by Randy A. Sansone, MD, and Lori A. Sansone, MD
by Randy A. Sansone, MD, and Lori A. Sansone, MD
R. Sansone is a professor in the Departments of Psychiatry and Internal Medicine at Wright State University School of Medicine in Dayton, OH, and Director of Psychiatry Education at Kettering Medical Center in Kettering, OH. L. Sansone is a civilian family medicine physician and Medical Director of the Family Health Clinic at Wright-Patterson Air Force Base Medical Center in WPAFB, OH. The views and opinions expressed in this article are those of the authors and do not reflect the official policy or position of the United States Air Force, Department of Defense, or United States Government.
Innov Clin Neurosci. 2013;10(4):36–40
This ongoing column is dedicated to the challenging clinical interface between psychiatry and primary care—two fields that are inexorably linked.
Funding: There was no funding for the development and writing of this article.
Financial Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Axis II, binge eating disorder, borderline, borderline personality, eating disorders, obesity
Abstract: Obesity is a significant health problem in the United States. Therefore, it is extremely important to understand potential clinical associations with obesity, including personality pathology. From studies of personality disorders in other types of eating pathology, it appears that restrictive personality disorders (e.g., obsessive-compulsive disorder) are associated with restrictive eating pathology (e.g., anorexia nervosa, restricting type) whereas impulsive personality disorders (e.g., borderline personality disorder) are associated with impulsive eating pathology (e.g., anorexia nervosa, binge-eating/purging type; bulimia nervosa, binge eating disorder). Because binge eating disorder is oftentimes associated with an obese status, it seems likely that borderline personality disorder may also be associated with obesity. At the present time, there appear to be nine accessible studies in this area, comprising 639 obese individuals. While rates of borderline personality disorder in these studies vary from 2.2 to 94.1 percent, 10 of 19 measures detected this disorder at rates of 25 percent or higher, and the average of all percentages is 26.9 percent. Findings appear to support the association between impulsive personality pathology and impulsive eating pathology, and underscore that a significant minority of obese individuals may suffer from borderline personality disorder.
Introduction
Obesity continues to be a major health concern in the United States. According to the Centers for Disease Prevention and Control, 35.7 percent of adults and approximately 17 percent of children in the United States are obese.[1] The individual states with the highest rates of obesity (>30%) include Alabama, Arkansas, Kentucky, Louisiana, Michigan, Mississippi, Missouri, Oklahoma, South Carolina, Tennessee, Texas, and West Virginia.[1] As for etiology, obesity appears to be a multidetermined syndrome with contributions from both genetics and the environment. Personality pathology may also play a unique role in obesity. In this edition of The Interface, we discuss the possible relationship between one specific personality disorder, borderline personality disorder (BPD), and obesity. We begin by presenting data on complimentary styles between personality pathology and eating pathology, then review the prevalence of BPD in obesity as well as discuss the possible nature of this association.
Impulsivity: An Essential Feature of Borderline Personality Disorder
In the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR),[2] BPD is categorized as a Cluster B personality disorder (i.e., this disorder resides in the emotional, dramatic, erratic cluster of personality disorders). The DSM-IV-TR describes BPD as a “pervasive pattern of instability” characterized by “marked impulsivity” that affects approximately two percent of the general population. To illustrate possible manifestations of impulsivity, the DSM-IV-TR provides, among others, the example of binge eating behavior. In doing so, the DSM-IV-TR affirms a distinct association between this specific type of personality pathology and impulsive eating behavior.
Relationships between Personality Disorder Style and Eating Pathology
In our previous work, we have noted general associations between personality disorder style and eating pathology.[3] In other words, the style of the personality pathology appears to compliment the style of the eating pathology. As an example, anorexia nervosa, restricting type, is psychologically characterized by high levels of personal control and restraint. When we examined 10 empirical studies on the types of personality pathology encountered in anorexia nervosa, restricting type, we found that obsessive-compulsive personality was the most common (prevalence rate of approximately 22%)—a personality pathology that is characterized by a preoccupation with details and order, perfectionism, excessive devotion to projects, inflexibility, and rigidity.2 In further support of this association, Cassin and von Ranson state that multidimensional perfectionism is a salient correlate in anorexia nervosa.[4]
In contrast to anorexia nervosa restricting type, anorexia nervosa binge-eating/purging type is characterized by high levels of impulsivity, which is manifest in both the behaviors of binge eating and purging. In our review of nine empirical studies on the personality pathology associated with this eating disorder, we found that BPD was the most common personality disorder (prevalence rate of approximately 25%).[3]
In further examination of the associations between personality pathology and eating pathology, we examined studies on the prevalence of various Axis II disorders in individuals with bulimia nervosa—another eating disorder that is characterized by impulsivity.[3] As expected, among the 28 empirical studies that we examined, we found that the personality disorder with the highest prevalence rate among individuals with bulimia nervosa was BPD, at a rate of around 28 percent.
From the preceding investigations, we concluded that the style of personality pathology confers an influence on the style of eating pathology, with restrictive personality pathology contributing to restrictive eating pathology, and impulsive personality pathology contributing to impulsive eating pathology.[5] Because personality disorders are believed to commence and consolidate in childhood through the interactions of genes and the environment, it is probable that personality pathology precedes eating pathology in most cases (eating disorders most often manifest in early-to-late adolescence). Therefore, a given personality pathology might be viewed as a potential risk factor for the subsequent development of a specific type of eating pathology.[5–7]
Borderline Personality and Binge Eating Disorder
Given the preceding perspective on relationships between personality pathology and eating pathology, it is reasonable to conjecture about possible relationships between BPD and obesity—an eating pathology that may be empirically characterized by impulsive eating. Partial evidence for impulsive eating patterns among individuals with obesity seems to currently lie within the literature on binge eating disorder.
Currently classified in the DSM-IV-TR as a criteria set for further study,[2] binge eating disorder is characterized by a recurrent pattern of binge eating that occurs at least twice a week for a minimum period of six months. The clinical characteristics of binge eating behavior in this disorder are like those encountered in bulimia nervosa.
Unlike the behavioral patterns observed in bulimia nervosa, there are no compensatory behaviors (e.g., vomiting, fasting, exercise) to counter the episodes of massive calorie ingestion in binge eating disorder. Therefore, many individuals with this syndrome wind up being overweight, although weight status, per se, is not a diagnostic criterion.
According to Bunnell[8] and Walsh, Wilfley, and Hudson,[9] the prevalence of binge eating disorder in the community is up to five percent, in weight loss clinics up to 30 percent, and in those with body mass indices (BMI) of 40 or greater, up to 50 percent. According to these prevalence data, in comparison with anorexia or bulimia nervosa, binge eating disorder is the most common eating disorder in existence. Unlike the traditional eating disorders, in binge eating disorder a substantial number of male individuals are affected, with the female to male ratio being 3:2.[8,9] The onset of this disorder is typically during the late teens to early 20s, the ethnicity of the patient population is diverse, and the age-of-presentation for treatment (i.e., 30–40 years) is later than that encountered in anorexia or bulimia nervosa.[8,9] This brief summary indicates that a number of individuals with obesity may suffer from binge eating disorder, an eating disorder characterized by impulsive eating behavior.
In a review of the literature on the relationship between BPD and binge eating disorder,[10] which was published in the year 2000, we encountered five relevant studies.[11–15] The prevalence rates of BPD among the various samples of individuals with binge eating disorder ranged from 6 to 30 percent. Rates of BPD were consistently higher in participants with binge eating disorder compared with controls. Since this review, we located two additional studies. In the first, van Hanswijck de Jonge et al reported that one out of 15 patients (6.6%) with binge eating disorder suffered from BPD.[16] In the second, Azuma et al found that Japanese participants with obesity and binge eating disorder had “characteristics of BPD.”[17] In summary, this collection of studies suggests that rates of BPD among individuals with binge eating disorder are generally higher than rates encountered in community samples.
Borderline Personality among individuals with Obesity
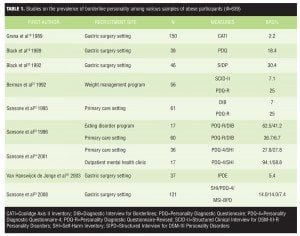
A number of studies have examined the prevalence of BPD among obese individuals (Table 1).[16,18–25] To summarize these data, among the nine studies displayed in Table 1, sample sizes vary from 17 to 150 individuals (i.e., they are generally small). The total number of participants in these nine studies is 639; they are from various socioeconomic classes and the majority are female. The prevalence rates for BPD in these studies varied from 2.2 to 94.1 percent. Several studies used multiple measures for BPD assessment. In examining results, 10 of 19 measures for BPD detected this disorder at rates of 25 percent or higher. Finally, averaging all of the reported percentages for BPD according to these various measures, 26.9 percent of participants met the criteria for BPD. In other words, a significant percentage of participants with obesity exhibited borderline personality symptomatology.
In addition to the preceding prevalence rates of BPD among individuals with obesity, there are two additionally important facets related to these data. First, in 5 of the 9 studies (over half), participants were recruited from gastric surgery sites. This finding may be particularly salient, as many of these individuals were examined during the assessment phase for gastric surgery. Given that assessments for BPD typically inquire about various self-harm behaviors (e.g., cutting oneself) as well as suicidal ideation and other self-regulation difficulties (e.g., promiscuity, alcohol/drug misuse), it seems feasible that a meaningful percentage of candidates would not disclose this information during the psychological assessment phase for fear of being disqualified for the surgery, regardless of whether such a disclosure would disqualify them or not. If so, then these findings may be appreciably under-reporting the actual prevalence rates of BPD in obesity.
Second, in comparing sample types, note that the lowest rate of BPD among individuals with obesity is reported in a gastric surgery sample whereas the highest rate of BPD is reported in a mental health sample. While disclosure is clearly a potential factor in explaining the differences between these two prevalence rates, setting may be an additional factor. Specifically, it is likely that more emotionally disturbed individuals with obesity are presenting for mental health treatment than for gastric surgery, thereby resulting in a relatively higher rate of BPD among individuals with obesity in mental health settings. Because of this possibility, clinicians in mental health settings need to be particularly aware of screening for BPD in patients who are obese, particularly in the presence of a comorbid mood disorder, an additional form of self-regulation difficulty (e.g., substance misuse), and/or repetitive self-harm behavior (e.g., suicide attempts, self-mutilation).
Temporal Associations: Contributory Relationships?
From the available studies, it appears that BPD is relatively infrequent among eating pathologies characterized by restrictive patterns and ubiquitous in eating pathologies characterized by impulsivity. Because personality pathology is born of genetics and early childhood experiences and eating pathology typically emerges in early-to-late adolescence, it is likely that personality pathology generally precedes eating pathology. Given this proposed temporal relationship, it may be that borderline personality pathology functions as one of several risk factors for the evolution of particular types of eating pathology—especially anorexia nervosa, binge-eating purging type; bulimia nervosa, binge eating disorder; and/or obesity. Importantly, these eating disorders are multidetermined and their etiologies cannot be simply ascribed to personality pathology. Therefore, personality pathology is probably best viewed as one of several contributory factors for impulsive eating pathology.
Conclusion
Obesity is a rampant health problem in the United States. Because of this, it is critical to understand relationships between obesity and other disorders as well as contributory variables. In this regard, personality pathology appears to influence eating pathology, such that restrictive personality pathology (e.g., obsessive-compulsive personality disorder) is most present in restrictive eating pathology, and impulsive personality pathology (e.g., borderline personality disorder) is most present in impulsive eating pathology. These relationships are reinforced by various empirical studies, which document significant rates of obsessive-compulsive personality and perfectionism in anorexia nervosa, restricting type, and significant rates of BPD in anorexia nervosa, binge-eating/purging type; bulimia nervosa, binge eating disorder; and obesity. For example, current data indicate that 27 percent of individuals with obesity harbor comorbid BPD. However, this percentage is likely to be low based upon the observation that 5 of 9 studies took place in gastric surgery settings, many during the assessment phase, thereby potentially compromising patient disclosure. In conclusion, BPD appears to be present in a significant minority of obese individuals, and likely is a contributory factor to initiating and maintaining an obese status.
References
1. Centers for Disease Control and Prevention. Obesity and overweight for professionals: data and statistics. Located at: http://www.cdc.gov/obesity/data/trends.HTML. Accessed on March 13, 2012.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Press Inc.; 2000.
3. Sansone RA, Sansone LA. The prevalence of personality disorders in those with eating disorders. In: Sansone RA, Levitt JL (eds). Personality Disorders and Eating Disorders. Exploring the Frontier. New York: Routledge;2006:23–39.
4. Cassin SE, von Ranson KM. Personality and eating disorders: a decade in review. Clin Psychol Rev. 2005;25:895–916.
5. Sansone RA, Sansone LA. Personality pathology and its influence on eating disorders. Innov Clin Neurosci. 2011;8(3):14–18.
6. Sansone RA, Sansone LA. Childhood trauma, borderline personality, and eating disorders: a developmental cascade. Eat Disord. 2007;15:333–346.
7. Sansone RA, Sansone LA. Borderline personality and eating disorders: a chaotic crossroads. In: Maine M, Bunnell D, McGilley B (eds). Special Issues in the Treatment of Eating Disorders: Bridging the Gaps. New York: Elsevier;2010:217–232.
8. Bunnell D. The “new” eating disorder. Perspective 2004;1:4–6.
9. Walsh BT, Wilfley DE, Hudson JI. Binge Eating Disorder: Progress in Understanding and Treatment. (Educational monograph). West Wayne, NJ: Health Learning Systems; 2003:1–14.
10. Sansone RA, Wiederman MW, Sansone LA. The prevalence of borderline personality disorder among individuals with obesity: a critical review of the literature. Eating Behav. 2000;1:93–104.
11. McCann UD, Rossiter EM, King RJ, Agras WS. Nonpurging bulimia: a distinct subtype of bulimia nervosa. Int J Eat Disord. 1991;10:679–687.
12. Yanovski SZ, Nelson JE, Dubbert BK, Spitzer RL. Association of binge eating disorder and psychiatric comorbidity in obese subjects. Am J Psychiatry. 1993;150:1472–1479.
13. Specker S, de Zwaan M, Raymond N, Mitchell J. Psychopathology in subgroups of obese women with and without binge eating disorder. Compr Psychiatry. 1994;35:185–190.
14. Abbott DE, de Zwaan M, Mussell MP, et al. Onset of binge eating and dieting in overweight women: implications for etiology, associated features and treatment. J Psychosom Res. 1998;44:367–374.
15. Telch CF, Agras WS. Psychiatric comorbidity in women with binge eating disorder: prevalence rates from a non-treatment-seeking sample. J Consult Clin Psychol. 1998;66:768-776.
16. Van Hanswijck de Jonge P, van Furth EF, Lacey JH, Waller G. The prevalence of DSM-IV personality pathology among individuals with bulimia nervosa, binge eating disorder and obesity. Psychol Med. 2003;33:1311–1317.
17. Azuma Y, Kodama K, Noda S, et al. Personality traits of simple obese patients with binge eating disorder. Clin Psychiatry. 2000;42:605-610.
18. Grana AS, Coolidge FL, Merwin MM. Personality profiles of the morbidly obese. J Clin Psychol. 1989;45:762?765.
19. Black DW, Yates WR, Reich JH, et al. DSM-III personality disorder in bariatric clinic patients. Ann Clin Psychiatry. 1989;1:33?37.
20. Black DW, Goldstein RB, Mason EE. Prevalence of mental disorder in 88 morbidly obese bariatric clinic patients. Am J Psychiatry. 1992;149:227?234.
21. Berman WH, Berman ER, Heymsfield S, et al. The incidence and comorbidity of psychiatric disorders in obesity. J Pers Disord. 1992;6:168–175.
22. Sansone RA, Sansone LA, Fine MA. The relationship of obesity to borderline personality symptomatology, self-harm behaviors, and sexual abuse in female subjects in a primary-care medical setting. J Pers Disord. 1995;9:254–265.
23. Sansone RA, Sansone LA, Morris DW. Prevalence of borderline personality symptoms in two groups of obese subjects. Am J Psychiatry. 1996;153:117?118.
24. Sansone RA, Wiederman MW, Sansone LA, Monteith D. Obesity and borderline personality symptomatology: comparison of a psychiatric versus primary care sample. Int J Obesity. 2001;25:299–300.
25. Sansone RA, Schumacher D, Wiederman MW, Routsong-Weichers L. The prevalence of binge eating disorder and borderline personality symptomatology among gastric surgery patients. Eat Behav. 2008;9:197-202.