by Julie P. Gentile, MD; Paulette Marie Gillig, MD, PhD; Kelly Stinson, MD; and Jeremy Jensen, MD
by Julie P. Gentile, MD; Paulette Marie Gillig, MD, PhD; Kelly Stinson, MD; and Jeremy Jensen, MD
Dr. Gentile is Professor, Department of Psychiatry, Wright State University, Dayton, Ohio; Dr. Gillig is Professor, Department of Psychiatry, Wright State University, Dayton, Ohio; Dr. Stinson is Administrative Chief Resident, Department of Psychiatry, Wright State University, Dayton, Ohio; and Dr. Jensen is Staff Psychiatrist, Scott Air Force Base, 375 MDOS/SGOW.
Innov Clin Neurosci. 2014;11(11–12):22–26.
Funding: No funding was provided.
Financial disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key words: Intellectual disability, developmental disability, dual diagnosis, behavioral support, psychotherapy
Abstract: Objective: The purpose of this study was to determine the effectiveness of psychiatric medical services, counseling, and behavioral treatments for adult patients with intellectual disabilities plus behavioral disorders and/or emotional distress. Methods: Behavioral and medical data were collected at six and 12 months for a consecutive series of 141 adult patients with mild, moderate, or severe/profound intellectual disabilities who had been referred to a dual diagnosis mental health clinic, and treatment outcomes were compared. Results: Most improvement in behavioral problem severity occurred at six months, then plateaued. Treatment improvement for subjects with anxiety disorders was statistically significant across all interventions. In this sample, as expected, patients with intellectual disability had higher incidences of medical illnesses than the general population. Conclusions: Subjects with more behavioral (overt) symptoms tended to receive referrals for behavioral support, and subjects with less overt symptoms were referred to counseling. In a follow-up study, similar individuals with moderate intellectual disabilities will be seen psychiatrically, but then randomly assigned to either supportive counseling or behavior support, or both. They will be followed prospectively, to determine the relative benefits of supportive psychotherapy, behavior support, or a combination, and for what duration of time the treatment should be continued.
Introduction
The purpose of this study was to determine the relative effectiveness at six and 12 months of psychopharmacologic, counseling, and behavioral interventions for a sample of 141 adult patients with mild, moderate, or severe/profound intellectual disability (ID), who had been referred to a dual diagnosis mental health clinic (mental illness and/or behavioral disturbances persons with ID). In addition, the relative frequencies of selected medical disorders among this patient sample were compiled and contrasted with rates in the general population.
The particular clinical population that was chosen for this study was selected because persons with ID often are referred for psychiatric evaluation due to behavioral disturbance, and these behaviors can occur for a number of medical and psychological reasons. One area of concern for the psychiatrist is that behavioral disturbances can be related to undiagnosed medical conditions,[1,2] or to complications or side effects from medications. Appropriate diagnosis and treatment are important, because as medical care for individuals with ID has improved over the years, individuals who have more severe cognitive deficits and who require increased dependency on community supports still have shortened lifespans compared to persons with mild to moderate ID, who are more likely to live to adulthood.[3–6]
Individuals with ID experience the full range of psychiatric disorders at rates higher than the general population.[7] Many psychiatric disorders are misdiagnosed, under-diagnosed, or undiagnosed in this population, often because the ID symptoms overshadow (“diagnostic overshadowing”) other mental health symptoms and the clinician cannot “see” the other aspects of the patient’s presentation. From the limited data available, it appears that depressive disorders and anxiety disorders are under-diagnosed, although psychotic disorders are over-diagnosed. The co-occurrence of ID and mental illness, referred to as a “dual diagnosis,” is common. It is estimated that as many as 30 to 40 percent of persons with ID are dually diagnosed.[7]
Methods
This study is a confidential review of data collected from a consecutive sample of 141 individuals with ID who attended an outpatient clinic over a one-year period, and who had been referred for psychiatric consultation by other clinicians. Data were analyzed by frequency counts, means, standard deviations, chi-square comparisons where appropriate, and one-way analysis of variance (ANOVA) including a repeated-measures analysis for subject weight at beginning and the end of the one-year time period.
The study design was reviewed and approved by a university institutional review board (full review), as well as the superintendent and board of directors of the county board of developmental disability services and by the board of directors of the agency.
All of the individuals in the study were followed over a 12-month period by a psychiatrist and a nurse. Some also had been referred for behavioral support, others were referred for counseling, and some received both. In this initial study, individuals had not been referred to these behavioral treatments on a random basis, but instead on the basis of a needs assessment by the psychiatry service and treatment team. Data were collected on outcomes for these interventions in order to get information about relative effectiveness of the various interventions depending on level of ID and behavioral/emotional symptoms and signs.
Psychiatry medication-somatic program (all patients). Psychiatric diagnoses were made by a board-certified psychiatrist; medical diagnoses were collected from the medical charts and also on the basis of a medical screening by a registered nurse. At the time of intake to the Medication-Somatic Program each subject received the following measures: outpatient nursing assessment, including vital signs, allergies, medication side effects, mood, assessment of thought patterns, orientation, and other physical signs and symptoms; psychiatric diagnostic assessment, including reason for referral, living situation, social information, education, employment and legal history, medical history, previous mental health treatment, current medications, current symptoms and problems, behavioral observations and mental status examination, and diagnoses; Abnormal Involuntary Movement scale (AIMS);[8] list of current medications; and orders for any continued medications or medication changes. Patients were seen monthly or quarterly for 30 minute appointments by the nurse and/or the psychiatrist throughout the period of the study, depending on medical stability.
Behavior support program (by referral). Initial behavioral “problem severity” was rated by the clinic director (master’s level social worker) on the basis of the psychiatric history and available chart material, and ranked accordingly on the Problem Severity Scale.[9] Subjects who received the additional behavioral support were enrolled in a program that assessed and attempted to modify behavior using reinforcement and incentive principles. No aversive interventions were utilized in this program. The identified target behaviors were monitored daily and documented. An individualized design was created for each patient to fit specific needs and symptoms/behaviors.
Supportive psychotherapy program (by referral). Subjects who received supportive psychotherapy were enrolled in a program that provided encouragement, ideas for decreasing mental health symptoms, and increased coping skills/strategies. These subjects were seen once or twice weekly. The main focus of this program was teaching patients better coping skills by using techniques such as better identification of feeling states, management of grief and loss, and coping skills to use when feeling angry or frustrated, as well as assignment to a clinical social worker for supportive psychotherapy.[1]
Results
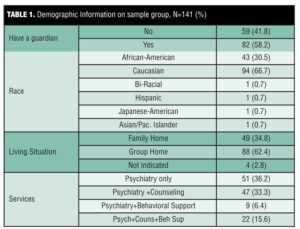
All data analyses were completed using SPSS version 20 and SAS v 9.3. Where appropriate, analyses include one-way ANOVA (weight-change data); chi-square or Fisher’s exact test (medical and psychiatric conditions within intellectual disability group); and Wilcoxin signed rank test (number of medications at beginning and end of study, AIMS scores beginning and end of study for bipolar, anxiety disorder and psychosis subgroups). Demographic information is summarized in Table 1.
Co-occurring medical conditions. An analysis of co-occurring medical conditions among the three ID groups (mild, moderate, severe/profound) revealed the highest frequency of diagnosis of gastroesophageal reflux disease (GERD) among persons diagnosed with mild intellectual disability relative to those with more significant cognitive deficits, which was unexpected. Those with mild ID had a prevalence of 38.1 percent, compared to those with moderate ID (28.6%) or severe/profound ID (28.6%) group (p<0.035, Fisher’s exact test). No statistically significant differences within these ID level subgroups were found in diagnostic frequencies of hyperlipidemia, hypertension, diabetes, family history of diabetes, thyroid disease, or medication allergies. However, when compared to data available on the general United States population, as expected the ID subject population in general had higher rates for most of these disorders (Table 2).
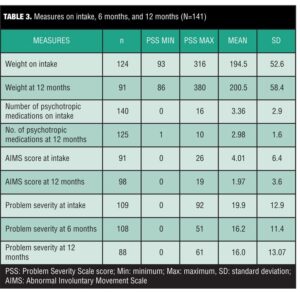
Over the course of the year of study, efforts were made to taper antipsychotic medications to the lowest possible doses and to discontinue the medications when possible. However, AIMS scores trended toward improvement (decreasing from 6.50–3.29) only within the bipolar disorder patient group (p<0.042). Despite efforts to simplify medication regimens that were prescribed and to reduce other side effects besides extrapyramidal symptoms (e.g., weight gain), there were no significant weight changes in either direction over the course of the study, and although the overall number of psychotropic medications decreased from a mean of 3.36 at intake to 2.98 at 12 months, this difference did not reach statistical significance.
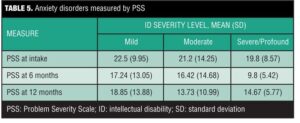
Problem Severity Scale scores (PSS scores). PSS scores are mostly presented by descriptive statistics due to small sample size (Table 4). The PSS scores subjects with anxiety disorders could be analyzed by a two-way repeated measures ANOVA (mild, moderate, severe/profound). Patients with anxiety disorders had a marginally downward trend for PSS scores over time for the moderate ID group (p<0.058, Table 3).
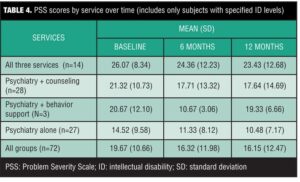
Service groups were defined as psychiatry only; psychiatry + counseling; psychiatry + behavior support; and all three services combined (Table 4). PSS scores for service groups at intake, six months, and 12 months were analyzed by two-way repeated measures ANOVAs, with PSS scores as the outcome. For all time points (at time of intake, 6 months, 12 months), the mean PSS scores for the psychiatry group (including at the outset of the study) were significantly smaller than those for the mean PSS scores for the other groups, reflecting the fact that patients who had displayed more problem behaviors or symptoms at the outset of the study had been assigned additional services (p<0.02 for psychiatry + counseling; p<0.0000 for psychiatry vs. all other service groups).
Length of treatment was significant for all service groups combined, indicating that regardless of starting point, mean PSS scores at the end of the study were significantly smaller than at the beginning, reflecting overall improvement in problem behaviors (mean=19.9 at beginning of study, 16.0 at end of study; p<0.019). The main improvement in PSS scores for all groups was found at the six-month treatment mark (Table 5).
Discussion
Problem severity decreased for all groups combined, and the most improvement was seen at six months. This may be a useful finding, if replicable, since behavior support interventions and counseling commonly are continued for longer durations. It may be more cost-effective to implement these treatments when needed (e.g., death of parent, other significant stressor) for limited periods, rather than as longer-term treatment. Of course, counseling techniques must be modified as suitable for the abilities of the individual patient.[1]
As anticipated, the ID population in this study generally had been diagnosed with a number of serious medical conditions more frequently than is seen in the general population. Although it had been expected that persons with a more severe level of ID would be more frequently diagnosed with serious medical conditions than persons with mild or moderate ID, this was not necessarily true in the current sample, and in fact, GERD was diagnosed more frequently in persons with mild ID. Individuals with mild ID are more likely to be community dwelling and to have more freedom in food options and less ongoing oversight, which may contribute to this finding. In view of the fact that PSS scores decreased with treatment for patients in the anxiety disorders subgroup, in future studies it would be useful to determine if GERD symptoms also decreased with treatment.
Like many persons with ID, these subjects were at an increased risk of having multiple medical problems, and so they often were receiving multiple medications. Although it was possible to simplify their medication regimen to some extent, this did not necessarily always include antipsychotic medication changes and was not necessarily reflected in an overall improvement in AIMS scores (although in some specific instances there was substantial improvement). The positive findings on many of the AIMS scores emphasizes the importance of increasing the use of standardized measurable instruments for assessing for extrapyramidal side effects in those ID patients, especially considering that a number of them may have associated muscular or neurological disorders.
Conclusion
In terms of the intervention strategies that were tried (behavior support and counseling), the results indicated that the first six months of treatment may have been the most effective. This may be important in helping to target services for the most cost-effective use. One important subgroup that needs additional study in terms of the best parameters for effective counseling is the large group of individuals with mild to moderate ID who have trauma histories who present with depression or anxiety symptoms. Expressive language skills are not a necessity,1 but the type of psychotherapy provided will be influenced by the individual’s verbal capabilities. Patients who lack expressive language skills may benefit from techniques that utilize written expression and/or art. Unfortunately, these latter individuals often are overlooked for counseling services because the focus is mainly on their behavior disturbances (which may be efforts to communicate their emotional distress). Paradoxically, one challenge to behavior support intervention alone (in contrast to supportive counseling therapy) is that, since many patients with ID are referred to such treatment by others, the patient may not be as invested in the treatment or have the same goals as the treatment team or referring person. The clinician may unfortunately have to focus on the behavior change and its psychosocial consequences before a good therapeutic alliance has been established.
In a subsequent study, subjects will be limited to those diagnosed with moderate ID and mental health issues who have been referred for treatment and follow-up by the medication-somatic service (psychiatry and nursing) at a community mental health center. As previously, they all will be seen psychiatrically, but then randomly assigned to either supportive counseling or behavior support, or both. They will be followed prospectively, to determine whether there is added benefit in receiving supportive psychotherapy, behavior support, or a combination, and for what duration of time.
References
1. Gentile J, Gillig PM, eds. Psychiatry of Intellectual Disability. West Sussex, England: Wiley Press; 2012.
2. Sutherland G, Murray S, Iacono T. Health issues for adults with developmental disability. Res Dev Disabil. 2002;23:422–445.
3. Chaney RH, Eyman RK. Patterns of mortality over 60 years among persons with mental retardation in a residential facility. Ment Retard. 2000;38:289–293.
4. Hayden MF. Mortality among people with mental retardation living in the United States: research review and policy application. Ment Retard. 1998;36:345–359.
5. Janicki MP, Breitenbach N. Aging and intellectual disabilities – improving longevity and promoting healthy aging: summative report. World Health Organ Tech Rep Ser, Geneva, 2000.
6. Dykins EM, Hodapp RM, Finucane BM. Genetics and mental retardation syndromes: a new look at behavior and interventions. Baltimore, MD: Paul H Brookes Publishing; 2000.
7. Gentile J, Jackson CS. Supportive psychotherapy with the dual diagnosis patient: co-occurring mental illness/intellectual disability. Psychiatry. 2008;5:49–57.
8. Ecdeu GW. Assessment manual for psychopharmacology. Washington, DC: Department of Health, Education and Welfare; 1976.
9. Rojahn J, Matson JC, Lott D, Esbensen A, Smalls Y. The behavior problem inventory: an instrument for the assessment of self-injury, stereotyped behavior and aggression/destruction in individuals with developmental disability. J Autism Dev Disord. 2001;31:577–588.