 by Masaru Nakamura, MD, PhD; Keigo Nakatsu, MD; and Takahiko Nagamine, MD, PhD
by Masaru Nakamura, MD, PhD; Keigo Nakatsu, MD; and Takahiko Nagamine, MD, PhD
Dr. Nakamura is with the Department of Psychiatric Internal Medicine, Kosekai-Kusatsu Hospital, Hiroshima, Japan; Dr. Nakatsu is with the Department of Psychiatry, Kosekai-Kusatsu Hospital, Hiroshima, Japan; and Dr. Nagamine is with the Department of Psychiatric Internal Medicine, Shinseikai-Ishii Memorial Hospital, Iwakuni, Japan.
Innov Clin Neurosci. 2015;12(11–12):18–20.
Funding: No funding was received for the preparation of this manuscript.
Financial Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Lithium, sinus node dysfunction, cardiac toxicity, therapeutic level, ECG, psychiatry
Abstract
Lithium carbonate (lithium) has been used extensively for the treatment of a variety of psychiatric conditions. It requires close monitoring of serum concentration due to its narrow therapeutic window. Cardiac toxicity range from asymptomatic electrocardiographic changes to fatal arrhythmias may occur even at the therapeutic levels. We report a case of psychiatric inpatient who developed asymptomatic severe bradycardia most likely related to sinus node dysfunction due to acute lithium treatment at therapeutic level. After withdrawal of lithium, a time sequential improvement of severe bradycardia examined by repeated electrocardiogram, including Holter monitoring, suggested a relationship between the lithium toxicity and sinus node dysfunction. Other factors such as baseline sinus bradycardia and lower limit of normal thyroid function might be associated with severe bradycardia. This case emphasizes the need, when prescribing lithium, for clinicians to regularly monitor their patients’ electrocardiogram and serum lithium levels to prevent serious or fatal complications, such as cardiac arrest.
Introduction
Lithium, a small monovalent cation, is used as an antimanic and mood-stabilizing drug combined with antipsychotics in the psychiatry clinical setting. Although evidence for both the safety and the efficacy of lithium has been established, serum lithium concentration is easy to exceed therapeutic levels because of its narrow therapeutic range, which may lead to serious physical complications.[1]
Lithium salts are highly water-soluble and are well absorbed by gastrointestinal tract. Complete absorption occurs in about eight hours, with peak concentration occurring 2 to 4 hours after an oral dose. Lithium is initially distributed in the extracellular fluid and then accumulates gradually in various tissues. Approximately 95 percent of a single dose is eliminated in the urine; with repeated administration, the excretion increases until a steady state is reached after 5 to 7 days.[2]
Cardiac disorders, including myocarditis, ventricular arrhythmias, and sinus-node dysfunction, are among several adverse effects of lithium, and are important clinical considerations.[3,4] There are various mechanisms by which lithium is postulated to cause these conduction abnormalities. Lithium’s interference with other cations’ exchange across cardiac cell membranes (e.g., K+, Na+, and Ca++) causes decreases in the spontaneous depolarization of the sinus node, the velocity in the atrioventricular and intraventricular conduction, and the adrenergic response.[5,6]
Sinus node dysfunction caused by lithium treatment is usually observed in the setting of long-term use or toxic levels and is exceedingly rare in short-term treatment within therapeutic levels.[7–9] We present a case of asymptomatic lithium-induced severe bradycardia at therapeutic level after one-week introduction.
Case presentation
A 36-year-old Japanese female patient with a 12-year history of schizophrenia presented to our hospital with exacerbation of psychiatric symptoms. After admitting her to the hospital, we decided to continue her current regimen of olanzapine (20mg/day) and paliperidone (9mg/day) for delusions and auditory hallucinations and eszopiclone (2mg/day) for sleeping disturbances but added lithium carbonate (400mg/day) for irritation.
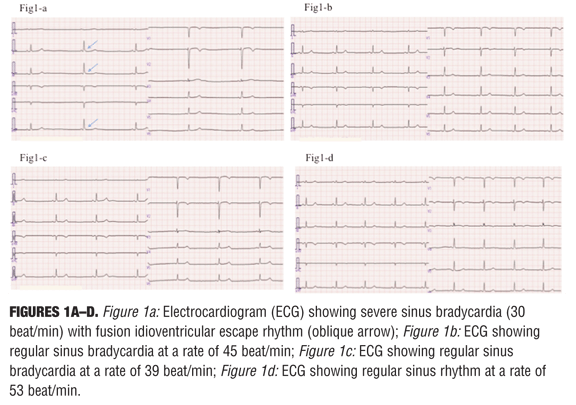
One week later, we noted the patient to have asymptomatic bradysphygmia (30–33 beats per minute [bpm]) with normal blood pressure of 91/56mmHg, as measured by the nursing staff. We then performed an electrocardiogram (ECG), which was suggestive of sinus bradycardia with a partial fusion idioventricular escape rhythm of 30 bpm (Figure 1a). There were no abnormalities in her physical findings, chest X-ray, and echocardiogram at this time. The hematological, renal and liver function tests, and serum electrolytes were also normal except for a lower limit of normal index in the thyroid function test (thyroid stimulating hormone, 4.50?U/mL; free triiodothyronine, 2.2pg/mL; free thyroxine 0.8ng/dL). Her serum lithium concentration (0.61mEq/L) was within therapeutic range. She had no history of syncope attack or heart disease, but had been diagnosed with bradycardia 13 years previously. A month earlier, prior to administration of litium, an ECG showed regular sinus bradycardia with heart rate of 45bpm (Figure 1b). Based on both records of ECG, we determined that the lithium carbonate aggravated the patient’s sinus node function and further decreased her heart rate. Therefore, we discontinued the lithium carbonate. The follow-up 12-lead ECG examination two days later revealed an improvement of sinus node function with regular sinus rhythm (39bpm) (Figure 1c) (53bpm 25 days later [Figure 1d]). To rule out idiopathic sick sinus syndrome (SSS) and to investigate the relationship between lithium carbonate and sinus node function, a 24-hour Holter ECG monitoring was performed 12 days and 30 days later. Results showed sinus rhythm throughout without fatal arrhythmia and just sustained bradycardia in the middle of the night—heart rate total: 69,971 to 81,294 per day, with a variability of 32–75bpm to 34–115 bpm, which suggests the sequential improvement of cardiac conduction system on the cessation of lithium therapy. Thirty-six days later, the patient was discharged from the hospital on olanzapine, paliperidone, and eszopiclone, and continued outpatient treatment with our department of psychiatry.
Discussion
The pathophysiological findings in the present case can be summarized as follows: 1) before the lithium treatment was added, sinus bradycardia had been observed by routine ECG monitoring; 2) after one week introduction of lithium, sinus node dysfunction was detected; 3) serum lithium concentration was within therapeutic range; 4) the cessation of lithium treatment led to an improvement of sinus node dysfunction; and 5) the findings of repeated standard 12-lead and Holter ECG studies suggested a gradual elimination of lithium from the myocardium.
Cardiac effects attributed to lithium toxicity occur in 20 to 30 percent of patients. Asymptomatic ECG changes are the most common and include T wave changes (e.g., flattening, isoelectricity, or inversion).[8] Infrequently, clinically evident cardiac manifestations occur that may require temporal pacemaker implantation (including sinus node dysfunction); rarely, more fatal manifestiations may occur, such as prolonged QT interval, ventricular tachycardia, and ventricular fibrillation.[9]
The fact that not all patients receiving lithium develop sinus node dysfunction suggests that there may be other factors accentuating conduction defects, including the following: Fluctuation in serum lithium levels;[3] intrinsic parasympathetic and sympathetic tone;[12] age-related interstitial fibrosis and decrease in sinus rate;[13] variations in cardiac sodium channel expression;[14] underlying pre-existing cardiac disease;[4] and medications that affect renal funtion, such as nonsteroidal anti-inflammatory drugs (NSAIDs), angiotensin converting enzyme inhibitors (ACE-I), or receptor blockers (ARB).[15]
In the present case, lithium treatment exacerbated sinus node dysfunction, and discontinuation of lithium carbonate resulted in the recovery from severe bradycardia that was observed in the daytime. The results of repeated ECG monitoring confirmed the relationship between the lithium toxicity and sinus node dysfunction.
Conclusion
Our case strongly suggests that sinus node dysfunction of lithium can occur even with lithium levels in the therapeutic range and in short-term “acute” treatment. Therefore, patients receiving lithium therapy should have their pulse monitored regulatory for any rhythm abnormalities, and lithium should be discontinued if rhythm disturbances occur during treatment. Further, when prescribing lithium, clinicians should regularly monitor their patients’ ECG and serum lithium levels to prevent serious or fatal complications.
Acknowledgment
The authors would like to thank our colleagues throughout Kosekai-Kusatsu Hospital for their assistance with this case report. The authors have no conflict of interest to this report.
References
1. Linakis JG, Toxicity, lithium. Last Updated: January 8, 2007. Medscape website. http://www.emedicine.com/emerg/topic301.htm, Accessed November 1, 2015.
2. Baldesarini RJ, Tarazi FI. Drugs and the treatment of psychiatric disorders: psychosis and mania. In: Hardman JG, Limbird LE (eds). Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 10th editon. New York: McGraw-Hill; 2001:507–511.
3. Livingstone C, Rampes H. Lithium: a review of its metabolic adverse effects. J Psychopharmacol. 2006; 20:347–355.
4. Darbar D, Yang T, Churchwell K, et al. Unmasking of brugada syndrome by lithium. Circulation. 2005;112:1527–1531.
5. Bogdanov KY, Vinogradova TM, Lakatta EG. Sinoatrial nodal cell ryanodine receptor and Na(+)-Ca(2+) exchanger: molecular partners in pacemaker regulation. Circ Res. 2001;88:1254–1258.
6. Azene EM, Xue T, Li RA. Molecular basis of the effect of potassium on heterologously expressed pacemaker (HCN) channels. J Physiol. 2003;547:349–356.
7. Oudit GY, Korley V, Backx PH, et al. Lithium-induced sinus node disease at therapeutic concentrations: linking lithium-induced blockade of sodium channels to impaired pacemaker activity. Can J Cardiol. 2007;23:229–232.
8. Singh LK, Praharaj SK, Munda SK, et al. Lithium-induced sinus node dysfunction at therapeutic serum levels. Natl Med J India. 2011;24:151–152.
9. Shetty RK, Vivek G, Parida A, et al. Lithium-induced sinus node dysfunction at therapeutic levels. BMJ Case Reports. 2013 Jan 22. doi: 10.1136/bcr-2012-008107
10. Demers RG, Heninger GR. Electrocardiographic T-wave changes during lithium carbonate treatment. JAMA. 1971;218:381–386.
11. Talati SN, Aslam AF, Vasavada B. Sinus node dysfunction in association with chronic lithium therapy: a case report and review of literature. Am J Ther. 2009;16:274–278.
12. Perini R, Veicsteinas A. Heart rate variability and autonomic activity at rest and during exercise in various physiological conditions. Eur J Appl Physiol. 2003;90:317–325.
13. Opthof T. The normal range and determinants of the intrinsic heart rate in man. Cardiovasc Res. 2000;45:173–176.
14. Bezzina CR, Shimizu W, Yang P, et al. Common sodium channel promoter haplotype in asian subjects underlies variability in cardiac conduction. Circulation. 2006;113:338–344.
15. Nagamine T. Lithium Intoxication Associated with Angiotensin II Type 1 Receptor Blockers in Women. Clin Neuropsychopharmacol Ther. 2013;4:23–25.





