by Takashi Ohnishi, MD, PhD; Hisanori Kobayashi, PhD; Tsutomu Yajima, MS; Takeshi Koyama, MS; and Kenichi Noguchi, PhD
Drs. Ohnishi, Kobayashi, and Noguchi are with the Medical Affairs Division, Mr. Yajima is with the Quantitative Science Division, and Mr. Koyama is with the Drug Surveillance Department of the Research and Development Division of Janssen Pharmaceutical K.K. in Tokyo, Japan.
Funding: Support for this study was provided by Janssen Pharmaceutical K.K.
Disclosures: All authors are full-time employees of Janssen Pharmaceutical K.K., which is a division of Johnson & Johnson Japan.
Abstract: Objective: While attention-deficit/hyperactivity disorder (ADHD) is associated with a high prevalence of comorbid psychiatric disorders in every age group, the etiology and epidemiology of comorbid disorders are less clear in adult patients with ADHD. In this surveillance study, investigators sought to assess the prevalence of comorbid psychiatric disorders, evaluate relationships between comorbid psychiatric disorders and demographic characteristics, and explore the patterns of these comorbid disorders and their relationships with ADHD subtypes. Methods: Data obtained from postmarketing surveillance of methylphenidate extended-release tablets for adult ADHD were used to evaluate the prevalence of psychiatric comorbidities. Age, sex, age at diagnosis, number of comorbidities, and severity of ADHD symptoms were used as external variables for exploratory analyses. Nonmetric multidimensional scaling (NMDS) was performed to explore correlations among comorbidities and ADHD subtypes and extract major dimensions underlying variations in the pattern of comorbid disorders. Results: Data were collected from 575 patients with adult ADHD, including 301 (52.35%) with at least one concurrent psychiatric disorder. Analysis by NMDS demonstrated that different patterns of psychiatric comorbidities were related to the subtypes of ADHD. Conclusions: Psychiatric comorbidities have a high prevalence in patients with adult ADHD. Understanding these patterns could provide useful information in the diagnosis of adult ADHD and future investigations of its etiology.
Keywords: Adult attention-deficit/hyperactivity disorder, comorbid disorders, externalizing disorder, internalizing disorder, nosology
Innov Clin Neurosci. 2019;16(9–10):11–16
Attention-deficit/hyperactivity disorder (ADHD) is a childhood-onset neuropsychiatric disorder characterized by developmentally inappropriate inattentiveness, increased impulsivity, and hyperactivity. Although ADHD is well-recognized in the pediatric population, a recent World Health Organization (WHO) universal mental health survey revealed that the average prevalence of adult ADHD was 2.8 percent across surveys.1 This indicates that adult ADHD is also a common psychiatric disorder around the world. While focus has been shifting toward adults with ADHD, fewer than 20 percent of adult patients with ADHD are currently diagnosed and/or being treated for this disorder.2,3 There are several reasons for this underdiagnosis and/or undertreatment of adult ADHD. In the past, inattention, impulsiveness, restlessness, and emotional dysregulation in adults were considered to be secondary to other psychiatric disorders rather than being symptoms of ADHD. Clinical research has shown that the predominant features of adult ADHD are different from those of typical pediatric ADHD and are often more heterogeneous.4 For example, hyperactivity tends to decrease with age, making it more difficult to diagnose adult ADHD.4 Also, adults with ADHD often have psychiatric comorbidities, such as mood disorders, substance use disorder, anxiety disorders, and/or conduct/behavioral disorders. Symptoms directly attributable to adult ADHD are often mistakenly considered to be symptoms of these psychiatric comorbidities, complicating the diagnosis of ADHD. Accordingly, understanding the profile of psychiatric comorbidities associated with adult ADHD is essential for an accurate diagnosis. It is also important for the management of adult ADHD, because the existence of other concurrent psychiatric disorders leads to more severe impairment, resistance to treatment, and worse outcomes.5,6 Moreover, guidelines recommend that, when ADHD coexists with other psychiatric comorbidities in adults, the most severe condition should be treated first.7
There have been several reports of a high prevalence rate of psychiatric comorbidities in adult patients with ADHD. In a United States (US) survey, 47.1 percent of respondents with ADHD also had an anxiety disorder, 38.3 percent had a mood disorder, and 15.2 percent had a substance use disorder.1 In a Canadian study, 71.9 percent of adults with ADHD had a comorbid Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition—Text Revision (DSM-IV-TR) Axis I disorder (usually anxiety and/or mood disorders) and 50.9 percent had a comorbid DSM-IV-TR Axis II disorder.8 Importantly, patients with ADHD often have multiple concurrent psychiatric disorders that make their clinical presentation more complicated, and understanding the patterns of these comorbid disorders could be important for both diagnosis and management. However, little is known about the patterns of psychiatric comorbidities in ADHD, particularly in adult patients.9,10
We conducted postmarketing surveillance of an osmotic-release oral system (OROS) with methylphenidate (MPH) application in adult patients with ADHD. Using baseline demographic data of 575 adult patients with ADHD receiving treatment with OROS-MPH, we sought to clarify the prevalence of various psychiatric comorbidities, the relationship between demographic variables (e.g., age, sex, age at diagnosis, severity of ADHD) and psychiatric comorbidities, and the patterns of psychiatric comorbidities in adult ADHD.
Methods
Study design. This was a one-year multicenter surveillance study of OROS-MPH therapy for adult ADHD. Patients 18 years of age or older who had recently commenced treatment with OROS-MPH for adult ADHD were the surveillance targets. Patients who had commenced OROS-MPH treatment during childhood were not included in this investigation. A diagnosis of adult ADHD was made according to the Japanese version of Conners’ Adult ADHD Diagnostic Interview for DSM-IV.11
We collected the following information for each patient: age, sex, age at the time of diagnosis of ADHD, severity of ADHD as estimated using the Conners’ Adult ADHD Rating Scales (CAARS) score at the time of entry into the study, and number of psychiatric comorbidities.
To assess psychiatric comorbidities, the attending physicians were asked about the presence or absence of the following 15 disorders: developmental disability, depressive disorder, dysthymia, bipolar disorder, generalized anxiety disorder (GAD), social phobia, impulse control disorder, panic disorder, learning disorder, obsessive-compulsive disorder (OCD), abuse (alcohol and/or substance), mental retardation, conduct disorder, oppositional defiant disorder (ODD), and posttraumatic stress disorder (PTSD). The diagnosis of these comorbidities was based on each physician’s clinical judgment.
An electronic data capture system was employed, and most data were transcribed from source documents into an electronic case report form by physicians and then transmitted securely to the sponsor. The protocol of this study was assessed by an internal review board of the sponsor (Research Concept Review Board of Janssen Pharmaceutical), including ethical aspects, and was also approved by the Pharmaceuticals and Medical Devices Agency (PMDA). Performing this postmarketing surveillance was part of the mandatory requirements determined and reviewed by the PMDA. The study was conducted in accordance with the relevant Japanese regulations for Good Postmarketing Study Practice (Ministry of Health, Labor, and Welfare Ministerial Ordinance no. 171). Each study site (hospital or clinic) followed its own regulations or standards for obtaining institutional review board approval, including informed consent from the participants, as is usual for this type of study in Japan. This study was registered with the UMIN Clinical Trials Registry (registration no. UMIN000015900).
Statistical analysis. Nonmetric multidimensional scaling (NMDS) was employed to explore correlations among disorders and to extract the major dimensions underlying variations in the pattern of concurrent disorders. A data matrix was created that summarized the presence/absence (1/0) of comorbidities and the subtypes of ADHD. The role of the external explanatory variables (i.e., age, sex, age at diagnosis of ADHD, number of psychiatric comorbidities, and severity of ADHD as estimated by CAARS score) was further explored by using a vector-fitting procedure to identify the direction of maximal correlation with these variables in the NMDS space.12
A two-sided p-value of less than 0.05 was defined as indicating statistical significance. Statistical analyses were conducted using the R Statistical software program, version 3.1.0 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Demographic characteristics. Table 1 lists the demographic characteristics of the subjects. A total of 575 adults with ADHD (298 men and 277 women with a mean age of 33.07 years) were enrolled in the survey. The group included 336 patients (58.43%) with the inattentive type of ADHD, 40 patients (6.96%) with the hyperactive–impulsive type, and 199 patients (34.61%) with the combined type.
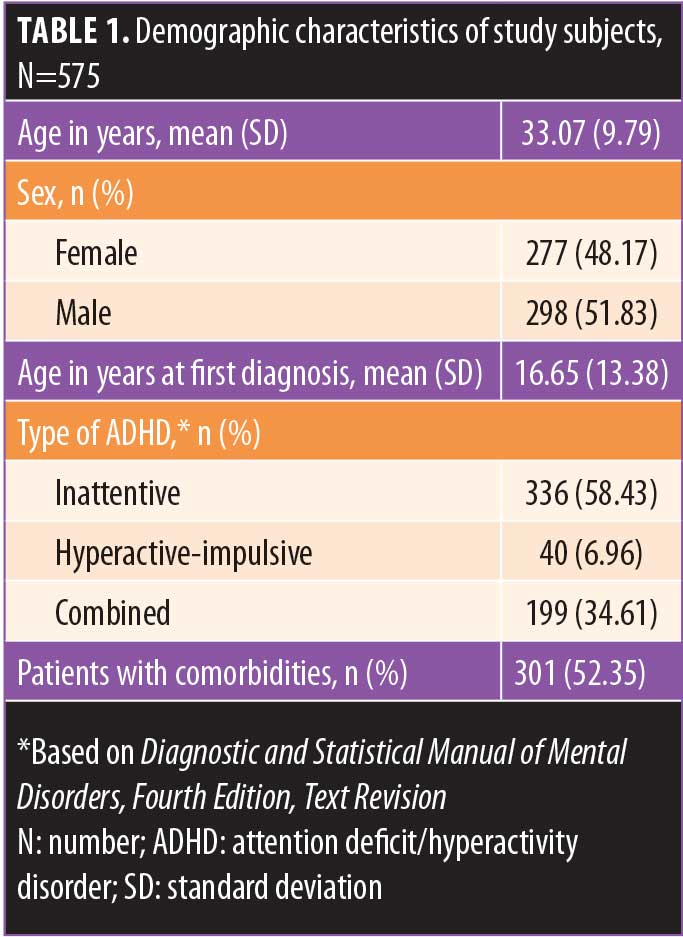
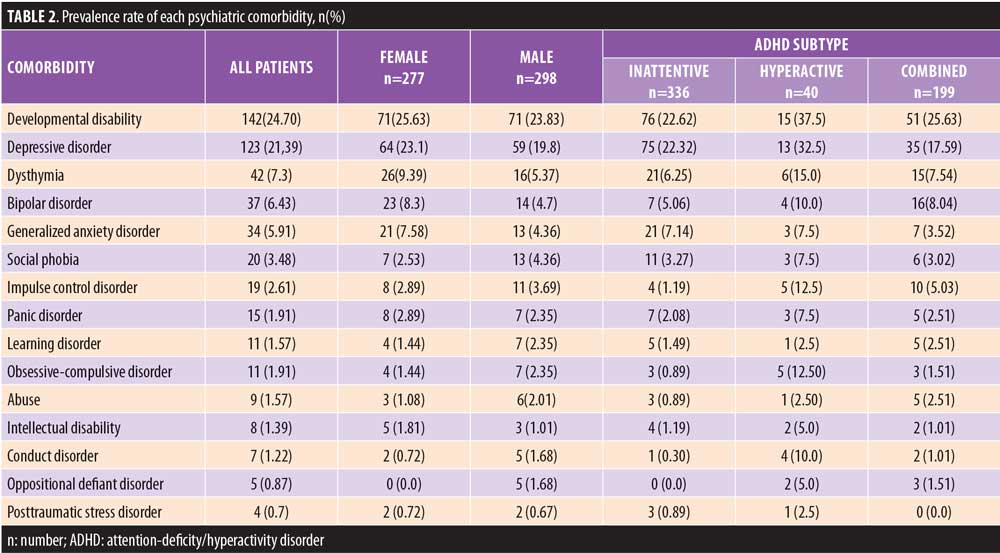
Prevalence of psychiatric comorbidities. Among the 575 patients, 301 (52.35%) had at least one concurrent psychiatric disorder. Table 2 shows the prevalence rate of each disorder. Frequently observed comorbid disorders included developmental disability (24.70%) and depressive disorder (21.39%); other disorders had prevalence rates of less than 10 percent, with exception of anxiety disorders, which had an overall prevalence (sum of GAD, social phobia, panic disorder, OCD, and PTSD) of 12.17 percent (n=70 patients).
One psychiatric comorbidity was present in 32.87 percent of the patients, two comorbidities were present in 12.7 percent, three comorbidities in 3.83 percent, and four or more comorbidities were present in 2.96 percent of the patients.
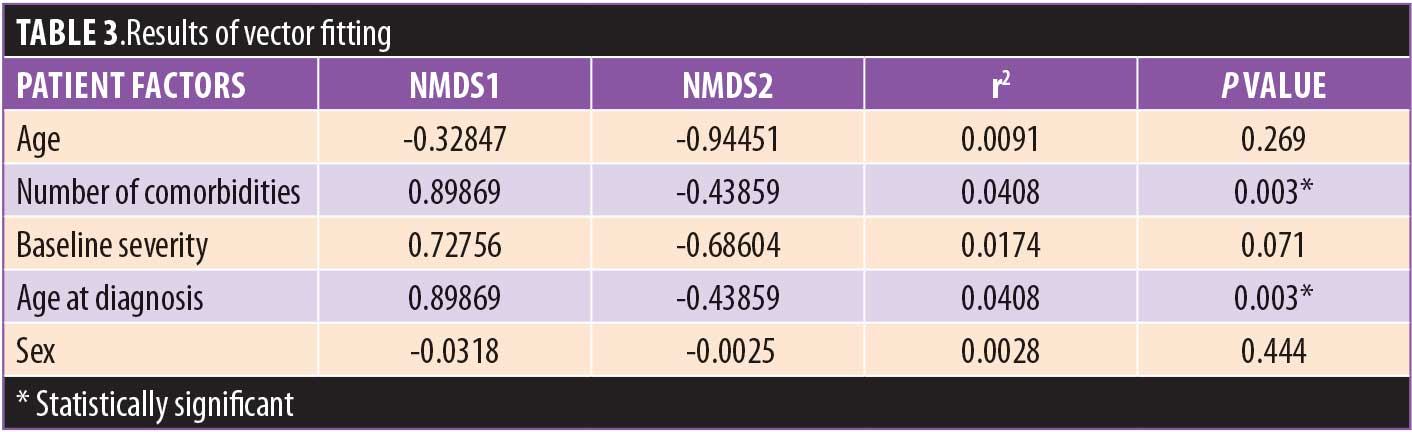
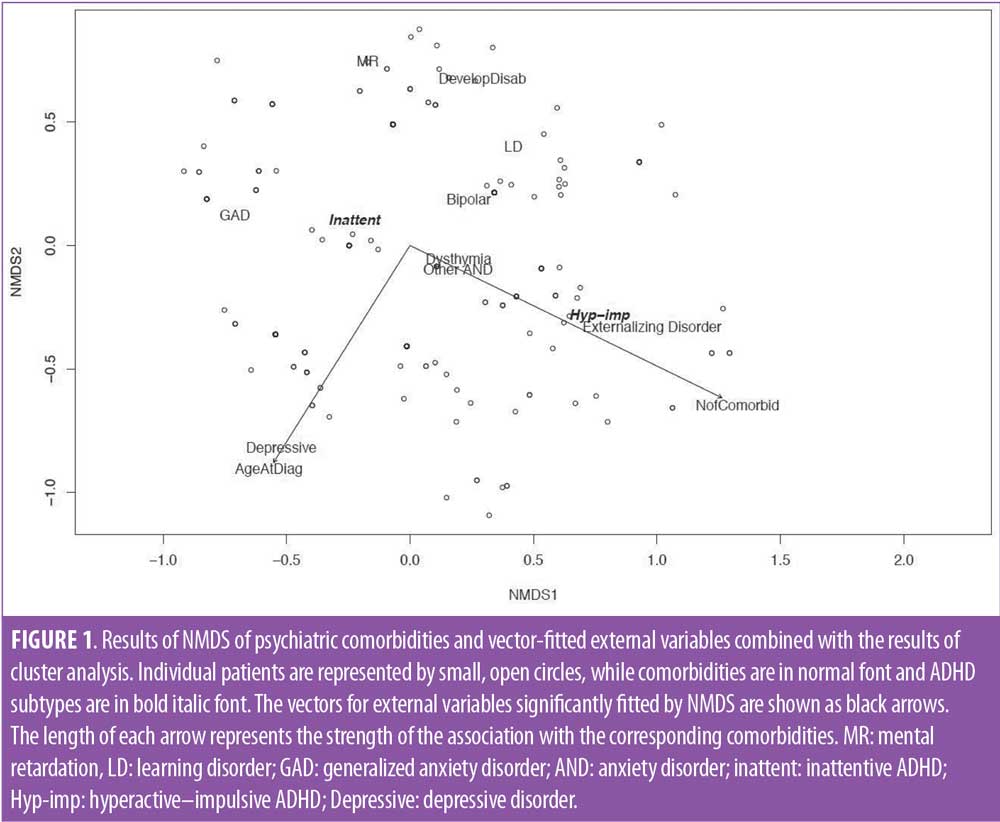
Patterns of psychiatric comorbidities and relationships between psychiatric comorbidities and demographic characteristics. First, NMDS was performed with the 15 categories of concurrent psychiatric disorders and three subtypes of ADHD. However, this model did not achieve convergence due to small sample sizes in some categories (data not shown). Therefore, we combined the various categories as follows: 1) we created a category of externalizing disorders that included impulse control disorder, ODD, CD, and abuse; (2) excluding GAD, we combined the other anxiety disorders (e.g., social phobia, panic disorder, OCD, and PTSD), which were all found in small numbers of patients; and 3) we dichotomized ADHD subtypes based on the presence of inattention and/or hyperactive–impulsive symptoms. Figure 1 displays the results obtained by NMDS using these categorized psychiatric comorbidities, ADHD subtypes, and vector-fitted external variables. Individual patients are represented by small open circles. Comorbidities and ADHD subtypes plotted close together in the figure are correlated with each other. As shown in Table 3, vector fitting revealed that the number of psychiatric comorbidities and the age at diagnosis of ADHD were significantly associated with the corresponding comorbidities. The vectors for these external variables that were significantly fitted by NMDS are shown as arrows in Figure 1, with the length of the arrow representing the strength of the association with the corresponding comorbidities. NMDS generated two dimensions that appeared to fit the data well, and these two dimensions explained a large proportion of the variance (stress=0.1786). The first dimension provided differentiation between depressive disorder/GAD and inattentive ADHD versus externalizing disorders and hyperactive–impulsive ADHD. The second dimension showed marked differentiation between depressive disorder versus mental retardation, developmental disability, and learning disorder. Mental retardation, learning disorder, and developmental disability were located close together in both dimensions. In addition, a cluster was formed by dysthymia, anxiety disorders including GAD, bipolar disorder, and inattentive ADHD. On the other hand, externalizing disorders and hyperactive–impulsive ADHD were located close together. Among the comorbidities, bipolar disorder, dysthymia, and other anxiety disorders formed a cluster, while other anxiety disorders and externalizing disorders were relatively close together. Vector fitting revealed an association between a larger number of psychiatric comorbidities and externalizing disorders (Figure 1, arrow), while an older age at the time of diagnosis of ADHD was associated with depressive disorder (Figure 1, arrow). However, these two external variables accounted for a low proportion of the variance (r2 < 0.25) (Table 3).
Discussion
In this study, we found that more than 50 percent of adult patients with ADHD had at least one comorbid psychiatric condition, and of those, nearly 40 percent had multiple comorbidities. Frequent concurrent psychiatric conditions included developmental disability, depressive disorder, and anxiety disorders. The NMDS clearly demonstrated the patterns of psychiatric comorbidities and relationships between ADHD subtypes and psychiatric comorbidities. For example, closeness among dysthymia, anxiety disorders, and the inattentive type of ADHD indicated that these disorders are likely to occur in patients with inattentive ADHD, while closeness between externalizing disorders and the hyperactive–impulsive type of ADHD suggest a strong relationship between these two disorders. On the other hand, there was a large distance between depressive disorder and other comorbidities, which suggests that depressive disorder tends to occur without other comorbidities in adult patients with ADHD.
Prevalence rate of each psychiatric comorbidity. Depressive disorders. ADHD and depression often occur together, and the prevalence rate of depression in patients with adult ADHD has been reported ranging from 18.6 to 53.3 percent.1,17 In agreement with the results of previous studies, we also found a high prevalence (28.49%) of depressive disorder and dysthymia associated with adult ADHD in our patient sample.
Autistic spectrum disorder. Although the diagnosis of ADHD was based on Conners’ Adult ADHD diagnostic interview for DSM-IV that specifies a diagnosis of autistic spectrum disorder (ASD) as excluding ADHD, the most frequent psychiatric comorbidity in our study was developmental disability (mainly ASD). While DSM-IV-TR does not allow for a dual diagnosis of ADHD and ASD, several studies have identified frequent co-occurrence of these two disorders.18,19 Previous investigations of children and adolescents have found that 30 to 50 percent of patients with ASD also exhibit prominent ADHD symptoms.20,21 In addition, other researchers report that more than 60 percent of individuals with ADHD also showed features of ASD.22 The high prevalence rate of developmental disability in our study suggests that not only children but also adults with ADHD frequently have ASD as a comorbidity. Indeed, a longitudinal investigation of the relationship between ASD and ADHD revealed that the trajectories of both conditions were strongly interlinked,23 and most children with persistent hyperactive-inattentive symptoms also showed persistent social commutation deficits.23 These data seem to support a high prevalence rate of concurrent ADHD and ASD in adults. Since the DSM-5 allows for the dual diagnosis of ASD and ADHD, future research will be able to clarify the precise prevalence rate of ASD in adults with ADHD.
Anxiety disorders. Anxiety disorders are well-known psychiatric comorbidities in adult patients with ADHD. In our study, the prevalence rate for all anxiety disorders combined (i.e., GAD, social phobia, panic disorder, OCD, and PTSD) was 12.17 percent. According to a previous survey, 23 percent of adult patients with ADHD had concurrent anxiety disorders and 16.7 percent had a history of anxiety disorders.8 Other studies have also shown a higher risk of anxiety disorders in individuals with ADHD, compared to the general population,1,24,25 and our results support a high prevalence of anxiety disorders in adults with ADHD.
Externalizing disorders. Impulse control disorder, conduct disorder (CD), and oppositional defiant disorder (ODD) are well-known comorbid externalizing disorders in children and adolescents with ADHD, while substance use disorder is a typical comorbid externalizing disorder in adult ADHD. In this study, the prevalence rate of these externalizing disorders, including substance use disorder, was 5.56 percent (n=32). Previous studies of children and adolescents have found that 30 to 50 percent of these patients who meet the criteria for ADHD also fulfill the criteria for CD or ODD.26–28 Also, a longitudinal study demonstrated a correlation between ADHD-like symptoms and externalizing traits that became stronger over time.28 Thus, the prevalence rate of externalizing disorders in our study seems to be low. A possible explanation for this finding is the influence of selection bias (see the Limitations section at the end of the Discussion). The prevalence rate of substance use disorder was only 1.56 percent in our study. Another study found that concurrent conduct disorder was a powerful predictor of the subsequent onset of substance use disorder.29 Taken together, the low prevalence rate of externalizing disorders in our study was probably associated with selection bias.
Patterns of psychiatric comorbidities and relationship with demographic characteristics. The analysis by NMDS clearly demonstrated different patterns of psychiatric comorbidities in relation to the subtype of ADHD. As already mentioned, the closeness between intellectual disability and developmental disability indicates that these two disorders are likely to occur together, while the large distance between depressive disorder and the other comorbidities suggests that depressive disorder tends to occur in isolation. In addition, the closeness between dysthymia, anxiety disorders (e.g., GAD), bipolar disorder, and the inattentive type of ADHD suggests that these comorbidities are likely to occur together in patients with inattentive ADHD. On the other hand, externalizing disorders are likely to occur in patients with the hyperactive–impulsive type of ADHD. The relative closeness between externalizing disorders, dysthymia, and anxiety disorders (except GAD) suggests a pattern of concurrent externalizing and internalizing disorders in adult ADHD. In contrast with these disorders, depressive disorder tended to occur independently of other comorbidities in our patient sample. Although patients with adult ADHD often have multiple psychiatric comorbidities that contribute to challenges in its diagnosis and management, the patterns of concurrent disorders are not well known. While a few studies were conducted to clarify comorbidity patterns in children and adolescents with ADHD,9,10 our literature search did not identify any previous reports regarding the patterns of psychiatric comorbidities in adult ADHD. A previous study of comorbidity patterns in children and adolescents with ADHD revealed that 33.3 percent had one additional disorder, 18.7 percent had two additional disorders, 8.2 percent had three additional disorders, 2.9 percent had four additional disorders, and 0.6 percent had five additional disorders.10 The same study also reported that anxiety disorders, ODD, and minor depression/dysthymia were frequently combined in children and adolescents with ADHD and multiple comorbidities,10 suggesting that these patients are likely to have both externalizing and internalizing disorders. Although the prevalence rates of multiple comorbidities were lower our study than in the previous study of children and adolescents with ADHD,10 we also found a combination of both externalizing and internalizing disorders in our adult patients with ADHD.
Previous studies of psychiatric comorbidities in ADHD have also investigated the relationship between comorbid disorders and demographic variables such as sex and ADHD subtype.10,30 In children and adolescents, Elia et al10 reported that ODD was more prevalent in the combined and hyperactive types of ADHD compared to the inattentive type. In a longitudinal study investigating sex differences of comorbid disorders in adult ADHD, researchers observed that externalizing disorders were more common in men and internalizing disorders were more common in women.30 Unlike other studies, we employed multivariate analyses rather than stratified analyses to investigate the relationship between comorbidity patterns and demographic variables, including the subtype of ADHD. We found that externalizing disorders were associated with hyperactive–impulsive ADHD, in agreement with a previous report.10 However, the association between sex and prevalence of comorbid internalizing/externalizing disorders, did not reach statistical significance in our study. We did find that having a larger number of comorbidities was associated with externalizing disorders in adult patients with ADHD, and that older age at the time of diagnosis of ADHD was associated with depressive disorder. Although these associations were statistically significant, these factors accounted for a low proportion of the variance. Therefore, our results should be interpreted with caution and we cannot offer any explanation for these associations at present.
Why is ADHD so often associated with psychiatric comorbidities? It has long been recognized that psychiatric disorders tend to run in families, suggesting a genetic influence. ADHD and some of the comorbidities identified in our study, such as ASD and bipolar disorder, have demonstrated high heritability.6,14,18,31 Symptoms of ADHD and comorbid psychiatric disorders often overlap, and their shared symptoms suggest possible similarities at the biological level, particularly common genetic risk factors.6,14,18,31,32,33 In this study, we found that certain internalizing disorders (i.e., anxiety disorders) and externalizing disorders (i.e., impulse control disorder, OCD, and CD) tended to occur together. It was reported that polymorphism of tryptophan hydroxylase,2 the rate-limiting enzyme for serotonin synthesis, is associated with traits of aggressiveness, impulsiveness, and anxiety,32 and that individuals with the TPH2 rs4570625 TT genotype exhibit less aggression and a favorable impulsivity profile along with a lower risk of developing anxiety disorders by young adulthood.32 These findings suggest that genetic mechanisms underlying the co-occurrence of certain internalizing and externalizing disorders might exist.
On the other hand, studies searching for common genetic factors related to psychiatric disorders have obtained somewhat conflicting results with regard to the genetic associations of ADHD.18,33,34 Several studies have suggested that ASD and ADHD share a common genetic basis.18 However, a recent genome-wide association study (GWAS) exploring genetic relations among five psychiatric disorders (schizophrenia, bipolar disorder, major depressive disorder, ADHD, and ASD) found an unexpected lack of genetic overlap between ASD and ADHD.33 Another GWAS assessing the relationship between genetic factors, personality traits, and psychiatric disorders observed a strong genetic correlation between ADHD and extroverted personality traits and a weak correlation with other psychiatric disorders (except bipolar disorder), suggesting that ADHD might be clustered with personality traits rather than psychiatric disorders.34 Such data support the hypothesis that attentional and associated symptoms represent a continuum rather than discrete categories.35 While this does not mean that dysfunction due to ADHD is not worthy of clinical attention, it calls into question the current classification of ADHD. It is possible that ADHD is an extremely heterogeneous disorder and the present categorical classification contributes to inconsistent results in studies of genetic associations among ADHD and other psychiatric disorders. With regard to the psychiatric comorbidities associated with ADHD, further studies using a dimensional approach could help to clarify the etiology of such psychiatric comorbidities in patients with ADHD.6,36 The dimensional approach could also be important for redefining the subtypes of ADHD, including comorbid psychiatric symptoms. Our present findings regarding the patterns of other psychiatric disorders in ADHD may provide useful information for such approaches.
Limitations. This study only enrolled adult patients with ADHD who had recently commenced treatment with OROS-MPH, suggesting that sampling bias should be considered when interpreting the findings, particularly with regard to the prevalence of comorbidities. In previous studies, the most frequent comorbidities associated with adult ADHD were mood and anxiety disorders as well as substance use disorder.1,6,8,13 In fact, some previous surveys showed that more than 10 percent of adult patients with ADHD also had substance use disorder,1,8 whereas the prevalence rate in our study was only 1.56 percent. The prevalence rate of bipolar disorder was also lower in our study than in previous surveys (6.43% vs. more than 10%, respectively).1,8 It is possible that the lower prevalence rates of these disorders in our study could be explained by selection bias. Although the use of long-acting stimulants in patients with ADHD and bipolar disorder has been advocated after stabilizing the mood with appropriate medications,14 there have been concerns about the potential risk of stimulant-associated mania/hypomania.15 Also, in patients with ADHD and concomitant substance use disorder, concern exists regarding medication diversion and the potential misuse of stimulants. Therefore, the literature has suggested that nonstimulants should be selected as first-line pharmacologic treatment for adults with ADHD and comorbid substance use disorder.16 These concerns could have influenced the registration of subjects in this study and might have contributed to the relatively low prevalence rates of bipolar disorder and substance use disorder.
Another limitation that should also be taken into consideration when interpreting these results is that comorbid psychiatric disorders were diagnosed in our study according to the clinical judgment of the attending physicians (mainly psychiatrists) rather than by way of structured interviews. This could raise some degree of concern about diagnostic accuracy, but the purpose of this study was to determine the prevalence of comorbidities in the real world, so diagnosis based on the physician’s clinical judgment seems to be a suitable method.
Conclusion
Although inherent selection bias should be taken into consideration when interpreting the results of this study, we found a high prevalence of psychiatric comorbidities in adult ADHD. The comorbidity patterns identified in our study could provide useful information for making a more accurate diagnosis of adult ADHD and support new insights for future investigations into the etiology of this disorder.
References
- Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–723.
- Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402–409.
- Nutt DJ, Fone K, Asherson P, et al. Evidence-based guidelines for management of attention-deficit/hyperactivity disorder in adolescents in transition to adult services and in adults: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2007;21(1):10–41.
- Nierenberg AA, Miyahara S, Spencer T, et al. Clinical and diagnostic implications of lifetime attention-deficit/hyperactivity disorder comorbidity in adults with bipolar disorder: data from the first 1000 STEP-BD participants. Biol Psychiatry. 2005;57(11):1467–1473.
- Gillberg C, Gillberg IC, Rasmussen P, et al. Co-existing disorders in ADHD—implications for diagnosis and intervention. Eur Child Adolesc Psychiatry. 2004;13 Suppl 1:180–192.
- Katzman MA, Bilkey TS, Chokka PR, et al. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. 2017;17(1):302.
- Canadian Attention Deficit Hyperactivity Disorder Resource Alliance. (CADDRA): Canadian ADHD Practice Guidelines. 3rd Ed. Toronto ON: CADDRA; 2011. https://www.aepap.org/sites/default/files/documento/archivos-adjuntos/gpc_tdah_canada_2011.pdf.
- Cumyn L, French L, Hechtman L. Comorbidity in adults with attention-deficit hyperactivity disorder. Can J Psychiatry. 2009;54(10):673–683.
- Jensen PS, Hinshaw SP, Kraemer HC, et al. ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry. 2001;40(2):147–158.
- Elia J, Ambrosini P, Berrettini W. ADHD characteristics: I. Concurrent co-morbidity patterns in children & adolescents. Child Adolesc Psychiatry Ment Health. 2008;2(1):15.
- Epstein JN, Johnson DE, Conners CK. Conners’ Adult ADHD Diagnostic Interview for DSM-IV. North Tonawanda, NY: Multi-Health Systems; 2001.
- Oksanen J. Multivariate analysis of ecological communities in R. Available at: http://cc.oulu.fi/~jarioksa/opetus/metodi/vegantutor.pdf.
- Young S, Sedgwick O, Fridman M, et al. Co-morbid psychiatric disorders among incarcerated ADHD populations: a meta-analysis. Psychol Med. 2015;45(12):2499–2510.
- Klassen LJ, Katzman MA, Chokka P. Adult ADHD and its comorbidities, with a focus on bipolar disorder. J Affect Disord. 2010;124(1-2):1–8.
- Wingo AP, Ghaemi SN. Frequency of stimulant treatment and of stimulant-associated mania/hypomania in bipolar disorder patients. Psychopharmacol Bull. 2008;41(4):37–47.
- Wilens TE. Impact of ADHD and its treatment on substance abuse in adults. J Clin Psychiatry. 2004;65 Suppl 3:38–45.
- Torgersen T, Gjervan B, Rasmussen K. ADHD in adults: a study of clinical characteristics, impairment and comorbidity. Nord J Psychiatry. 2006;60(1):38–43.
- Leitner Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children—what do we know?. Front Hum Neurosci. 2014;8:268.
- Davis NO, Kollins SH. Treatment for co-occurring attention deficit/hyperactivity disorder and autism spectrum disorder. Neurotherapeutics. 2012;9(3):518–530.
- Lee DO, Ousley OY. Attention-deficit hyperactivity disorder symptoms in a clinic sample of children and adolescents with pervasive developmental disorders. J Child Adolesc Psychopharmacol. 2006;16(6):737–746.
- Gadow KD, DeVincent CJ, Pomeroy J. ADHD symptom subtypes in children with pervasive developmental disorder. J Autism Dev Disord. 2006;36(2):271–283.
- Mulligan A, Anney RJ, O’Regan M, et al. Autism symptoms in Attention-Deficit/Hyperactivity Disorder: a familial trait which correlates with conduct, oppositional defiant, language and motor disorders. J Autism Dev Disord. 2009;39(2):197–209.
- St. Pourcain B, Mandy WP, Heron J, et al. Links between co-occurring social-communication and hyperactive-inattentive trait trajectories. J Am Acad Child Adolesc Psychiatry. 2011;50(9):892–902.
- Mancini C, Van Ameringen M, Oakman JM, Figueiredo D. Childhood attention deficit/hyperactivity disorder in adults with anxiety disorders. Psychol Med. 1999;29(3):515–525.
- Braaten EB, Beiderman J, Monuteaux MC, et al. Revisiting the association between attention-deficit/hyperactivity disorder and anxiety disorders: a familial risk analysis. Biol Psychiatry. 2003;53(1):93–99.
- Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999 Jan;40(1):57–87.
- Singh I. Beyond polemics: science and ethics of ADHD. Nat Rev Neurosci. 2008;9(12):957–964.
- Kuja-Halkola R, Lichtenstein P, D’Onofrio BM, Larsson H. Codevelopment of ADHD and externalizing behavior from childhood to adulthood. J Child Psychol Psychiatry. 2015;56(6):640–647.
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Arch Gen Psychiatry. 2007;64(10):1145–1152.
- Yoshimasu K, Barbaresi WJ, Colligan RC, et al. Adults with persistent ADHD: gender and psychiatric comorbidities—a population-based longitudinal study. J Atten Disord. 2018;22(6):535–546.
- Franke B, Faraone SV, Asherson P, et al. The genetics of attention deficit/hyperactivity disorder in adults, a review. Mol Psychiatry. 2012;17(10):960–987.
- Laas K, Kiive E, Mäestu J, Vaht M, et al. Nice guys: Homozygocity for the TPH2 -703G/T (rs4570625) minor allele promotes low aggressiveness and low anxiety. J Affect Disord. 2017;215:230–236.
- Cross-Disorder Group of the Psychiatric Genomics Consortium, Lee SH, Ripke S, et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet. 2013;45(9):984–994.
- Lo MT, Hinds DA, Tung JY, et al. Genome-wide analyses for personality traits identify six genomic loci and show correlations with psychiatric disorders. Nat Genet. 2017;49(1):152–156.
- McLennan JD. Understanding attention deficit hyperactivity disorder as a continuum. Can Fam Physician. 2016;62(12):979–982.
- Karalunas SL, Fair D, Musser ED, et al. Subtyping attention-deficit/hyperactivity disorder using temperament dimensions: toward biologically based nosologic criteria. JAMA Psychiatry. 2014;71(9):1015–1024.





