by Randy A. Sansone, MD, and Lori A. Sansone, MD
by Randy A. Sansone, MD, and Lori A. Sansone, MD
R. Sansone is a professor in the Departments of Psychiatry and Internal Medicine at Wright State University School of Medicine in Dayton, OH, and Director of Psychiatry Education at Kettering Medical Center in Kettering, OH. L. Sansone is a civilian family medicine physician and Medical Director of the Family Health Clinic at Wright-Patterson Air Force Base Medical Center in WPAFB, OH. The views and opinions expressed in this article are those of the authors and do not reflect the official policy or position of the United States Air Force, Department of Defense, or United States Government.
Innov Clin Neurosci. 2014;11(11–12):36–40
This ongoing column is dedicated to the challenging clinical interface between psychiatry and
primary care—two fields that are inexorably linked.
Funding: There was no funding for the development and writing of this article.
Financial disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Aggression, healthcare, patient aggression, patient violence, physicians, violence
Abstract: Over the past 20 or so years, a number of studies have examined patient aggression toward healthcare professionals. While the majority of these studies has focused on healthcare professionals in the fields of emergency medicine, psychiatry, and primary care, available data extends beyond these three specialties. Studies have been done in the United States, other English-speaking countries, and elsewhere—all reporting surprisingly high rates of patient aggression. Results indicate that patient aggression toward healthcare professionals is common and worldwide. In addition, one study examined aggressive patient behaviors as reported by the patients themselves, and their self-report data reinforce the mainstream data. While these data do not enable us to determine if patient aggression is genuinely on the increase, we can safely say that these behaviors are rampant.
Introduction
Aggression is unfortunately ever-present in our world. And, it seems to be spreading into the sanctum of the medical practitioner, whether in the psychiatry setting or primary care setting. While patient aggression in the clinical setting has been well-known for years, cumulative studies are beginning to elucidate its extent. Indeed, even the media are now actively acknowledging patient violence against healthcare professionals. For example, in a 2010 blog by the Skeptical Scalpel, there is an article entitled, “World-Wide Violence Against Doctors and Nurses.”[1] In this edition of The Interface, we present a number of articles on the prevalence of patient aggression in various medical settings based upon the accounts of trainees, physicians-in-practice, and even the patients themselves. From these data, one conclusion is evident— aggressive patient behaviors in the medical setting are fairly rampant, regardless of practice type, patient sample, or geographic location. We will first examine aggressive patient behaviors toward trainees.
Medical Trainees at Risk
According to empirical studies, patient mistreatment of resident physicians is surprisingly common. For example, among trainees in seven Canadian residencies, Cook et al[2] found that 50 percent of participants reported psychological abuse by patients, with 10 to 15 percent reporting physical assaults by either patients or family members. Coverdale et al[3] surveyed 135 New Zealand residents in the fields of psychiatry, general medicine, surgery, and obstetrics/gynecology. In this study, 67 percent of participants reported verbal threats by patients, 54 percent physical intimidation, 41 percent the observation of damage to the treatment facility, and 39 percent physical assaults. We surveyed training directors of psychiatry programs and found a mean of 1.26 physical attacks on residents per program during a two-year study period.[4] Finally, in a study of psychiatric trainees in Belgium, Pieters et al[5] found that 72 percent of respondents reported verbal threats by patients and 56 percent had experienced at least one physical assault by a patient.
Physicians at Risk
In addition to trainees, physicians in practice are at risk for patient aggression. In this regard, several studies from the United States have documented patient violence toward physicians who are established in practice. For example, in a survey of emergency physician members of the Michigan College of Emergency Physicians, Kowalenko et al[6] reported on the results of 171 respondents. In this study, during the previous 12 months, 74.9 percent reported at least one verbal threat by a patient and 28.1 percent reported a physical assault by a patient. In a study of 65 emergency departments across the United States, Kansagra et al[7] examined the responses of 3,518 participants. In this study, respondents indicated a median of 11 patient attacks per site over a five-year period. In a survey of 91 psychiatrists, Dubin et al[8] found that approximately one-third of respondents reported serious assaults by patients. Finally, Madden et al[9] surveyed 115 psychiatrists and found that 41.7 percent reported physical assaults by patients.
Patient abuse of physicians is also reported in other English-speaking countries. For example, in a study from the United Kingdom, Hobbs10 examined aggressive patient incidents experienced by general practitioners.[1] In this sample of 1,093 physicians, 62.9 percent reported abuse or violence during the preceding 12 months. While the majority of incidents involved verbal abuse or threats (91.3% of all incidents), there were 90 incidents of frank physical assault or injury of physicians. Cook et al[11] surveyed 501 Canadian general internists and found that three quarters had experienced emotional abuse by patients, with 38 percent of female and 26 percent of male respondents reporting physical assaults. Among 196 Canadian female physicians, Stewart et al[12] found that during the year preceding the study, 71 percent had experienced verbal abuse and 33 percent physical assault by patients. In an Australian sample of general practitioners, Tolhurst et al[13] found that 73 percent of surveyed participants reported some form of violent or aggressive behavior from patients. Finally, in another study of Australian general practitioners, Koritsas et al[14] examined physician gender and relationships to patient abuse. In this study, 49 percent of women and 41 percent of men reported verbal abuse; 24 percent of women and 22 percent of men reported property damage or theft by patients; three percent of women and four percent of men reported physical abuse; and no women and two percent of men reported sexual assault by patients.
Unfortunately, the preceding statistics are echoed in non-English-speaking countries, as well. For example, in a study from Kuwait, Al-Sahlawi et al[15] examined 101 emergency medicine physicians and found that 86 percent had experienced either verbal insults or intimidation, 28 percent physical assaults, and seven percent serious injury. In a Turkish study of 195 emergency medicine physicians, Ayranci[16] found that 72.3 percent reported some form of violence: 69.5 percent emotional or verbal abuse and 8.5 percent physical assault. In an Israeli study comparing community and hospital physicians, Carmi-lluz et al[17] surveyed 177 practitioners. Verbal abuse was reported by 53.7 percent of hospital physicians and 58.5 percent of community physicians whereas physical violence was experienced by 9.5 percent of hospital physicians and 8.5 percent of community physicians. In a study from Japan, Arimatsu et al[18] studied 698 physicians from various specialties and reported that 24.1 percent had experienced verbal abuse and 2.1 percent physical violence in the past six months. In a second study from Turkey, Aydin et al[19] examined 522 general practitioners and found that 82.8 percent reported violence, mostly verbal abuse. In a second study from Japan, Saeki et al[20] examined 758 physicians from various specialties and found that 26 (3.4%) had experienced posttraumatic stress disorder (PTSD)-symptoms in the aftermath of patient aggression. In a study from Poland, Kowalczuk et al[21] surveyed 501 physicians and reported that 86 percent had experienced patient aggression. Finally, Algwaiz and Alghanim22 surveyed 600 physicians and nurses in Saudi hospitals and found that 67.4 percent had been victims of patient violence in the preceding 12 months.
In summarizing these studies, it is evident that participants are reporting surprisingly high rates of maltreatment by patients. This finding is evident regardless of study methodology, sample type, or country in which the investigation took place. Clearly, patient aggression toward trainees and physicians in practice is despairingly common. One limitation of the majority of the previous studies is the lack of explicit clarification of the nature of physician maltreatment by patients.
A Physician Survey exploring Explicit Aggressive Patient Behaviors
In an effort to further examine the types of aggressive patient behaviors experienced by physicians, we undertook a cross-sectional survey of 61 primary care physicians.[23] In this survey, we asked if participants had experienced any of 26 aggressive patient behaviors during the preceding 12 months (Table 1). Note that, as in previous studies, various forms of verbal abuse were quite common. Unlike previous reports, no participant reported a physical assault. However, 41 percent of participants reported calling the police or security to have a patient removed from their office.
We also asked respondents if their practice styles had been affected by patient aggression during the previous 12 months. In this sample, 8.2 percent endorsed this item and offered the following comments: “increased background checks on suspicious or abusive patients and increased numbers of policies/procedures to deal with inappropriate behavior;” “I am drafting a letter to patients explaining our policies/procedures and expectations of their behavior;” “cautious, thorough documentation of boundaries;” “more setting limits with patients, and not allowing patients between me and the door;” and, “we lock the door between the waiting room and our back office to limit access to all but scheduled patients.”
We also included a screen for PTSD. In examining these data, 4.9 percent of respondents indicated having had nightmares about a patient incident, 9.8 percent reported trying to avoid thinking about an incident, and 4.9 percent acknowledged being constantly on guard, watchful, or easily startled as a result of an incident. None of the respondents reported feeling numb or detached or missing work as a result of patient bullying or harassment. Only one respondent (1.6%) endorsed the necessary three items for a diagnosis of PTSD.
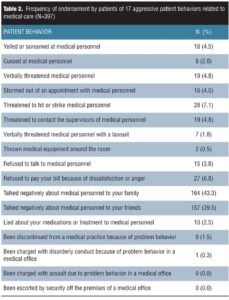
Patient Disclosures of Their Aggressive Behavior
While there are numerous physician reports of aggressive patient behaviors in the empirical literature, there is little documentation from the patients themselves. To address this gap, in a cross-sectional study of 397 internal medicine outpatients, we explored the lifetime prevalence of 17 aggressive patient behaviors according to self-report data from the patients, themselves (Table 2).[24] In this study, the most frequently endorsed aggressive patient behaviors were talking negatively to friends and family about providers. However, 7.1 percent of the sample reported that they had threatened to hit or strike medical personnel and 1.5 percent admitted to being discontinued from a previous medical practice due to problem behavior.
Conclusion
These data clearly affirm that over the past 20 or so years, patients have demonstrated a number of aggressive behaviors toward trainees and physicians-in-practice. From the available studies, it is difficult to discern if these behaviors are genuinely occurring more frequently (i.e., it is difficult to compare various samples and variables at two points in time), although a number of authors believe so. In addition to reports by trainees and physicians in practice, the patients themselves are reporting aggressive behaviors toward healthcare professionals. In the extant literature, the explanations for the prevalence of aggressive patient behaviors vary, but one thing seems clearly evident—these behaviors are not diminishing in the clinical setting.
References
1. Skeptical scalpel. Aug 15, 2010. World-wide violence against doctors and nurses. http://skepticalscalpel.blogspot.com/2010/08/world-wide-violence-against-doctors-and.html. Accessed on March 14, 2012.
2. Cook DJ, Liutkus JF, Risdon CL, et al. Residents’ experiences of abuse, discrimination and sexual harassment during residency training. McMaster University Residency Training Programs. CMAJ. 1996;154:1657–1665.
3. Coverdale J, Gale C, Weeks S, et al. A survey of threats and violent acts by patients against training physicians. Med Educ. 2001;35:154–159.
4. Sansone RA, Taylor SB, Gaither GA. Patient assaults on psychiatry residents: results of a national survey. Traumatol. 2002;8:211–214.
5. Pieters G, Speybrouck E, de Gucht V, Joos S. Assaults by patients on psychiatric trainees: frequency and training issues. Psychiatr Bull. 2005;29:168–170.
6. Kowalenko T, Walters BL, Khare RK, Compton S. Workplace violence: a survey of emergency physicians in the state of Michigan. Ann Emerg Med. 2005;46:142–147.
7. Kansagra SM, Rao SR, Sullivan AF, et al. A survey of workplace violence across 65 U.S. emergency departments. Acad Emerg Med. 2008;15:1268–1274.
8. Dubin WR, Wilson SJ, Mercer C. Assaults against psychiatrists in outpatient settings. J Clin Psychiatry. 1988;49:338–345.
9. Madden DJ, Lion JR, Penna MW. Assaults on psychiatrists by patients. Am J Psychiatry. 1976;133:422–425.
10. Hobbs FD. Violence in general practice: a survey of general practitioners’ views. BMJ. 1991;302:329-332.
11. Cook DJ, Griffith LE, Cohen M, et al. Discrimination and abuse experienced by general internists in Canada. J Gen Intern Med. 1995;10:565–572.
12. Stewart DE, Ahmad F, Cheung AM, et al. Women physicians and stress. J Womens Health Gend Based Med. 2000;9:185–190.
13. Tolhurst H, Baker L, Murray G, et al. Rural general practitioner experience of work-related violence in Australia. Aust J Rural Health. 2003;11:231–236.
14. Koritsas S, Coles J, Boyle M, Stanley J. Prevalence and predictors of occupational violence and aggression towards GPs: a cross-sectional study. Br J Gen Pract. 2007;57:967–970.
15. Al-Sahlawi KS, Zahid MA, Shahid AA, Hatim M, Al-Bader M. Violence against doctors: 1. A study of violence against doctors in accident and emergency departments. Eur J Emerg Med. 1999;6:301–304.
16. Ayranci U. Violence toward health care workers in emergency departments in west Turkey. J Emerg Med. 2005;28:361–365.
17. Carmi-lluz T, Peleg R, Freud T, Shvartzman P. Verbal and physical violence towards hospital- and community-based physicians in Negev: an observational study. BMC Health Serv Res. 2005;5:54.
18. Arimatsu M, Wada K, Yoshikawa T, et al. An epidemiological study of work-related violence experienced by physicians who graduated from a medical school in Japan. J Occup Health. 2008;50:357–361.
19. Aydin B, Kartal M, Midik O, Buyukakkus A. Violence against general practitioners in Turkey. J Interpers Violence. 2009;24:1980–1995.
20. Saeki K, Okamoto N, Tomioka K, et al. Work-related aggression and violence committed by patients and its psychological influence on doctors. J Occup Health. 2011;53:356–364.
21. Kowalczuk K, Jankowiak B, Krajewska-Kulak E, Van Damme-Ostapowicz K, Kowalewska B. Comparison of the level of aggression towards healthcare workers within Podlaskie Voivodeship. Int J Occup Med Environ Health. 2011;24:267–274.
22. Algwaiz WM, Alghanim SA. Violence exposure among health care professionals in Saudi hospitals. A preliminary investigation. Saudi Med J. 2012;33:76–82.
23. Sansone RA, Sansone LA, Wiederman MW. Patient bullying: a survey of physicians in
primary care. Prim Care Companion. 2007;9:56–58.
24. Sansone RA, Farukhi S, Wiederman MW. Aggressive patient behaviors related to medical care: a self-report survey. Prim Care Companion CNS Disord. 2011;13(4). pii: PCC.11m01160.