by Aksha M. Memon, MBBS, MD, MPH; Jigar Katwala, MBBS, MD; Clarice Douille, BS; Caitlin Kelley, BS; and Varun Monga, MD
Dr. Memon is with Creighton University School of Medicine in Phoenix, Arizona. Mses. Douille and Kelley are second-year medical students at Creighton University School of Medicine in Phoenix, Arizona. Dr. Monga is with Banner Health, Banner Thunderbird Medical Center in Glendale, Arizona. Dr. Katwala is with Medical University of Americas in Charlestown, Nevis, Saint Kitts and Nevis.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest relevant to the contents of this article.
Innov Clin Neurosci. 2023;20(7–9):47–51.
Abstract
Objective: Compared to the general population, the risk of suicide is three times higher in patients with epilepsy and remains doubled for these patients even after adjusting for sociodemographic correlates of suicide in the absence of mental health comorbidities. Following the United States (US) Food and Drug Administration (FDA) alert prompting a black box warning regarding the association between suicidality and antiepileptic drugs (AEDs), several studies were conducted, the results of which have been ambiguous, with some demonstrating a positive association between suicidality and AEDs, while others did not. This systematic review of literature sought to study the relationship between suicidality and AEDs when used exclusively for treatment of epilepsy.
Methods: A comprehensive literature search was conducted on PubMed without time limits using a predefined search language. The search results were then subjected to a systematic screening process. Eight out of a total of 443 articles satisfying predefined inclusion and exclusion criteria were included in the review for final data extraction.
Results: Three studies found a significant association between suicide-related behavior and levetiracetam use in the treatment of epilepsy. One study reported a positive association of pregabalin use in patients with epilepsy under 40 years of age and high AED load with suicidality, independent of depression. The remaining four studies reported a significant association between positive family and personal history of psychiatric comorbidities and suicidality in epilepsy.
Conclusion: Although there were several methodological limitations, this review found an association between levetiracetam use and mental health comorbidities and the occurrence of suicidality in epilepsy. Larger prospective, randomized studies that overcome the limitations of current studies are required to provide definitive evidence on the occurrence of suicidality in patients with epilepsy and AED use.
Keywords: Antiepileptic drugs, epilepsy, suicide, suicidality, suicide-related behavior
Suicide is the 12th leading cause of death in the United States (US) general population.1 In 2020, a total of 1.2 million Americans attempted suicide, 45,797 died from suicide, and the age-adjusted suicide rate was 13.48 per 100,000 individuals.1 According to the World Health Organization (WHO), in 2019, more than 1 in 100 deaths globally were due to suicide, and 703,000 individuals die each year due to suicide,2 which is preventable.1,2 In patients with epilepsy, more than 11 in 100 deaths are attributed to suicide.3 Compared to the general population, the risk of suicide in patients with epilepsy is three times higher.4 The risk remains doubled even in those patients without psychiatric comorbidities that contribute to suicidal behavior and after adjusting for sociodemographic correlates of suicide.4 Another study reported that suicidal ideation, a risk factor for suicide, was prevalent in 1 in 4 patients with epilepsy.5 This increased risk of suicidality (ideation, attempt, or completed suicide) in epilepsy needs further exploration, with a focus on potential epilepsy-related causal factors, such antiepileptic drugs (AEDs), which are the focus of this review.
In January 2008, the United States Food and Drug Administration (FDA) issued a warning about an increased risk of suicidal thoughts and behaviors in patients treated with certain AEDs, based on analysis of data from 199 clinical trials.6 According to this analysis, 11 antiepileptic drugs (carbamazepine, felbamate, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, tiagabine, topiramate, valproate, and zonisamide) were associated with doubling the risk of suicidality in recipients, compared to a placebo.6 Following this black box warning, several retrospective observational studies were conducted to replicate the study findings, only to provide inconclusive evidence; some studies succeeded in showing this association7,8 whereas some failed.9 Grimaldi-Bensouda et al10 hypothesized that these studies yielded inconclusive evidence because of their reliance on data extracted from electronic healthcare databases, which are not robust enough to control for underlying, confounding conditions that could possibly contribute to suicidal behavior for which the AED might have been prescribed. Also, secondary analysis of data from electronic healthcare databases cannot help to determine the temporality between AED use and occurrence of suicidal behavior.10 Additionally, according to the current evidence, prevalence of psychiatric comorbidities is higher in patients with epilepsy than the general population, with 24 to 74 percent of these patients having a mood disorder,11 which is a risk factor for suicidality, as well as one of the clinical indications for use of certain AEDs.12 Thus, this review aims to research the association between the occurrence of suicidality and AEDs when used exclusively for treatment of epilepsy to avoid the confounding effect of any psychiatric comorbidities that are a risk factor for suicidal behavior.
The FDA warning has been under scrutiny, given that the complex relationship between suicidality and AEDs is bidirectional and multifactorial in origin and, as stated previously, there are no definitive answers.13 However, there was increased concern among neurologists following this warning, and patients or their caregivers were advised on the potentially increased risk of suicidality with AED use,14 and the black box warning became a part of the enclosure for all AEDs.13 Nonadherence to AEDs, the mainstay of epilepsy treatment, can pose dangers of its own by tripling mortality risk.13 Hence, the risk-benefit ratio must be considered before discontinuing an AED, and each patient receiving an AED must be subjected to thorough mental health screenings before initiating AED therapy.13 We believe that this systematized review of literature will add to the body of evidence and bridge the knowledge gap pertaining to the role of AEDs on suicidal behavior when used to treat seizures.
Methods
An electronic literature search was conducted on PubMed in July 2022, without time limits, using a search language combining f the following medical subject headings (MeSH) terms to maximize sensitivity: anticonvulsants, antiepileptic agents, antiepileptic drugs, drugs, antiepileptic,* anticonvulsant,* anticonvulsant drugs, suicide, self-injurious behavior.
Table 1 shows the selection strategy that was applied to the resultant PubMed database search. This search yielded 443 references, with one duplicate, the titles of which were manually screened in the first stage. An additional reference was discovered from another source. In cases of ambiguous titles, the abstracts were read to check for eligibility. Irrelevant titles were discarded (n=345).
The following inclusion and exclusion criteria were applied during the second stage of screening to 95 out of 98 articles (3 were irretrievable). The inclusion criteria were 1) study design: cross-sectional, case control, cohort, randomized controlled trial, or quasi-experimental; 2) publication type: peer-reviewed, English language; 3) studies examining the association of AED treatment for epilepsy with occurrence of suicidal behavior, defined as emergency hospital visits due to self-injurious behavior or suicide attempt, or death by suicide (International Classification of Diseases, 10th revision [ICD-10] codes X60–X84); and 4) study population: patients with clinically diagnosed epilepsy undergoing active treatment with antiepileptic drugs. The exclusion criteria were 1) study design: case reports, literature reviews, poster abstracts, and unpublished doctoral theses; 2) publication type: nonpeer-reviewed and non-English publications; and 3) studies examining the association between the use of AEDs for psychiatric indications other than epilepsy and suicidal behavior.
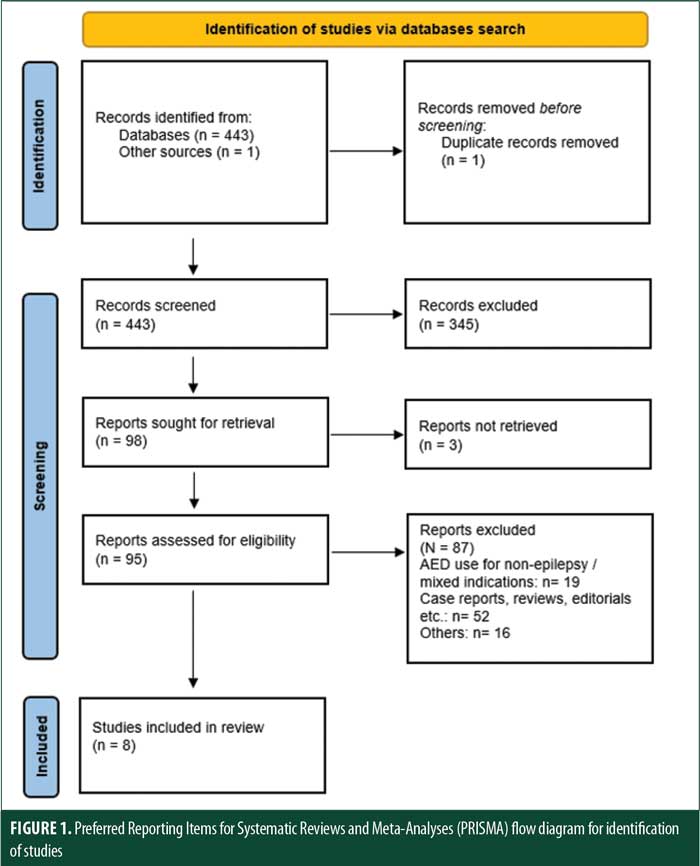
Eight7,10,14–19 out of 95 publications satisfied the above documented inclusion and exclusion criteria and were selected for data extraction and further analysis. The rest were excluded.
Results
See Table 2 for results.
Discussion
Immediately following the issuance of FDA alert,6 multiple studies were conducted to investigate the association between AED use and suicidality. However, there have not been any recent publications to provide new insights on the issue, except one review published in 2022.13 To the best of our knowledge, this is the first systematic review of literature assessing the complex interrelationship between AED use for the treatment of epilepsy and occurrence of suicidal behavior.
Data was extracted from eight studies7,10,14–19 that fulfilled the predefined inclusion and exclusion criteria. Pugh et al15 concluded that there was a significant association between suicide-related behavior and six specific AEDs, including valproate, gabapentin, lamotrigine, levetiracetam, phenytoin, and topiramate, after controlling for potential confounders, following the use of a new monotherapy AED prescription for one year. Andersohn et al7 reported a significant association between current use of levetiracetam (a newer AED with high depression potential, along with vigabatrin, tiagabine, and topiramate) and risk of self-harm/suicidal behavior. VanCott et al14 discovered an increased risk of suicide-related behavior with the use of levetiracetam and lamotrigine combined. Surprisingly, Kim et al19 found that pregabalin use in younger patients with epilepsy and high overall AED load were associated with suicidality, independent of depression. AED load was calculated as the sum of the prescribed daily dose divided by the defined daily dose ratios for levetiracetam, valproate/valproic acid, oxcarbazepine, carbamazepine, topiramate, lamotrigine, pregabalin, and perampanel. An AED load of one or greater was considered for analysis. The remainder of the studies10,16–18 failed to find any direct association between the use of AED and suicidality. Instead, these studies found that personal or family history of psychiatric comorbidities were greater predictors of increased risk of suicidality in patients with epilepsy than the use of any AED.
Aligning with these findings, the risk estimate of levetiracetam was highest in the FDA meta-analysis, with almost three times higher odds of suicidality out of the 11 AEDs studied.6 In a retrospective case registry data evaluation of 517 patients taking levetiracetam, four patients developed suicidality, but this was in the context of a mood disorder.21 Another systematic review on the behavioral effects of levetiracetam reported that behavioral events, such as affective and psychotic symptoms and suicidality, were more frequent in patients treated for epilepsy, compared to those treated for cognitive or anxiety disorders. However, the study concluded that these behavioral events were attributed to certain epilepsy-associated characteristics, rather than to the use of a particular AED.23 Considering all these nuances and that the studies7,14,15 with similar findings included in this review are of different methodologies and have their own limitations, it is still questionable if levetiracetam, as a specific agent, is responsible for the observed increase in suicidal behavior.
Considering the role of psychiatric illness in the occurrence of suicidality in epilepsy, the study by Wen et al16 reported that baseline depression or suicidal ideation were the strongest predictors of follow-up depression or suicidal ideation, after adjusting for AED type. VanCott et al14 also found a significant association between suicide-related behavior and a past diagnosis of affective disorder. Machado et al17 reported that the use of certain AEDs, including phenobarbital, phenytoin, topiramate, and primidone, was associated with depression. However, personal and family history of psychiatric comorbidities were associated with suicidality, rather than the use of AEDs. Grimaldi-Bensouda et al10 reported significant odds of suicide attempts with presence of lifetime depression and anxiety disorders. According to these findings, diagnosis of psychiatric comorbidities is equally relevant to occurrence of suicidality in epilepsy, compared to AED use.
The aforementioned findings are concordant with findings from a cross-sectional study conducted by Ding et al22 in China to study the association between possible risk factors and suicidality in adults with epilepsy. The findings revealed a strong association of poor family relationship and depression with suicidality. In a multicenter, cross-sectional study by Seo et al,23 major depressive disorder and generalized anxiety disorder emerged as strong predictors of suicidality in 684 Korean patients with epilepsy. These findings collectively suggest that psychiatric comorbidities in patients with epilepsy play a significant role as predictors of suicide-related behavior.
Strengths and limitations. The strengths of this review include its systematic nature, with the literature search being conducted using meticulous search terms and studies being screened using predefined inclusion and exclusion criteria to be considered eligible for data extraction; the inclusion of studies evaluating the use of AED exclusively for the treatment of epilepsy, which thus reduced the potential confounding effect of other AED indications, such as bipolar mood disorders and chronic pain; and the inclusion of studies conducted between 2010 to 2020, after the FDA alert. However, this review has multiple methodological limitations as well. Only one reviewer (AM) was involved in performing the final stage screening and article selection, which might have subjected the screening process to selection bias. Quality assessment of included articles was not performed. Finally, studies examining the association between AEDs and suicidality irrespective of clinical indications were excluded, thereby limiting the scope of determining the association between AEDs and the occurrence of suicidality.
Conclusion
Use of the AED levetiracetam and presence of psychiatric comorbidities are associated with the occurrence of suicide-related behavior in patients with epilepsy. Considering the limitations of our review, as well as those of the included studies, the generalizability of levetiracetam’s role in suicide-related behavior is still questionable. Larger, prospective, randomized studies overcoming limitations of the included studies are needed to show a definitive association. This review emphasizes the role that psychiatric comorbidities may play in the development of suicidality in patients with epilepsy, as supported by multiple previous studies. Hence, patients receiving AEDs for the treatment of epilepsy should undergo thorough psychiatric evaluation regularly for symptoms of depression, anxiety, and suicide-related behavior, and treatment should not be withheld even in cases of positive suicidal screen, as recommended by the ad hoc Task Force of the International League Against Epilepsy (ILAE) expert consensus in 2013.24
References
- American Foundation for Sucide Prevention. Suicide statistics. Updated 17 Feb 2022. https://afsp.org/suicide-statistics/. Accessed 8 Aug 2022.
- World Health Organization. Suicide. 17 Jun 2021. https://www.who.int/news-room/fact-sheets/detail/suicide. Accessed 8th Aug, 2022.
- Jones J, Hermann B, Barry J, et al. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2003;4(Suppl 3):S31–S38.
- Christensen J, Vestergaard M, Mortensen PB, et al. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol. 2007;6(8):693–698.
- Tellez-Zenteno JF, Patten SB, Jetté N, et al. Psychiatric comorbidity in epilepsy: a population-based analysis. Epilepsia. 2007;48(12):2336–2344.
- Kuehn BM. FDA warns of adverse events linked to smoking cessation drug and antiepileptics. JAMA. 2008;299(10):1121–1122.
- Andersohn F, Schade R, Willich SN, Garbe E. Use of antiepileptic drugs in epilepsy and the risk of self-harm or suicidal behavior. Neurology. 2010;75(4):335–340.
- Patorno E, Bohn RL, Wahl PM, et al. Anticonvulsant medications and the risk of suicide, attempted suicide, or violent death JAMA. 2010;303(14):1401–1409. Erratum in: JAMA. 2010;303(22):2252. Dosage error in article text.
- Arana A, Wentworth CE, Ayuso-Mateos JL, Arellano FM. Suicide-related events in patients treated with antiepileptic drugs. N Engl J Med. 2010;363(6):542–551.
- Grimaldi-Bensouda L, Nordon C, Rossignol M, et al. Antiepileptic drugs and risk of suicide attempts: a case-control study exploring the impact of underlying medical conditions. Pharmacoepidemiol Drug Saf. 2017;26(3):239–247.
- Gaitatzis A, Trimble MR, Sander JW. The psychiatric comorbidity of epilepsy. Acta Neurol Scand. 2004;110(4):207–220.
- Meyer JM. Pharmacotherapy of psychosis and mania. In: Brunton LL, Knollman BC, eds. Goodman & Gilman’s: The Pharmacological Basis of Therapeutics, Fourteenth Edition. McGraw Hill; 2022.
- Mula M. Suicidality and antiepileptic drugs in people with epilepsy: an update. Expert Rev Neurother. 2022;22(5):405–410.
- VanCott AC, Cramer JA, Copeland LA, et al. Suicide-related behaviors in older patients with new anti-epileptic drug use: data from the VA hospital system. BMC Med. 2010;8:4.
- Pugh MJV, Copeland LA, Zeber JE, et al. Antiepileptic drug monotherapy exposure and suicide-related behavior in older veterans. J Am Geriatr Soc. 2012;60(11):2042–2047.
- Wen X, Meador KJ, Loring DW, et al. Is antiepileptic drug use related to depression and suicidal ideation among patients with epilepsy? Epilepsy Behav. 2010;19(3):494–500.
- Machado RA, Espinosa AG, Melendrez D, et al. Suicidal risk and suicide attempts in people treated with antiepileptic drugs for epilepsy. Seizure. 2011;20(4):280–284.
- Rissanen I, Jääskeläinen E, Isohanni M, et al. Use of antiepileptic or benzodiazepine medication and suicidal ideation—the Northern Finland Birth Cohort 1966. Epilepsy Behav. 2015;46:198–204.
- Kim SJ, Kim HJ, Jeon J, et al. Clinical factors associated with suicide risk independent of depression in persons with epilepsy. Seizure. 2020;80:86–91.
- Mula M, Sander JW. Suicidal ideation in epilepsy and levetiracetam therapy. Epilepsy Behav. 2007;11(1):130–132.
- Cramer J. A systematic review of the behavioral effects of levetiracetam in adults with epilepsy, cognitive disorders, or an anxiety disorder during clinical trials. Epilepsy Behav. 2003;4(2):124–132.
- Ding S, Li X, Hua Y, Dong F, et al. Risk factors for suicidal tendency in adult patients with epilepsy in China. Epilepsy Behav. 2019;97:118–122.
- Seo JG, Lee JJ, Cho YW, et al. Suicidality and its risk factors in Korean people with epilepsy: a MEPSY Study. J Clin Neurol. 2015;11(1):32–41.
- Mula M, Kanner AM, Schmitz B, Schachter S. Antiepileptic drugs and suicidality: an expert consensus statement from the Task Force on Therapeutic Strategies of the ILAE Commission on Neuropsychobiology. Epilepsia. 2013;54(1):199–203.


