by Catherine Butz, PhD; Cindy Iske, MS, OTR/L; Natalie Truba, PhD; and Kristen Trott, PhD
Drs. Butz, Truba, and Trott are with the Psychology Department, and Ms. Iske is Program Manager for the Rehabilitation Unit, Physical Medicine and Rehabilitation Service, at Nationwide Children’s Hospital in Columbus, Ohio.
Funding: No funding was provided.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Objective: Conversion disorder has a significant impact on families and the healthcare system. A recent review suggests there is little uniformity in treating this population. This paper describes an inpatient treatment program emphasizing physical conditioning and less time uncovering the psychological underpinnings of the presentation. Design: This study included 100 pediatric patients admitted to an inpatient rehabilitation setting with lower extremity weakness/dysfunction not explained by a medical cause. Patients followed a 16-step goal hierarchy to increase physical function. Patients participated in three hours of therapy and met with a psychologist and teacher daily. Patient functioning was assessed at three time periods using the mobility items of the Functional Independence Measure for Children (WeeFIM). Results: Ninety-four patients completed the program. The average length of stay was 10 days. There were no significant differences between gender, length of stay, or insurance. Data was collected from 73 participants at a two-month follow-up. A repeated measures analysis of variance (ANOVA), using time points at admission, discharge, and follow-up, revealed significant improvements over time. Post-hoc contrasts showed differences with admission and discharge but no differences between discharge and follow-up, suggesting gains in mobility remained. Conclusion: This paper describes an inpatient program that effectively treats patients with conversion disorder in a relatively short period. The physical gains made during hospitalization persisted over time and suggest inpatient rehabilitation focusing on physical mobility could be a more financially beneficial approach than outpatient treatment. Future considerations include identifying a more robust assessment process for patients to determine other psychological characteristics that might impact successful, more short-term treatment.
Keywords: conversion, rehabilitation, mobility, short-term
Innov Clin Neurosci. 2019;16(7–8):18–21
Conversion disorder, defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) as altered voluntary motor or sensory function that cannot be explained by another medical disorder affects less than one percent of the population.1 Early estimates suggest those with functional impairments comprise 20 to 25 percent of inpatient populations.2 Stone et al,3 report referrals for conversion disorder make up a third of neurology clinic visits. Blitzstein4 suggests 5 to 15 percent of psychiatric consultations involve an element of conversion in the patient’s description of symptoms. The variability in these prevalence rates reflect the difficulty in diagnosing this disorder based on vague criteria. However, revisions of the DSM-V offer a more standardized approach to diagnosing this functional neurological syndrome to include impairments of weakness or paralysis in upper or lower extremities, with more complicated examples associated with gait disturbance and abnormality.
Factors leading to a conversion presentation vary. Some studies suggest that emotional conflict, abuse, or trauma might contribute to the cause of nonepileptic seizures.5,6 Recent evidence points to family discord and academic stressors as primary risk factors in youth diagnosed with functional neurological symptom disorder.7 Similarly, Sar et al8 note the most prevalent problems associated with conversion disorder are anxiety and mood symptoms, with ongoing difficulties noted at a one-year follow-up when treated on an outpatient basis. These results suggest a higher level of care might be needed to address these symptoms effectively, especially for the most severe symptoms involving lower extremities numbness and gait abnormalities.
A diagnosis of conversion disorder can have a strong impact on the family and the healthcare system.9 Treatment of this disorder has its roots in psychoanalytic history and has transformed over the years into a more focused approach on improvement of functionality. Emphasis on improvements in mobility in combination with minimal suggestions of feigning symptoms or psychological triggers are recommended.10 Adult studies suggest an emphasis on education of physiology, creating clarity in links between physiology and emotional functioning and focusing treatment on physical therapy (PT).11,12 Studies examining treatment effectiveness in the adult population suggest an inpatient setting could provide the most comprehensive approach to symptoms extinction.13,14 Using a multidisciplinary approach involving PT and occupational therapy (OT), patients with severe motor disturbances have shown improvements in activities of daily living. In addition, sustained improvements after a one-year follow-up suggests intensive treatment to address the physical and psychological aspects of the disorder is necessary.12
While treatment programs for the inpatient setting are emerging as effective for symptom reduction and resolution in adults, evidence within an adolescent population is in the early stages. Most examples are case studies with limited generalizability. In a review of available studies among children, Fitzgerald et al7 concluded that there appears to be little uniformity in treating this patient population. Others have attempted to identify key variables in this patient population that would help to provide a framework for interventions. Kazlowska et al15 suggest that when compared to matched controls, youth with conversion disorder exhibited deficits of attention and executive functioning, supporting the notion of poor cognitive control. As such, suggested interventions include improvements in self-management, acknowledging the impact of underlying stress. Others suggest providing targeted informational fact sheets about the physical presentation to help families understand the functional and somatic aspects of this presentation.16
A treatment approach consistent among published literature is to be nonconfrontational on deficits while providing feedback about physical gains. In addition, most studies suggest there should be focus on improving coping skills, in particular stress management, but have been unable to demonstrate a uniform approach or outcome measure to capture physical gains.9 The present study highlights a structured and systematic approach to treating children and adolescents presenting with gait abnormality. The treatment approach highlights the importance of uniformity among providers, devoting more time to physical conditioning and less time exploring the psychological underpinnings of the presentation. This standardized approach could assist in making this comprehensive approach more cost-effective in the long run.
Methods
Study procedures were consistent with the hospital’s Institutional Review Board guidelines and were considered exempt from the review process.
Increasing evidence supports a physical rehabilitation approach to the treatment of functional gait disturbance. A multidisciplinary approach can more quickly address the physical symptomatology, allowing for youth to return to school and their daily routines sooner. An inpatient program based within a large children’s hospital developed a multidisciplinary intervention that incorporates PT, OT, therapeutic recreational specialists, a school liaison, and psychology. All patients were cared for on the rehabilitation unit, followed by specialized rehab-trained nurses and pediatric physiatrists.
Participants. The participants of this study included 100 children and adolescents who were admitted to the Physical Medicine and Rehabilitation (PM&R) inpatient unit between 2003 and 2017. A preadmission assessment was completed by a PM&R physician and a psychologist. Patients started the program once parents granted consent for participation. Insurance authorization was required prior to admission, with the majority of participants having commercial insurance carriers.
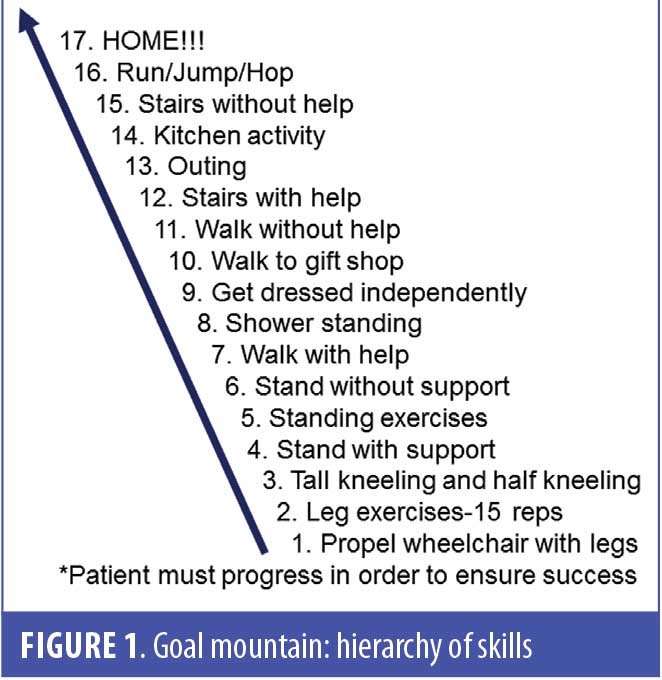
Procedures. Youth admitted to the PM&R unit participated in a structured treatment plan. The goals were organized in an advancing hierarchy of skills to ensure patient success, regardless of their individual level of functioning at the time of admission. The 16-step intervention, referred to as the “Goal Mountain,” identified each goal the patient must complete, in ascending order, prior to discharge.
The Goal Mountain was posted in each patient’s room to ensure patient and family understanding of the expectations, as well as a visual means to track progress. Mastering each step before advancing to higher goals was an essential component to the program, limiting the potential for splintered functional abilities. The daily goal was reinforced during six individual, 30-minute therapy sessions with occupational and physical therapists in addition to sessions with recreational therapy. No adaptive equipment was used once the participant could ambulate safely without a wheelchair. With few exceptions, participants needed to demonstrate mastery of a treatment goal in two consecutive therapy sessions before moving on to the next goal, thus minimizing inconsistencies or a loss of skill (Figure 1).
Additional guidelines were developed to promote success, such as minimizing outside factors that could interfere with treatment. Visitation was limited to the immediate family to promote patient rest. Access to internet, social media, and cell phone use was restricted. Internet usage was limited to reduce exposure to potential triggers (e.g., cyberbullying) that might impede physical recovery. These guidelines helped reduce secondary gain that might come from a hospital stay. Similarly, gifts and outside foods were discouraged, and families were encouraged to celebrate success after discharge rather than reinforce the time in the hospital.
During the hospitalization, participants remained engaged with a hospital-appointed school teacher. This served the dual purpose of reducing the workload from missed school and helping transition to a regular routine. In addition, patients met daily with a member of the psychology team. During these sessions, participants learned adaptive coping and stress management tools through the use of biofeedback, cognitive behavioral therapy skills, and psychoeducation. Psychologists also worked closely with the family to identify and secure, appropriate, outpatient behavioral health services so that intervention could be continued postdischarge to maintain gains.
At discharge, families were provided with instructions to re-engage with academic, physical, and social activities while minimizing attention to re-emerging symptoms. Ongoing use of OT/PT services was strongly discouraged. Rather, families were coached on importance of identifying proactive behaviors of functionality.
Measure. The Functional Independence Measure for Children (WeeFIM) is an 18-item measure used to assess a child’s performance in daily functional skills in three areas: self care, mobility, and cognition. The measure is used in an interview format and with observations to assess children with neurodevelopmental disabilities.17 Data was collected using the WeeFIM at three time points. Premorbid functioning was obtained by asking families to rate their child’s level of functioning prior to onset of symptoms. Rehabilitation therapists rated functioning at admission, when most impaired, discharge, and at two-month follow-up.
Results
Data were collected from 2003 to 2017 to capture the first 100 patients who participated in the program. The average age at admission was 13.39, with a range of 7 to 19 years of age. Seventy-six percent of the population admitted were female. The average length of stay was 10.52 days (standard deviation [SD]=11.68, range 2–103 days). The majority of families (63%) were covered under private insurance, suggesting a higher socioeconomic status for the population. There were no differences observed between length of stay and type of insurance (F=1.138, p<0.215)
Discharge was arranged when the patient resumed optimal functioning, thus achieving the highest score possible on the WeeFIM. Initial analyses revealed that 15 percent of the population did not reach the maximum WeeFIM score at discharge. Further examination revealed the majority of these cases had lower scores because of premorbid levels of cognitive complications, which tend to remain stable despite interventions during admission. Therefore, only mobility scores on the WeeFIM were used to assess for change in functioning. Data from a two-month follow-up were collected for 73 participants.
Ninety-four patients successfully completed the inpatient rehabilitation program. Data from a two-month follow-up were collected for 73 participants. A repeated measures analysis of variance (ANOVA), using time points at admission, discharge, and two-month follow-up, revealed significant changes in overall score achieved (f= 945.07, p<0.001). Post-hoc contrasts showed differences with admission and discharge (p<0.001) but no differences between discharge and follow-up (p=0.45), suggesting that gains in mobility were sustained over time. There were no differences when comparing age, sex, or type of insurance carrier. Of the 100 participants, only five patients, due to various factors, did not complete the program. Two families questioned the fit of the program for their children, and they expressed concerns with the guidelines prior to admission. As a result of this doubt, these families elected to withdraw voluntarily from the program. Another patient had a comorbid diagnosis of autism spectrum disorder (ASD), and cognitive challenges related to this diagnosis interfered with the patient’s success. The final two patients who were unable to complete the program successfully were experiencing significant psychosocial issues, including allegations of abuse and active involvement from Child and Family Protective Services. When comparing the small group of noncompleters, several comorbid diagnoses were detected, including significant mood and behavior issues.
Discussion
Symptoms of conversion disorder can adversely impact the daily functioning and quality of life in youth. Currently, there is limited research investigating interventions that improve functioning in youth with functional gait disturbance. Our study explored the impact an acute inpatient rehabilitation stay can have on improvements in function. Results from our sample are encouraging and highlight the positive impact acute rehabilitation has on motor functioning. This finding has a number of implications. Specifically, the participants in our study gained increased independence, and for many individuals, this resulted in a return to the school setting.
Research confirms that individuals with functional symptoms, including functional gait disorders, access healthcare at increased rates, and it has been estimated that this might account for up to 10 percent of medical costs.18 Additionally, these patients often return to the medical setting seeking information regarding the symptomatology, and as a result, undergo extensive assessments. In many cases, this represents costly, repetitive, and unnecessary assessment, and contributes to increased visits to the urgent care setting, hospital admissions, and lengthy inpatient stays.19,20
In our study, the physical gains made by participants during hospitalization were achieved within a relatively short time frame, and these physical gains were maintained over time. In addition to being a time-efficient intervention to address gait difficulties, this suggests acute inpatient rehabilitation also might be more financially beneficial.
Another significant finding from our study relates to the socioeconomic status of youth with functional neurological symptoms disorders. Historically, literature has suggested conversion disorder is more prevalent in rural populations and individuals with lower socioeconomic status.21 However, our findings suggest there might be a shift in the demographics, specifically among youth with conversion symptoms, because more than half of our population had private insurance.
Limitations. The fact that some families withdrew from the program prematurely, at times because of psychosocial complexities, suggests a limitation in pre-admission assessment. While a physician and a psychologist conducted interviews prior to admission, this study did not use a standardized approach to pre-admission assessment. Similarly, this study used only one measure to determine functional progress, without evaluating changes in emotional functioning as well. Finally, this study took place in a children’s hospital. It is not clear whether this approach is generalizable to adults.
Future Directions
While our preliminary findings are promising, further research is needed to explore the emotional and behavioral functioning and quality of life for youth of this potentially unique patient population. One such area warranting additional research is whether specific maladaptive coping mechanisms contribute to the development and maintenance of functional symptoms. As mentioned in our introduction, Kazlowska et al15 reported that youth with conversion disorder exhibited deficits of attention and executive functioning. This might indicate these youths had poor cognitive control at baseline; however, it might also reflect changes in attentional control that develop through use of maladaptive coping mechanisms. There are multiple benefits to examining the relationship between the functional underpinnings of coping strategies/styles used by this population (e.g., ignoring internal cues of distress, tolerating internal distress resulting in habituation, acceptance of internal experiences) and the development and maintenance of functional neurological symptoms. Exploring this relationship might facilitate clarity regarding whether deficits of attention and executive control are vulnerability factors in the development of functional neurological symptoms, are secondary deficits resulting from use of maladaptive coping strategies, or result from a combination of cognitive vulnerability and maladaptive coping.
Incorporating standardized measures at the time of diagnosis and at follow-up would provide greater insight regarding this patient population, and it could assist with improved identification of specific behavioral health and psychiatric needs. Administering standardized measures among medical teams and clinical therapists throughout a youth’s medical work-up might facilitate improved diagnostic clarity and reduce overall length of inpatient admissions. In turn, this could inform the best treatment approach for each youth and their family. For example, a child with no history of mental health concerns or medical conditions who is diagnosed with functional neurological symptoms might only require a robust psychoeducation program that outlines the conceptualization of functional neurological symptoms and provides basic instruction in use of behavioral principles.
Another area of future direction could involve incorporating current medical technology (e.g., functional magnetic resonance imaging [fMRI]) to improve our theoretical, conceptual, and clinical understanding of functional neurological symptoms. Moving forward, collaborating with physicians and neurobehavioral researchers will be important for improving diagnosis and treatment of conversion disorder. Additionally, involving neuropsychology evaluation tools might afford further insight into these youth’s cognitive functioning, including evaluation of executive functioning, cognitive control, and effort testing, which can provide information on current cognitive and emotional/behavioral functioning. Furthermore, involving neuropsychology could provide additional support related to working with the youth’s school to transition the patient back to regular school routine and behavioral expectations following discharge.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub; 2013.
- Engel G. Conversion symptoms. In: Macbryde C, Blacklow, RS, editor. Signs and Symptoms: Applied Pathologic Physiology and Clinical Interpretation, 5th edition. Philadelphia: Lippincott; 1970. p. 650–658.
- Stone J, Carson A, Duncan R, et al. Who is referred to neurology clinics? The diagnoses made in 3781 new patients. Clin Neurol Neurosurg. 2010;112(9):747–751.
- Blitzstein S. Recognizing and treating conversion disorder. Virtual Mentor. 2008;10(3):158–160.
- Fiszman A, Alves-Leon S, Nunes R, et al. Traumatic events and posttraumatic stress disorder in patients with psychogenic nonepileptic seizures: a critical review. Epilepsy Behav. 2004;5(6):818–825.
- Wood B, Haque S, Weinstock A, Miller B. Pediatric stress-related seizures: conceptualization, evaluation, and treatment of nonepileptic seizures in children and adolescents. Curr Opin Pediatr. 2004;16(5):523–531.
- Dworetzky BA. Psychogenic nonepileptic seizures: children are not miniature adults. Epilepsy Curr. 2015;15(4):174–176.
- Sar V, Akyuz G, Kundakc T, et al. Childhood trauma, dissociation, and psychiatric comorbidity in patients with conversion disorder. Am J Psychiatry. 2004;161(12):2271–2276.
- FitzGerald T, Southby, AK, Haines, TP, et al. Is physiotherapy effective in the management of child and adolescent conversion disorder? A systematic review. J Paediatr Child Health. 2015;51(2):159–167.
- Yakobov E, Jurcik, T, Sullivan, MJ Conversion Disorder. In: Budd M, Hough, S, Wegener, S, Stiers, W editor. Practical Psychology in Medical Rehabilitation: Springer, Cham; 2017, p. 277–285.
- Ali S, Jabeen S, Pate RJ, et al. Conversion disorder—mind versus body: a review. Innov Clin Neurosci. 2015;12(5–6):27–33.
- Jordbru A, Smedstad LM, Klugsøyr O, Martinsen EW. Psychogenic gait disorder: a randomized controlled trial of physical rehabilitation with one-year follow-up. J Rehabil Med. 2014;46(2):181–187.
- McCormack R, Moriarty J, Mellers JD, et al. Specialist inpatient treatment for severe motor conversion disorder: a retrospective comparative study. J Neurol Neurosurg Psychiatry. 2013;85(8):895–900.
- Tsui P, Deptula A, Yuan DY. Conversion disorder, functional neurological symptom disorder, and chronic pain: comorbidity, assessment, and treatment. Curr Pain Headache Rep. 2017;21(6):1–10.
- Kozlowska K, Palmer DM, Brown KJ, et al. Conversion disorder in children and adolescents: a disorder of cognitive control. J Neuropsychol. 2015;9(1):87–108.
- Cruz C, Chudleigh C, Savage B, Kozlowska K. Therapeutic use of fact sheets in family therapy with children and adolescents with functional somatic symptoms. Aust N Z J Fam Ther. 2014;35(3):223–243.
- Msall M, DiGaudio K, Duffy LC, et al. WeeFIM: normative sample of an instrument for tracking functional independence in children. Clin Pediatr. 1994;33(7):431–438.
- Anderson K, Gruber-Baldini AL, Vaughan CG, et al. Impact of psychogenic movement disorders versus Parkinson’s on disability, quality of life, and psychopathology. Mov Disord. 2007;22(15):2204–2209.
- Cardozo A, Rubiano MA, Garces G, et al. Conversion disorder in a neurological emergency department: retrospective series. Journal of Acute Disease. 2017;6(5):218–221.
- Adjei M, Coebergh JA. An audit of the diagnosis and costs associated with inpatients with functional neurological symptoms in a district general hospital. J Neurol Neurosurg Psychiatry. 2014;85(2):220–226.
- Deka K, Chaudhury PK, Bora K, Kalita P. A study of clinical correlates and socio-demographic profile in conversion disorder. Indian J Psychiatry. 2007;49(3):205.





