by Donna Vanderpool, MBA, JD
by Donna Vanderpool, MBA, JD
Ms. Vanderpool is Director of Risk Management at Professional Risk Management Services (PRMS)
FUNDING: No funding was provided for the preparation of this article.
DISCLOSURES: The author is an employee of PRMS. PRMS manages a professional liability insurance program for psychiatrists.
This ongoing column is dedicated to providing information to our readers on managing legal risks associated with medical practice. We invite questions from our readers. The answers are provided by PRMS (www.prms.com), a manager of medical professional liability insurance programs with services that include risk management consultation and other resources offered to health care providers to help improve patient outcomes and reduce professional liability risk. The answers published in this column represent those of only one risk management consulting company. Other risk management consulting companies or insurance carriers might provide different advice, and readers should take this into consideration. The information in this column does not constitute legal advice. For legal advice, contact your personal attorney. Note: The information and recommendations in this article are applicable to physicians and other health care professionals so “clinician” is used to indicate all treatment team members.
Innov Clin Neurosci. 2020;17(10–12)
Question
I think I finally understand what the telepsychiatry rules are during the pandemic. But what happens when the government determines the pandemic is over? Will all of the pre-COVID-19 requirements go back into effect?
Answer
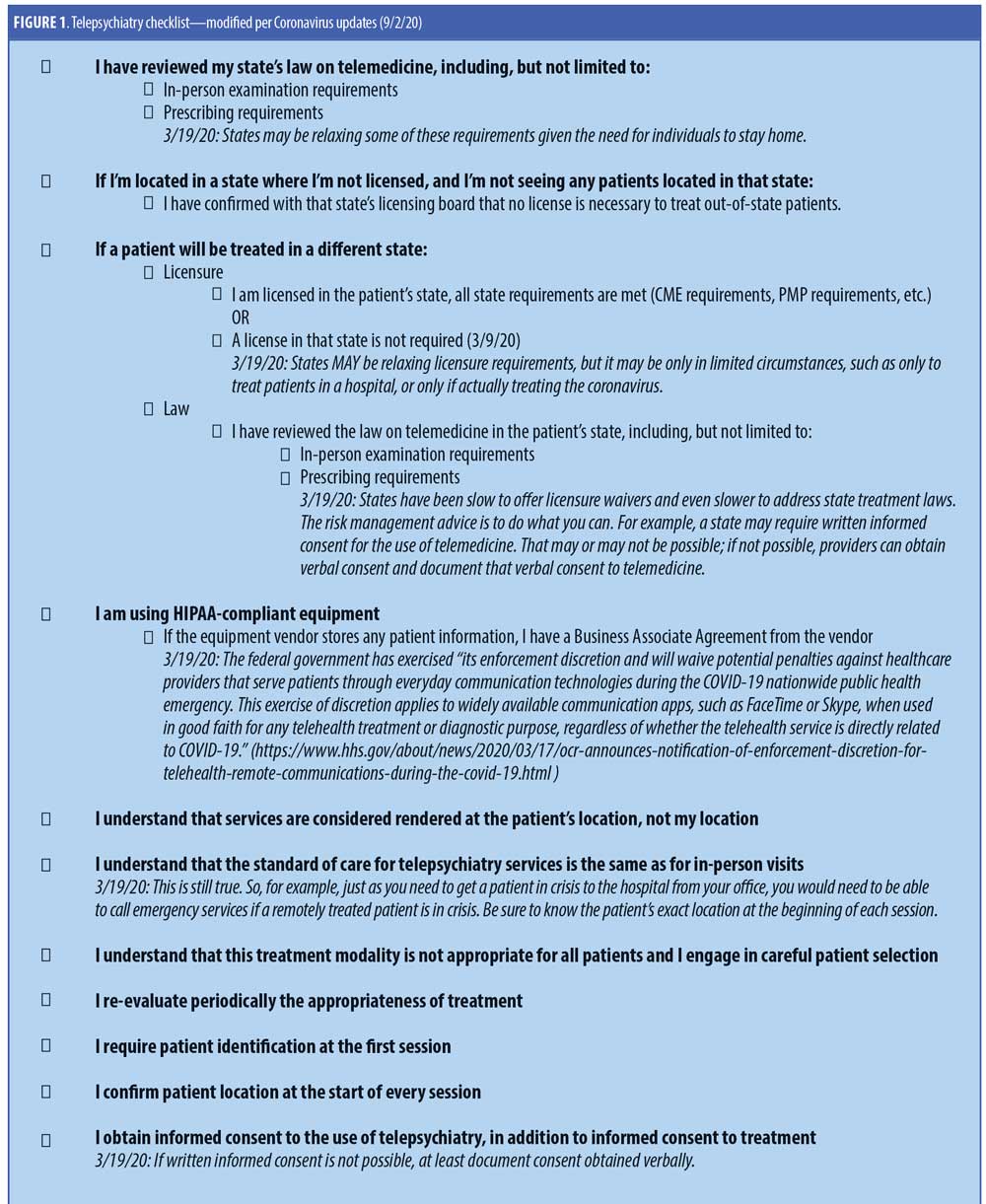
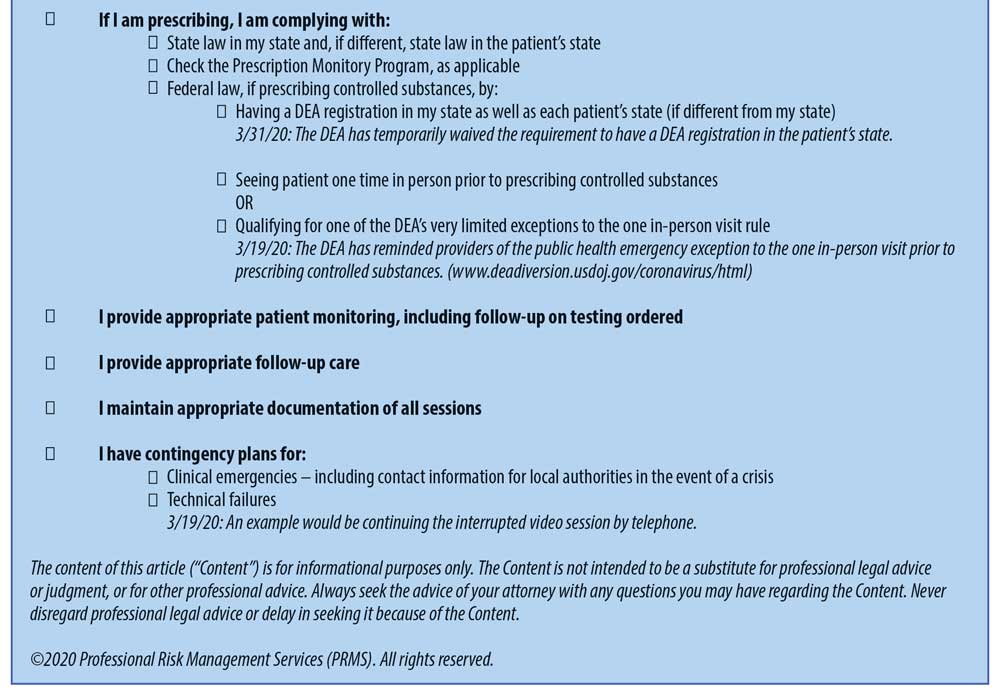
This is uncharted territory and there currently are unresolved issues. The Telepsychiatry Checklist includes the current administrative requirements. There will be more uncertainty in the future as we emerge from the COVID-19 public health emergency (PHE). The federal PHE is currently set to expire January 20, 2021, but it could be extended again. While we do not know exactly what will happen in the future, clinicians should be prepared to address at least the following issues:
1. Re-opening Your Physical Office
You should review guidelines and best practices from your state, from both your health officials and the state medical society. Additionally, you might want to review the following guidelines:
AMA
- Guide: www.ama-assn.org/delivering-care/public-health/covid-19-physician-guide-keeping-your-practice-open
- Checklist: www.ama-assn.org/system/files/2020-08/physican-guide-keep-practices-open-covid-19.pdf
- MGMA (Medical Group Management Association): www.mgma.com/MGMA/media/files/pdf/MGMA-Practice-Reopening-Checklist.pdf?ext=.pdf
2. For Patients That Stayed Local, Determine Whether They Need to Be Seen In-person, Remotely, or a Combination of Both
Most patients have been pleased to receive services remotely and would in fact prefer to continue virtual visits for convenience. You, as the clinician, need to make this decision based on your determination of the patients’ clinical needs, not on the patients’ preference for telepsychiatry.
3. For Patients Currently Out of State, Determine if They Have Imminent Plans to Return to Your State
Manage patient expectations and let them know that the rules might be changing soon, and you might not be able to continue to treat remotely. While the federal government has extended the PHE to at least January 2021, states might have earlier expiration of their emergency declarations.
4. Track State Licensure Waivers in Your Patients’ States
They might expire on specific dates, be extended, or withdrawn at any point. PRMS is tracking these changes and making updates available online to all at www.prms.com/faq.
Do keep in mind that the federal government, via the Centers for Medicare and Medicaid Services, has temporarily waived the requirement to be licensed in the patient’s state. However, that is only relevant in terms of Medicare and Medicaid payments. The federal government does not control licensing of healthcare providers (that is left to the states). So, while you might think you do not need to worry about licensure requirements in your Medicare patients’ states, you still need to meet the states’ licensure requirements.
5. Once the Licensure Waiver No Longer Exists for a State Where Your Patient is, Check to See What is Needed to Continue to Treat Your Patient Via Telemedicine
States might require full licensure, a telemedicine registration, or nothing to continue to treat existing patents. You might want to check with your risk managers or malpractice insurance company to obtain this information.
6. If After The Waiver Ends, You Are Allowed to Continue to See the Out-of-state patient, Determine and Follow That State’s Standard Telemedicine Rules That Will Likely Be Back in Effect
States can have laws addressing requirements for elements, such as in-person visits, informed consent, and documentation. If your patient’s state does not have such laws, follow the telemedicine guidelines developed by the Federation of State Medical Boards, available at www.fsmb.org/siteassets/advocacy/policies/fsmb_telemedicine_policy.pdf .
Your risk managers or malpractice insurance company might be able to assist in obtaining this information.
7. If After the Waiver Ends, You Are Not Able to Continue Treating the Out-of-state patient (i.e., Full Licensure is Required), Terminate Treatment
However, you do not want to abandon your patients, so you might want to consider giving 30 days’ notice.
8. If After the Waiver Ends, and Licensing Requirements Have Been Adhered to, Adhere to the Patient’s State’s Prescribing Laws
There might be specific state laws, such as for in-person visits when prescribing controlled substances.
You should also register and use, to the extent possible, the state’s prescribing drug monitoring program.
9. If You Are Prescribing Controlled Substances to Patients Out-of-state, Watch for When The Department Of Health And Human Services (HHS) Declares the End of the PHE
The current PHE declaration is set to expire in January, but it could be extended again.
When the PHE ends, two currently suspended federal requirements for prescribing controlled substances will likely go back into effect.
First, the in-person visit requirement prior to prescribing controlled substances will likely go back into effect. It is unclear whether the United States Drug Enforcement Administration (DEA) will require an in-person visit after the PHE for those who were prescribed controlled substances without it during the PHE.
Second, the requirement to have a federal DEA registration in the patient’s state (as well as in your state) will likely go back into effect.
10. When the PHE Ends, Telemedicine Likely Needs to Go Back to Being Done Via A Hipaa-Adherent Telemedicine Platform
HHS temporarily waived the requirement for Health Insurance Portability and Accountability Act (HIPAA)-adherent telemedicine platforms during the PHE. Post-PHE, you will need a Business Associate Agreement (BAA) from the vendor.