conversion disorder, and intellectual disability modules were added to the standard MINI Kid for adolescents. Interview modules for these additional disorders were prepared by a team of psychiatrists and psychologists and then reviewed and finalized by the TWG. We also administered the Barriers to Accessing Care Evaluation (BACE) and a questionnaire on help seeking-behavior for participants who were diagnosed with any mental disorders in the past 12 months. BACE is a 30-item questionnaire on key barriers to accessing care for mental disorders and has demonstrated validity, reliability, and acceptability.17,18
Tools and techniques of data collection. One of our first challenges was translating the MINI. Although the MINI has been translated and linguistically validated in over 70 languages, it had not been translated into the Nepali language. This meant that both the adult and kid versions of the instrument had to be translated before we could start. Nepal has many ethnic groups and languages. Since it was not feasible for time and budgetary reasons to translate the instrument into more than one language and 77 percent of the population in Nepal speak the Nepali language, we elected to translate the instrument into the Nepali language only.
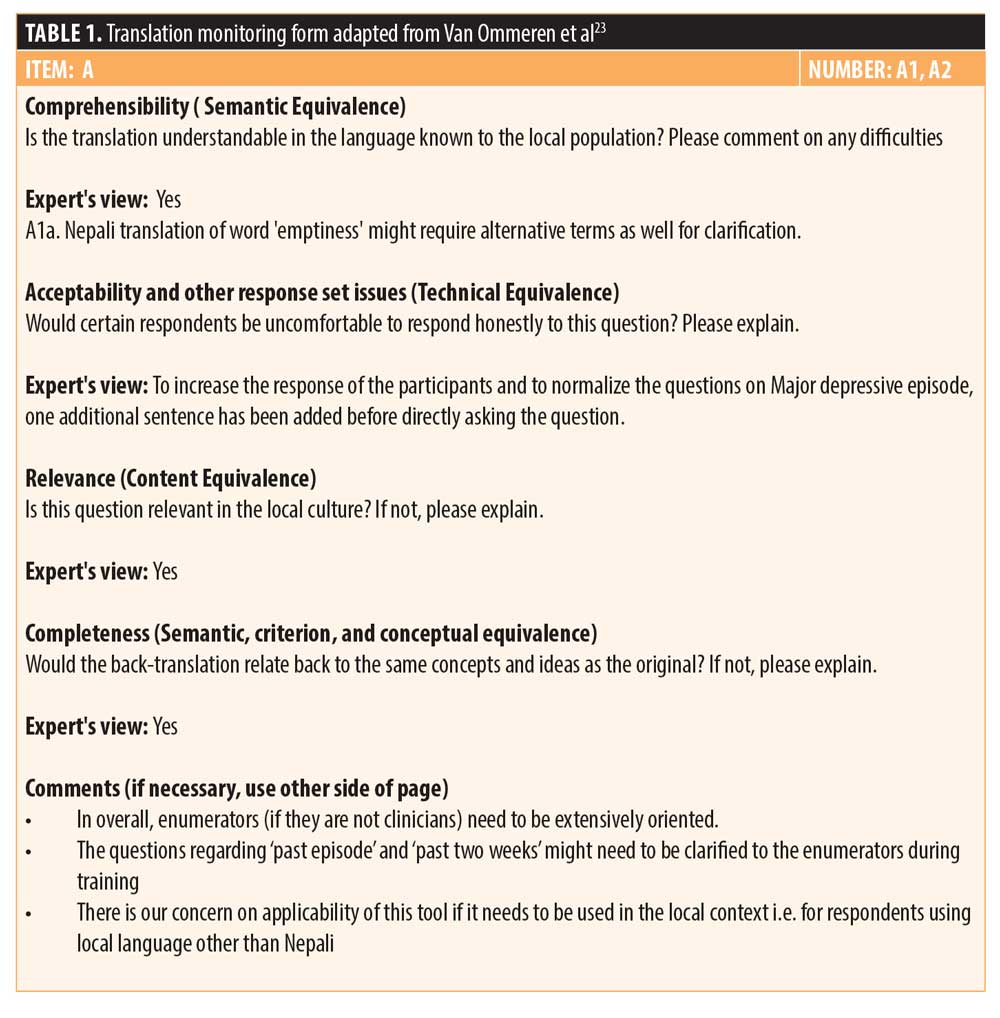
Previous work has addressed the complexities involved in adapting diagnostic instruments to Nepal with its historic isolation, its background of poverty and inequality, and its unique cultural interpretations of health and mental health.19 During the initial phase of MINI tool’s translation, the research team realized that mere verbal translation of the tools would not be sufficient to guarantee conceptual equivalence, criterion equivalence, or content equivalence. To address these issues, we carefully followed guidance in the literature.20–23 We developed an iterative six-step process for translating the instruments (Figure 1). This process included forward and blind back translations of the instruments. Following earlier models,23 we prepared a structured form with four different criteria: comprehensibility, acceptability, relevance, and completeness to be verified in the tools. The comprehensibility criterion addressed whether the translation was understandable to the local population. The acceptability criterion addressed whether a respondent might be “uncomfortable” answering a question directly or if it needed to be modified to more acceptable wording. The relevance criterion addressed the question’s relevance to local culture. Questions about entertainment that refer to video games, mobile games, or television might not be relevant in settings without electricity, for example, and it might be necessary to include other entertainment modes that are relevant. Finally, the completeness criterion addressed whether the back translation related back to the same concepts and ideas as the original question. Each of the experts who verified the forward and back translated tools carefully evaluated these criteria for each item in the MINI. One sample of the monitoring form filled by our experts is shown in Table 1.
Recruitment and training of field data collectors. We recruited 12 field data collectors (FDCs). Each, as a minimum qualification, had to have a bachelor’s degree in nursing or public health. A team of psychiatrists, psychologists, and research experts who were trained online by the copyright holder of the tool provided the FDCs with a one-week training on the survey instruments and the survey methodology. The training was practice-based, focused on building the skills of FDCs in successfully conducting the interview using the given instrument. The initial sessions included an overview of the mental disorders in the tool followed by the discussion on each items of the tool. The remaining sessions incorporated careful observation of demonstration interviews conducted by experts. These were followed by interviews done by the FDCs under supervision. FDCs were provided sufficient level of feedback to ensure that they understood how to do the interviews correctly. Following the training, the FDCs were sent to two villages within the Kathmandu district to pretest the instruments, where they interviewed a total of 138 adults and 30 adolescents. After pretesting, the FDCs engaged in a group discussion and gave feedback to the study planners. We made necessary modifications in the Nepali translations of the instruments based on their feedback.
Home interviews and data collection. Interviews were conducted June 20 to July 20, 2018, by the trained data collectors who made home visits and conducted face-to-face interview with the participants using the paper version of MINI 7.0.2 Adult and MINI-Kid 7.0.2. for DSM-5, questionnaire on help seeking behavior, and BACE.
Data management and analysis. The data were collected on paper and entered into EpiData version 3.1, with pre-set checks and controls, then checked for consistency before entering into the entry format. All the entered data were rechecked to correct any data entry errors. We analyzed the data in IBM SPSS Statistics 23. We summarized the data using descriptive statistics and reported frequencies and percentage values. We examined the prevalence of each of the disorders. We also calculated Cronbach’s alpha values for the selected most common disorders to identify the level of internal consistency between the items in different modules of the Nepali translated version of MINI. For example, in the adult dataset, we calculated the alpha value for current and lifetime major depressive episode, substance use disorder, alcohol use disorder, lifetime psychotic disorder, and items in the suicidality module. This calculation was not performed for the dataset of adolescent respondents because of the small sample size.
Ethical aspects. Approval for the study was provided by the Ethical Review Board (ERB) of the Nepal Health Research Council (NHRC) prior to the start of the study. To facilitate referral for identified cases at risk, we developed a list of health facilities where mental health services are available for each district. We also developed an adverse event management protocol to be able to provide appropriate healthcare to any individual with suicidality and/or a severe mental disorder. Identified cases were referred to the health facility/service based on the previously prepared list. For other common mental disorders, we provided psychoeducation about the need for treatment.
Results
Our goals in this pilot study were to test survey tools and techniques, identify practical problems in the field, evaluate participants’ response rate, determine the human resource need/time and cost for the national survey, and to estimate the prevalence of mental disorders in the selected pilot survey areas.
Testing of survey tools and techniques. During the translation of tools, we gave special care to incorporating sociocultural context. We evaluated the draft version of the translated MINI by interviewing 25 adults and 10 adolescents. This led to the identification of MINI questions that were not easily understood by the participants or were difficult for the interviewer to administer.
At times, the tools translation team encountered problems or failure to reach consensus in reconciling the back translation with the original source translation. For example, question C3d in the manic episode module of the MINI in English addresses “racing thoughts.” When back translated to English from Nepali, the question read “Did you feel that there was quick change in thoughts from one to another?” This occurred because of difficulty in finding Nepali words for “racing thoughts.” We consulted the copyright holder of the MINI who helped us resolve this issue and other similar ones and provided clarity on the diagnostic criterion being probed.
Ratings also posed challenges. For example, on the psychotic disorder module in “b” questions that address potential delusions, the team initially felt that the extent of belief in questions addressing current belief should be “strong.” However, after consulting with the copyright holder, we agreed that delusion of any extent (“a little” or “strong”) are both valuable. Examples of other questions that required consultations were: C7 in the manic episode module, D4k in the panic disorder module, G3a in the obsessive-compulsive disorder module, H5f in the posttraumatic stress disorder (PTSD) module, and N3a in the generalized anxiety disorder module.
Identification of practical problems/cultural issues. Pretesting indicated that field interviewers had unique difficulties with the psychotic disorder module of the MINI. When administering the psychotic disorder module, they reported trouble judging the presence or absence of disorganized, derailed, incoherent, and marked loosening of association. We addressed this issue with further training.
Interviewers also reported difficulty making smooth transitions from one module of the MINI to the next. To address this problem, in consult with the developer of the MINI, we allowed them to use bridging sentences in Nepali. For example, before the major depressive episode module, we allowed them to say:
“Some people share that they feel lonely, depressed, or down most of the time…”
Similarly, before the suicidality module, we allowed them to say:
“These days, we hear many events of suicide. Many people share that they sometime have suicidal thoughts…”
The suicidality module posed other challenges in that respondents became irritable when asked to respond to questions that sounded similar, especially when they had responded “no” to previous questions. To address this irritability, we gave them other wording they could incorporate:
After a “yes” to the first question about suicidal thoughts: “Now I am going to ask about these types of thoughts….. some of the questions may seem unnecessary to you…”
After a “no” to the first question: “It may appear to you that we should not ask you any additional questions on suicidality if you answer ‘no’ to suicidal thoughts, but this can happen to some people. Some people make suicide attempts in the past week even though they had no suicidal thoughts or plans in the past week. So please bear with me as we go through all these questions with everyone, even if they don’t apply to you.”
A cultural issue that emerged in the administration of the alcohol use disorder module is that alcohol use in the Brahmin community is considered taboo. So, when asking a question on alcohol use to someone from the Brahmin caste, we allowed the interviewer to start with a comment such as:
“These days, people from the Brahmin community are also found to drink alcohol….” then proceed with the question: “Have you ever….”
Also, in Nepal, alcohol use is not considered usual among children. To address this issue, we allowed the interviewer to introduce the module this sentence:
“Some children of your age are found to be taking/using alcohol.” They could then go on to ask, “Have you ever tried/used alcohol?”
These introductory sentences had the additional advantage of normalizing the situation before asking a potentially sensitive question.
A practical issue that emerged in administering the alcohol use disorder module was how to quantify the amount of locally prepared alcoholic drink called “rakshi,” “jaad,” and “chayang,” since such drinks are not measured in terms of standard drinks in Nepal. To address this issue, we provided detailed enumerators on types of local alcoholic drink and the amount in local unit that is equivalent to a standard unit of alcohol.24
Another cultural issue that emerged in the anorexia nervosa module was that respondents had trouble recalling their lowest body weight in last three months because they do not routinely monitor their weight.
Additionally, in the course of the pretest we discovered a need to create a list of local words for some technical terms in the questionnaire. For example, the local name in Terai for “atmahatya” (suicide) was identified as “khudkhushi.” Similarly, the local word for “nidra” (sleep) was identified as “neend,” that for “ausadhi” (medicine) identified as “dabai,” that for “upachaar” (treatment) identified as “ilaaj.”
Finally, we noted that for the 30-item BACE questionnaire, some items, e.g., “fear of being recorded in medical record as mentally ill” were not relevant in the Nepalese setting. As a result, it was recommended that in the final survey, the BACE be shortened to meet our needs. We sought permission from the copyright holder of the BACE tool before finalizing this recommendation.
During the main survey, we planned to address these practical issues and challenges further through extensive training and orientation of the FDCs to minimize information bias. No new questions, per se, were added to any module.
Though many of the above revisions were made in the tools after pretesting, based on the experiences of the field interviewers and supervisors, we further identified the strategies to apply during data collection in the national level survey.
Reliability, data management, and analysis. The MINI is a complex instrument requiring a large number of skips and checks. Assessing the inter-rater reliability of the interviewers was not feasible in this pilot survey because of time and budgetary constraints.
In the pilot study, we did examine internal consistency using the intra-class correlation coefficient as a measure of reliability for some of the most common disorders. We found good internal consistency (Cronbach’s alpha >0.8) in the adult data set for current and past major depressive episode. For the substance use disorder and alcohol use disorder, internal consistency was acceptable to good with Cronbach’s alpha scores of 0.78 and 0.82, respectively. For lifetime psychotic disorder the alpha value was acceptable (0.77). In the suicidality module when items with adequate cases were counted, the alpha value was poor (only 0.57). This improved to 0.69 when we dropped during analysis item b2, an item on passive suicidal ideation (in contrast to active suicidal ideation) that seems to have been over endorsed. These results helped us identify items that could have been rated incorrectly by interviewers and alerted us to the need for more comprehensive training of interviewers for the large scale national mental health survey.
Participant response rate, human resource time, and prevalence. The response rate was very high (more than 99%) in this study. The average duration of the face-to-face interview for adolescents was 36 minutes (minimum 18 minutes and maximum 90 minutes; SD: 9 minutes) and 35.9 minutes for adults (minimum 15 minutes and maximum 103 minutes; SD: 12.3 minutes).
Prevalence rates for this pilot study for the most common mental disorders are reported elsewhere.16 Notably, we did not find any cases of anorexia nervosa, bulimia nervosa, and hypomanic episode in adults in the pilot study. Among adolescents, we did not find any case of manic and hypomanic episode, PTSD, alcohol use disorder, Tourette’s disorder, attention deficit hyperactivity disorder, conduct disorder, bulimia nervosa, and binge eating disorder. In the substance use disorder, most of the cases using tobacco products were identified, but there were only a few cases of misuse of other substances. These findings were discussed among the TWG members and a broader platform and necessary strategies to capture the cases and the list of disorders that should be included in the main survey were recommended.
Discussion
There are not many reports on lessons learned from pilot epidemiologic studies. Our purpose in writing this manuscript was to share the processes, the difficulties we faced, the actions taken, and the lessons we learned for larger-scale surveys.
From the outset, we focused on preparing the instruments to ensure their correct translation and implementation for the study. We believe that the iterative six-step process with checks and rechecks we applied resulted in tools that are context specific and culturally appropriate. It is likely that our introduction of bridging sentences before the start of each module contributed to the acceptability of the questions in the module and reduced nonresponse by alleviating potential anxiety about topics that are otherwise sensitive in Nepal. It was our impression that the bridging sentences made the respondents feel safe and contributed to their answering honestly. Fortunately, there was consensus among our experts and the copyright holder that such statements would not affect the content, semantic, criterion, and conceptual equivalence of the tool. Moreover, previous work has shown that cross-cultural adaptation of other mental health tools for Nepal is feasible.19,21 Earlier work by Kohrt et al22 shows that culturally appropriate studies of depression and PTSD can succeed in Nepal. Indeed, detection of depression has been done with different populations within Nepal ranging from adults to geriatric populations.21,22 Also, a previous version of MINI itself was successfully used in a population of Eastern Nepal to evaluate the prevalence of psychiatric morbidity,25 hence the cross-cultural adaptation is feasible. There have also been studies in the Nepalese context using structured interview schedules using similar translation technique to ours.26 These prior studies provide further supportive evidence that context‐specific, culturally appropriate translation in our population is feasible with good psychometric properties.
In this pilot study, we had a high response rate (99%). This response rate was higher than the response in similar studies conducted in Argentina (77%) and Australia (78%),27,28 and was comparable to that of a national study conducted in India (91%).10 The high response rate might have been a function of two decisions we made. First, we elected to mobilize FCHVs who are appointed from the local level. The FCHV program is a government initiated unique program in Nepal and FCHVs are considered as the backbone behind the success of many community-based health programs in Nepal. FCHVs are female health volunteers who are elected by the mother’s groups in each ward, the smallest local administrative body in Nepal. They have key roles in linking families and communities to the health workers and modern health facilities.29 The FCHVs were mobilized during the community mapping, household listing, and rapport building phase of data collection of this study. Second, to minimize stigma related to the term mental disorders, we used the term “survey of health problems that are related to ‘Mann,’” Nepali terms for “mind” or “feelings” instead of “mental health survey.” The high response rate we obtained indicated the willingness of people to talk about their mental health conditions in this way. Also, countries like Nepal and India share a similar culture of showing respect and hospitality to the guests/outsiders. We plan to use a similar approach for the comprehensive survey, and we hope there will again be a minimal nonresponse. For the incomplete responders, we plan to conduct a segregated analysis that will help to identify how they differ from those providing complete response.
This was a pilot study conducted prior to the final comprehensive study to work through the main problems prior to the final study. The findings of this pilot study suggested a need to conduct inter-rater reliability testing at an earlier stage in study preparation (i.e., at the pilot stage). For the comprehensive survey, we aim to focus not only on developing the interview skills of the FDCs, but also on improving their conceptual grasp and clarity in understanding the types of disorders included in the survey. To ensure and maximize the inter-rater reliability of raters in the final comprehensive survey, we plan to increase the duration of training of the FDCs in line with the training duration in previous similar surveys that ranged from 7 to 8 weeks.10 We realized that they should also be exposed to real patients with different mental disorders to increase their understanding from the real cases in the outpatient clinics and in-patient services of the psychiatric units. This will be helpful especially in the questions that need the enumerator’s clinical judgment of the case. The MINI has demonstrated acceptable levels of inter-rater reliability in almost all the epidemiological studies in which it has been used.10,12,30,31 We anticipate that with intensive training of the FDCs and other methodological rigors, the psychometric properties of the MINI are unlikely to be substantially different in our population compared with those in prior studies.
A major strength of this study is that we used an internationally validated brief structured diagnostic psychiatry interview questionnaire including 15 and 23 mental disorders for adults and adolescents, respectively. Another strength was the involvement of experts from different fields of mental health. This pilot study provided a baseline for the planning and implementation of our national mental health survey in Nepal and alerted us to areas where robust monitoring is required. This study gave a strong indication that with the newer recommendations, the mental health survey at the national level is feasible using our study tools. Our study had some limitations. Although many languages are spoken in Nepal, our instruments were translated only into the Nepali language, spoken by the majority of the population. We included only participants who had some understanding of the Nepali language. The findings from the pilot study are not generalizable outside the study areas, especially to institutional settings, e.g., to hospitalized or imprisoned populations. In addition, since stigma is associated with mental illness in Nepal, reporting bias by families affected by mental illness is possible. Another limitation is that we only included children aged 13 and above. Our findings cannot be generalized to children below age 13 years who form a major population block.
Conclusion
The pilot survey was an important first step in preparing the first national mental health survey in Nepal. It helped us identify areas for improvement in the survey instruments, data collection techniques, and other methodological aspects. The lessons we learned from this pilot study might be applicable to the planning and execution of other national level surveys.
Acknowledgments
We would like to acknowledge the input of all the members of Steering Committee and Technical Working Group for the pilot mental health survey. We would also like to acknowledge the members of the tools translation committees. This study would not be possible without the efforts of field data enumerators, and our survey participants. We are grateful to Government of Nepal and World Health Organization (WHO) Country Office for Nepal for financial support to conduct this study. We thank Dr. Kathy Sheehan for her assistance with the manuscript. We would also like to thank all the FCHVs for their valuable help during the household listing phase.
Members of steering committee: Dr. Anjani Kumar Jha, Dr. Bibek Kumar Lal, Dr. Deependra Raman Singh, Mr. Matrika Devkota, Dr. Mohan Raj Shrestha Lakhe, Dr. Pashupati Mahat, Dr. Rabi Shakya, Dr. Saroj Ojha, and Mr. Suraj Koirala.
Members of Technical Working Group: Dr. Anjani Kumar Jha, Dr. Baikuntha Subedi, Dr. Basudev Karki, Dr. Devrat Joshi, Mr. Devendra Lal Karanjit, Ms. Kabita Khati, Dr. Kedar Marahatta, Ms. Khagi Maya Pun, Dr. Meghnath Dhimal, Mr. Nagendra Luitel, Dr. Pawan Sharma, Dr. Phanindra Baral, Mr. Ramesh Prasad Adhikari, Dr. Sagun Ballav Pant, Dr. Saroj Ojha, Mr. Shiva Lal Sharma, Dr. Suraj Shakya, Ms. Sushma Dahal, Ms. Sweta Labh, and Ms. Yeshoda Aryal.
List of members in the tools translation committee: Mr. Prabhat Kiran Pradhan, Dr. Rachana Sharma, Dr. Ritesh Thapa, Ms. Sandhya Budhathoki, Dr. Suraj Shakya, Ms. Sushma Dahal, and Ms. Sweta Labh.
References
- Rathod S, Pinninti N, Irfan M, et al. Mental health service provision in low and middle income countries. Health Serv Insights. 2017;10:1178632917694350.
- Kohrt BA, Hruschka DJ, Worthman CM, et al. Political violence and mental health in Nepal: prospective study. Br J Psychiatry.
2012;201(4):268–275. - Tol WA, Kohrt BA, Jordans MJ, et al. Political violence and mental health: a multi-disciplinary review of the literature on Nepal. Soc Sci Med. 2010;70(1):35–44.
- Kane JC, Luitel NP, Jordans MJ, et al. Mental health and psychosocial problems in the aftermath of the Nepal earthquakes: findings from a representative cluster sample survey. Epidemiol Psychiatr Sci.
2018;27(3):301–310. - World Health Organization and Calouste Gulbenkian Foundation site. Social Determinants of Mental Health. 2014. https://apps.who.int/iris/bitstream/handle/10665/112828/9789241506809-chi.pdf. Accessed 9 December 2020.
- Sheehan DV. The MINI International Neuropsychiatric Interview (Version 7.0. 2) for DSM-5. Harm Research Institute; 2016.
- Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiat. 1998;59 Suppl 20:22-33;quiz 34–57.
- Government of Nepal: National Planning Commission Secretariat. Population Monograph of Nepal Volume 2. Ramshah Path, Kathmandu, Nepal: Central Bureau of Statistics; 2014:1–402.
- Nepal in figures. 2018. Central Bureau of Statistics. https://cbs.gov.np/wp-content/upLoads/2019/02/Nepal-in-Figures-2018.pdf. Accessed 17 Dec 2020.
- Murthy RS. National mental health survey of India 2015–2016. Indian J Psychiatry.
2017;59(1):21. - Government of Nepal: National Planning Commission Secretariat. National Population and Housing Census Central Bureau of Statistics. Kathmandu, Nepal: Central Bureau of Statistics; 2012.
- Sheehan DV, Sheehan KH, Shytle RD, et al. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). J Clin Psychiat. 2010;71(3):313–326.
- Suttajit S, Kittirattanapaiboon P, Junsirimongkol B, et al. Risks of major depressive disorder and anxiety disorders among Thais with alcohol use disorders and illicit drug use: findings from the 2008 Thai National Mental Health survey. Addict Behav. 2012;37(12):1395–1399.
- Kadri N, Agoub M, Assouab F, et al. Moroccan national study on prevalence of mental disorders: a community‐based epidemiological study. Acta Psychiatrica Scandinavica. 2010;121(1):71–74.
- Ghanem M, Gadallah M, Meky FA, et al. National survey of prevalence of mental disorders in Egypt: preliminary survey. E Mediterr Health J. 2009;15(1):65–75.
- Jha AK, Ojha SP, Dahal S, et al. Prevalence of mental disorders in Nepal: findings from the pilot study. J Nepal Health Res Counc. 2019;17(2):141–147.
- Clement S, Brohan E, Jeffery D, et al. Development and psychometric properties the Barriers to Access to Care Evaluation scale (BACE) related to people with mental ill health. BMC Psychiatry. 2012;12(1):36.
- Health Service and Population Research Department, Institute of Psychiatry. Barriers to Care Evaluation (BACE) Scale (v3). Strand, London WC2R 2LS, United Kingdom; King’s College London: 2011.
- Ghimire DJ, Chardoul S, Kessler RC, et al. Modifying and validating the Composite International Diagnostic Interview (CIDI) for use in Nepal. Int J Meth Psych Res. 2013;22(1):71–81.
- Brislin RW. The wording and translation of research instruments. In: Lonner WJ and Berry JW (Eds.). Cross-cultural research and ethodology series, volume eight. Field methods in cross-cultural research. Newbury Park, California; Sage Publications, In;
1986:137–164. - Kohrt BA, Luitel NP, Acharya P, et al. Detection of depression in low resource settings: validation of the Patient Health Questionnaire (PHQ-9) and cultural concepts of distress in Nepal. BMC psychiatry. 2016;16(1):58.
- Kohrt BA, Jordans MJ, Tol WA, et al. Validation of cross-cultural child mental health and psychosocial research instruments: adapting the Depression Self-Rating Scale and Child PTSD Symptom Scale in Nepal. BMC Psychiatry. 2011;11(1):127.
- Van Ommeren M, Sharma B, Thapa S, et al. Preparing instruments for transcultural research: use of the translation monitoring form with Nepali-speaking Bhutanese refugees. Transcult Psychiatry. 1999;36(3):285–301.
- Thapa N, Aryal KK, Paudel M, et al. Nepalese homebrewed alcoholic beverages: Types, ingredients, and ethanol concentration from a nation wide survey. J Nepal Health Res Counc. 2015;13(29):59–65.
- Shyangwa PM, Shakya DR, Adhikari BR, et al. Community based survey on psychiatric morbidity in eastern Nepal. J Nepal Med Assoc. 2014;52(196):997–1004.
- Van Ommeren M, de Jong JT, Sharma B, et al. Psychiatric disorders among tortured Bhutanese refugees in Nepal. Arch Gen Psychiatry. 2001;58(5):475–482.
- Stagnaro JC, Cía AH, Gaxiola SA, et al. Twelve-month prevalence rates of mental disorders and service use in the Argentinean Study of Mental Health Epidemiology. Soc Psychiatry Psychiatr Epidemiol. 2018;53(2):121–129.
- Andrews G, Henderson S, Hall W. Prevalence, comorbidity, disability and service utilisation: overview of the Australian National Mental Health Survey. Br J Psychiatry. 2001;178(2):145–153.
- Khatri RB, Mishra SR, Khanal V. Female community health volunteers in community-based health programs of Nepal: future perspective. Front Public Health.
2017;5:181. - Sheehan D, Lecrubier Y, Sheehan KH, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiat. 1997;12(5):232–241.
- Kadri N, Agoub M, El Gnaoui S, et al. Moroccan colloquial Arabic version of the Mini International Neuropsychiatric Interview (MINI): qualitative and quantitative validation. Eur Psychiat. 2005;20(2):193–195.





