by Ryan Bart, DO; Waguih William IsHak, MD, FAPA; Shaina Ganjian, MS; Karim Yahia Jaffer; Marina Abdelmesseh, MD, CIC; Sophia Hanna, BA; Yasmine Gohar, BA; Gezelle Azar, Bs; Brigitte Vanle, PhD; Jonathan Dang, MD; and Itai Danovitch, MD
Dr. Bart is with Western University of Health Sciences and Cedars-Sinai Medical Center, in Los Angeles, California. Drs. IsHak, Abdelmesseh, Vanle, Dang, and Danovitch and Mses. Ganjian, Abdelmesseh, and Gohar are with the Cedars-Sinai Medical Center, in Los Angeles, California. Mr. Jaffer is a medical student at Faculty of Medicine Cairo University in Cairo, Egypt and Cedars-Sinai Medical Center, in Los Angeles, California. Ms. Hanna is with California State University Long Beach, in Long Beach, California. Ms. Azar is with Loma Linda University in Loma Linda, California.
Funding: No funding was provided.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Innov Clin Neurosci. 2018;15(9–10):14–23
Abstract: We conducted a systematic review of the published literature relating to the assessment and measurement of wellness in order to answer the following questions: 1) What is the working definition of wellness? 2) What wellness assessment instruments have been evaluated or applied in medical settings? 3) How valid, reliable, and accessible are these wellness assessment tools? The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed for this systematic review. Studies published from1990 to 2016 on wellness assessment were identified through Medline and PsycINFO using the following keywords: “assessment” OR “evaluation” OR “measurement” AND “wellness” OR “wellbeing.” Two authors independently conducted a focused analysis then reached a consensus on 23 studies that met the specific selection criteria. This review revealed that there is a lack of uniform definition of wellness. The studies utilizing wellness assessment tools demonstrate strongest reliability values for the following instruments: Wellness Evaluation of Lifestyle, Five-factor Wellness Evaluation of Lifestyle, Perceived Wellness Survey, the Optimal Living Profile, and the Body-Mind-Spirit Wellness Behavior and Characteristic Inventory. However, there is insufficient evidence to support the clinical utility of a single particular wellness instrument. Properly defining wellness might help drive the development and validation of more precise assessment and measurement methods. This could reinforce interventions that promote wellness.
Keywords: Assessment, evaluation, measurement, wellness, wellbeing, instruments
Most people are interested in achieving optimal health; however, the medical field has been criticized for disproportionately focusing on the elimination of disease rather than the promotion of health in recent years.1 Over the last decade, healthcare professionals have begun to shift their approach to be more aligned with patient preferences by routinely guiding people to healthier lifestyle choices by improving wellness.2 Currently, two concepts have persisted: the emphasis on the multidimensional nature of wellness and the categorization of self-perceived wellness into at least three broad dimensions—the physical, mental, and social.3
In 1964, The World Health Organization (WHO) defined health as a state of physical, mental, and social well-being, not merely the absence of disease.4 Since its conception, the definition of wellness has continued to change.3 However, to better understand wellness, it is crucial to first understand what it is not.
First, wellness is different than health. Whereas the term health focuses on illness status and the individual’s relationship to that status, wellness transcends the absence of disease.5 Furthermore, wellness is different from wellbeing. Wellbeing can be described as the balance-point between an individual’s resources and the challenges he or she faces.3 Although wellbeing is a step toward wellness, it is not necessarily as encompassing as wellness. It is possible for someone to be in a state of wellbeing but not wellness; depletion of adequate resources (psychological, social, and/or physical) can prevent one from attaining wellness.3 Additionally, wellness should not be confused with quality of life (QOL), which involves an individual’s subjective perspective of his or her health and function in physical, psychological, social, and cognitive domains.6 QOL is a measure of a patient’s subjective evaluation of health and life aspects despite a given diagnosis, whereas according to the WHO, wellness involves more than the absence of disease, implying that absence of disease is one of the requirements for wellness. With these definitions in mind, we can understand wellness as an evolving process toward achieving one’s full potential; it is positive/affirming and holistic, and encompasses lifestyle, spiritual, and environment wellbeing domains. Wellness also accounts for the physical, mental, and social domains implied in health, and thus health is dependent on sufficient wellness.7 By better understanding wellness, physicians and patients can work together better to best treat the needs of the patient.
The importance of comprehensive wellness assessment in regular clinical practice cannot be overemphasized.8 The use of standardized wellness measurement instruments in primary care settings could improve preventive services, behavioral health outcomes, and overall patient care. Additionally, it allows for longitudinal tracking of overall patient health and extrapolation of long-term health outcomes.9
This systematic review of the published literature relating to the assessment and measurement of wellness was performed to identify areas where future studies are needed to move the field forward by addressing the following questions: 1) What is the working definition of wellness? 2) What wellness assessment instruments have been evaluated or applied in medical settings? 3) How valid, reliable, and accessible are these wellness assessment tools?
Methods
Search strategy. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for this review.10 A systematic literature search was conducted on articles listed in the PubMed and PsycINFO databases from January 1990 to February 2016 after setting exclusion and inclusion criteria. The keywords used for the search were assessment OR evaluation OR measurement AND wellness OR wellbeing. We also conducted a manual search of reference lists of identified papers and previous reviews of wellness assessment.
Study selection criteria and methodology. The following inclusion criteria were used: 1) articles that were in English or had an available published English translation; 2) articles that were previously published in a peer-reviewed journal; 3) studies of any design that focused on the assessment of wellness; and 4) studies that used at least one wellness assessment measure. Exclusion criteria included editorials, opinion pieces, and case reports. Two authors independently conducted a focused analysis then reached a consensus on studies that met the specific selection criteria.
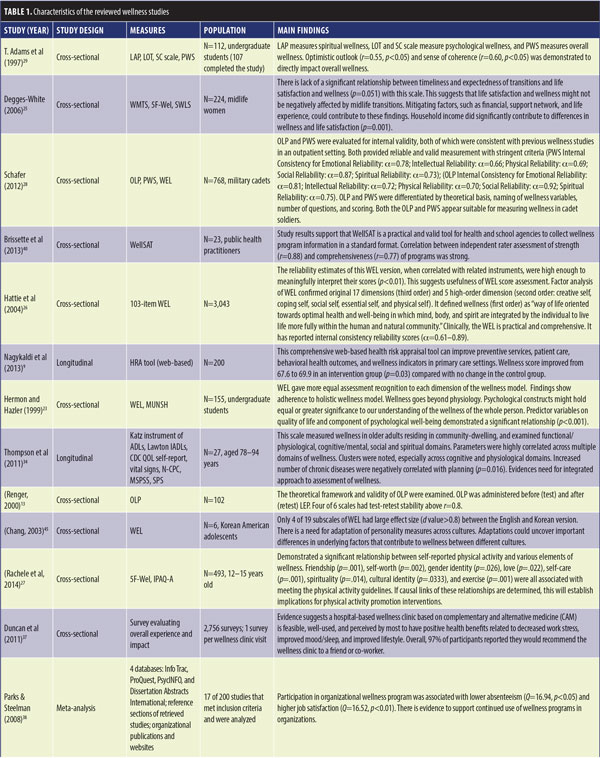
Data extraction and yield. Key findings were derived from the full text and tables of the selected studies. Study design and findings were analyzed for quality and detailed in Tables 1 and 2.
Results
Our search strategy identified 3,654 relevant articles. After reviewing the abstracts of 3,654 studies, irrelevant studies were excluded, leaving 51 studies. Two authors independently conducted a focused analysis using the gathered 51 full-text articles. The two authors then reached a consensus on the studies to include in this review, which yielded 23 studies. The findings from the reviewed studies are displayed in Table 1.
1. What is the working definition of wellness? The WHO’s original definition of health provided the foundation for defining wellness by emphasizing the three dimensions wellness comprises: physical, mental, and social health.11 These dimensions highlight that wellness not only comprises individual aspects but is an integrated whole.12 Wellness results from a balance of the dimensions, allowing an individual to cope with life circumstances and to achieve an optimal state of being.13 Thus, an operational definition of wellness emphasizes lifestyle behaviors that go beyond basic health into optimal states across multiple dimensions.14
In 1998, the Wheel of Wellness (WoW), a theoretical framework to better understand the concept of wellness, was developed.15 This widely used framework defined wellness as a “way of life oriented towards optimal health and well-being in which mind, body, and spirit are integrated by the individual to live life more fully within the human and natural community.”16 In 2004, the WHO Health Promotion Unit in Geneva, Switzerland, updated the definition of wellness in the Health Promotion Glossary as, “the optimal state of health of individuals and groups. There are two focal concerns: the realization of the fullest potential of an individual physically, psychologically, socially, spiritually, and economically, and the fulfillment of one’s role expectations in the family, community, place of worship, workplace, and other settings.”17 To properly assess wellness, comprehensive measurement methods that accurately identify and evaluate these various dimensions are necessary. However, the layered multidimensionality that is intrinsic to the concept of wellness has created roadblocks in developing a gold standard definition and has contributed to the disparities in evaluating wellness.3 Others assert that wellness is often considered the endpoint of physical, mental, or social interventions.
2. What are the current wellness assessment instruments that can be applied in a clinical medical setting?
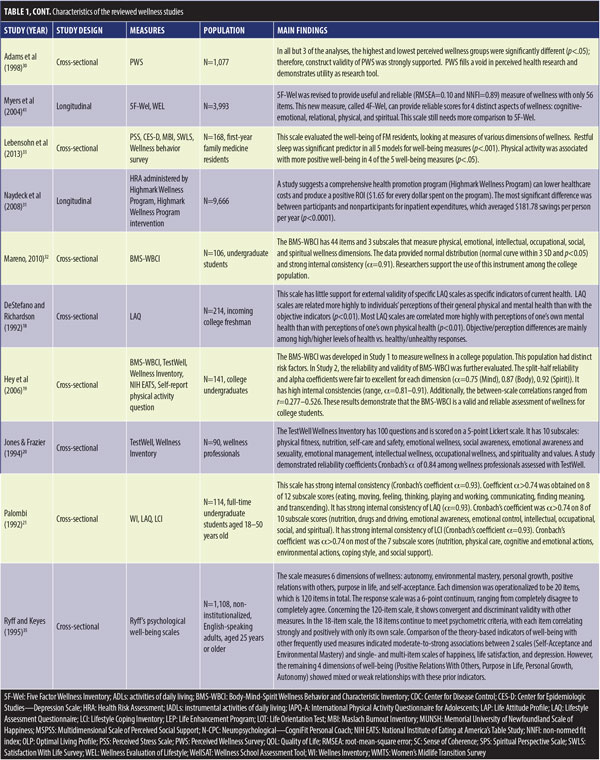
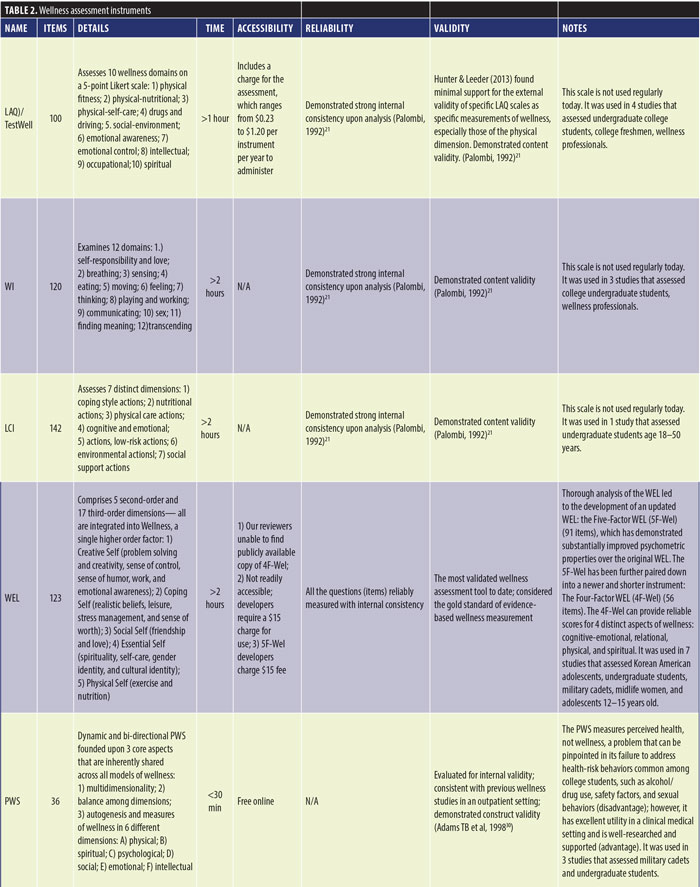
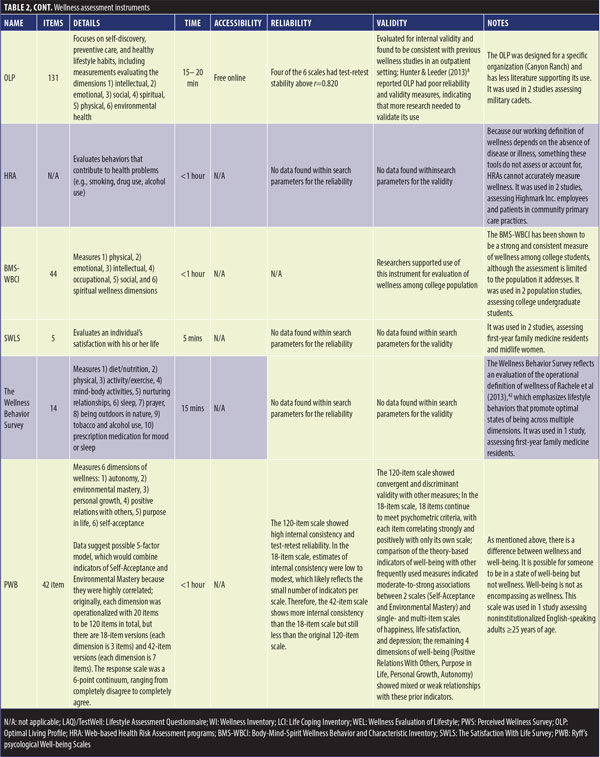
Wellness assessment instruments. Data collected about wellness assessment instruments can be found in Table 2.
Lifestyle Assessment Questionnaire (LAQ). One of earliest wellness assessments created for clinical use was the LAQ, also known as the TestWell Wellness Inventory.18 Established by the National Wellness Institute in 1983, the LAQ is a 100-item questionnaire assessing 10 wellness domains on a five-point Likert scale. The 10 domains include physical fitness, physical–nutritional, physical–self-care, drugs and driving, social-environment, emotional awareness, emotional control, intellectual, occupational, and spiritual. The LAQ was used in four of the reviewed studies to assess wellness in college undergraduates, in college freshmen, and in wellness professionals.18–21
Wellness Inventory (WI). The second tool from the 1980s was the WI,19 which contains 120 questions examining 12 domains: self-responsibility and love, breathing, sensing, eating, moving, feeling, thinking, playing and working, communicating, sex, finding meaning, and transcending. The WI was used in three of the reviewed studies to assess wellness in undergraduate students and in wellness professionals.19–22
Life Coping Inventory (LCI). The third tool from the 1980s was the LCI,21 which examines coping-related behaviors with 142 questions that assess seven distinct dimensions: coping style actions, nutritional actions, physical care actions, cognitive and emotional actions, low-risk actions, environmental actions, social support actions. The LCI was used in one of the reviewed studies to assess wellness in undergraduate students.21
Wellness Evaluation of Lifestyle (WEL). Developed from the theoretical framework of the WoW model, the WEL assessment tool was created in 2000.16 The WEL is a comprehensive tool for assessing wellness and prevention over an individual’s lifespan.2,15 The WEL comprises five second-order and 17 third-order dimensions, which are all integrated into wellness: a single higher-order factor. The second order dimensions include 1) creative self (problem-solving and creativity, feelings of control, sense of humor, work, and emotional awareness); 2) coping self (realistic beliefs, leisure, stress management, and sense of worth); 3) social self (friendship and love); 4) essential self (spirituality, self-care, gender identity, and cultural identity); and 5) physical self (exercise and nutrition). The WEL has been reported to recognize each dimension of the WoW model and has even been called the gold standard of wellness assessments.2,23
Five-factor WEL (5F-Wel) and Four-factor WEL (4F-Wel). The thorough WEL analysis led to the development of an updated WEL: the 5F-Wel,24 which has demonstrated significantly improved validity and reliability compared to the WEL.24 The 5F-Wel was further pared into a newer and shorter instrument: the 4F-Wel.25 The 4F-Wel provides reliable scores for four distinct aspects of wellness: 1) cognitive-emotional, 2) relational, 3) physical, and 4) spiritual. The 4F-Wel emerged after the 5F-Wel statistically failed to demonstrate consistent relationships between the 17 scales reported in the WEL. Additionally, the 4F-Wel is the shortest assessment instrument for explaining a given wellness dimension (the WEL and 5F-Wel are both lengthy with 123 items and 91 items, respectively).3,24 The WEL was used in seven of the reviewed studies to assess wellness in Korean-American adolescents, in undergraduate students, in military cadets, in midlife women, and in adolescents of age 12 to 15.23,25–28
Perceived Wellness Survey (PWS). The PWS assessment tool evaluates overall wellness.29 The dynamic and bi-directional PWS is founded upon three core aspects that are shared across all models of wellness. These three core aspects are 1) multidimensionality, 2) balance among dimensions, and 3) measures of wellness in six dimensions.30 However, the PWS measures perceived health, not wellness. While it is not the best at detecting health-risk behaviors common among college students, such as alcohol/drug use, safety factors, or sexual behaviors, its focus on health perceptions makes it a unique tool.19 The PWS was used in three of the reviewed studies to assess wellness in military cadets and in undergraduate students.28–30
The Optimal Living Profile (OLP). Although wellness assessments could be valuable in clinical settings to help healthcare professionals understand their patients, many tools were developed specifically for scientific studies on wellness. The OLP was used in two studies to evaluate wellness.31 This assessment tool focuses on self-discovery, preventive care, and healthy lifestyle habits and includes measurements that evaluate the dimensions of intellectual, emotional, social, spiritual, physical, and environmental health.2 The OLP was used in two reviewed studies to assess wellness in military cadets.28,31
Web-based health risk assessment (HRA) tool. Two different studies used the HRA tool, which assessed wellness via behaviors contributing to health problems, such as smoking and drug and alcohol use. The HRA tool was used in two of the reviewed studies to assess wellness among insurance company employees and in patients of a community primary care practice.9,31
The Body-Mind-Spirit Wellness Behavior and Characteristic Inventory (BMS-WBCI). The BMS-WBCI was developed in a two-study project conducted in 2006 as a wellness evaluation instrument for college students.19,32 This inventory measures 1) physical, 2) emotional, 3) intellectual, 4) occupational, 5) social, and 6) spiritual dimensions and has been shown to be a consistent measure of wellness.19,32 The BMS-WBCI was used in two of the reviewed studies to assess wellness in college undergraduate students.19,32
The Satisfaction with Life Survey (SWLS) and the Wellness Behavior Survey (WBS). The SWLS and WBS were utilized to evaluate wellness in first-year family medicine residents.33 The SWLS has five items to evaluate an individual’s satisfaction with his or her life, while the WLS has 14 items evaluating 1) diet/nutrition, 2) physical activity/exercise, 3) mind-body activities, 4) nurturing relationships, 5) sleep, 6) prayer, 7) being outdoors in nature, 8) tobacco and alcohol use, and 9) prescription medication for mood or sleep. The study also included scales for stress, depression, and burnout for the individual’s overall evaluation of wellness. The SWLS was used in two of the reviewed studies to assess wellness in first-year family medicine residents and in midlife women.25,33 The WBS emphasizes lifestyle behaviors that promote optimal states of being across multiple dimensions. The WBS was used in one reviewed study to assess wellness in first-year family medicine residents.33 In a study of older adults living in a community dwelling, wellness was evaluated using a variety of self-report tools focusing on the individual’s ability to carry out activities of daily living (ADLs).34
Ryff’s Psychological Well-being (PWB) scales. PWB scales measure six dimensions of wellness: 1) autonomy, 2) environmental mastery, 3) personal growth, 4) positive relations with others, 5) purpose in life, and 6) self-acceptance. Data, not theory, suggested a possible five-factor model, which would combine indicators of self-acceptance and environmental mastery because they were highly correlated. Initially, each dimension was operationalized with a 20-item scale to be 120 items in total but there are two shorter versions, an 18-item version (each dimension is 3 items) and a 42-item version (each dimension is 7 items). The response scale was a six-point continuum, ranging from “completely disagree” to “completely agree.”35 PWB scales were used in one of the reviewed study to assess wellness in noninstitutionalized English-speaking adults aged 25 years or older.35
Medical setting application. The following instruments have been implemented in medical settings: WEL, 5F-Wel, PWS, OLP, and the BMS-WBCI. However, when instruments measure multiple dimensions of wellness, completion of the instruments is time-consuming for the participants and administrators. The WEL and the 5F-Wel have 123 and 91 items, respectively. The WEL scoring ranges from 20 to 100, while the 5F-WEL ranges from 25 to 100, with higher scores indicating greater wellness.24 It would not be time efficient to administer these tests in a clinical medical setting because they take over two hours to complete. However, the 4F-Wel has only 56 items and still accurately measures the core WoW dimensions. The 4F-Wel provides a promising potential for clinical medical use, but our reviewers were unable to find a publicly available copy of the 4F-Wel. Although the 4F-Wel is a more time-efficient assessment tool, the lack of public availability creates an obstacle to its widespread implementation in medical settings. The developers of this assessment tool also asserted that more research is needed to validate the instrument further.
Both the OLP and PWS were consistent with previous wellness studies in an outpatient setting.2 Because of its brevity (36 items) and accessibility (free online), the PWS has excellent utility in a clinical medical setting, takes less than 30 minutes to administer, and is well-researched and supported. The PWS scores range from three to 29, with higher scores indicating greater perceived wellness. While the OLP takes 15 to 20 minutes to complete electronically, it was designed for a particular organization (Canyon Ranch) and has less literature supporting its use.28 However, its developers assert that the OLP is readily comprehensible and presents an accessible self-report format that makes it convenient for use in primary care settings.31 After careful component analysis, both the OLP and the PWS appear suitable for measuring wellness in Cadet soldiers.2
The BMS-WBCI has 44 items, with scores ranging from 44 to 132. Scores below 74 indicate the need for immediate change in behavior, scores above 103 indicate that a wellness lifestyle exists, and scores from 74 to 103 indicate that behavior change is needed in certain areas. The BMS-WBCI is short and easy to administer, and it focuses on assessing the frequency of positive health behaviors, making it a useful assessment tool to identify health-risk behaviors and create improvement goals.9
3. How valid, reliable, and accessible, are these wellness assessment instruments? Validity and reliability. The WEL is one of the oldest and most validated wellness assessment tools to date and is considered the gold standard of evidence-based wellness measurement.2,36 The WEL measures the 17 domains found in the framework of the WoW through 123 questions, all of which have reliability with internal consistency (alpha scores ranging from 0.61–0.89 across all domains).26 The WEL is not readily accessible because its developers require a $15 charge for its use.
The 5F-Wel is an updated version of the WEL.16 There is still the required fee of $15 for its use, the 5F-Wel has only 91 questions and has been found to be valid and reliable. 5F-Wel has since been revised to the 4F-Wel, providing useful and reliable (RMSEA=0.10 and NNFI=0.89) measure of wellness with only 56 items; however, it does not appear to be available to the public.
The LAQ, also known as TestWell, was more widely used in the 1990s and measures wellness across multiple dimensions.9 It is cumbersome to complete, as it has 100 items, and includes a charge for the assessment, which ranges from $0.23–1.20 per instrument per year to administer. Additionally, Hunter & Leeder found minimal support for the external validity of particular LAQ scales as precise measurements of wellness, especially those of the physical dimension.8 Related to the same time era of LAQ are the WI and the LCI. Both the WI and LCI have demonstrated strong internal consistency and content validity upon analysis, as did the LAQ (Cronbach’s coefficient ?=0.93 and ?=0.84, respectively).20,21 After careful review of the literature, neither of these instruments appear to be regularly used today.
The PWS was evaluated for internal validity and was consistent with previous wellness studies in an outpatient setting.2 The PWS offers a reliable and valid assessment instrument of 36 items while maintaining stringent criteria. The PWS has free online access. The construct validity of the PWS is strongly supported.30
The OLP consists of 131 electronic items and is free of charge.2 Four of the six scales had test-retest stability above r=0.820. The OLP was evaluated for internal validity and was found to be consistent with previous wellness studies in an outpatient setting.2 However, Hunter & Leeder reported that the OLP had poor reliability and validity measures, indicating that more research is needed to validate the use of OLP.8
The BMS-WBCI is a relatively new 44-item assessment that consists of three subscales focused on evaluating wellness in the college student population. In the first study focusing on the development of the BMS-WBCI, the following alpha scores measured: mind (?=0.88), body (?=0.81), and spirit (?=0.91).9 In the same article, Hey et al9 conducted a second study and found the following alpha values: mind (?=0.75), body (?=0.87), and spirit (?=0.92). Data obtained from the BMS-WBCI provided a normal distribution (standard curve within 3 SD and p<.05) and strong internal consistency (?=0.91).32 The researchers supported the use of this instrument for among college populations.
The Ryff’s PWB scale has many versions (e.g., 120-item scale, 42-item scale, and 18-item scale). The 120-item scale has shown high internal consistency and test-retest reliability, while the 18-item scale estimates of consistency have been measured at low to modest. This modest internal consistency likely reflects the small number of indicators per scale. Therefore, the 42-item scale shows more internal consistency than the 18-item scale but still less than the original one (120-item scale). Regarding validity, for the 120-item scale, it shows convergent and discriminant validity with other measures. In the 18-item scale, all 18 items continue to meet psychometric criteria. Comparison of the theory-based indicators of well-being (Ryff’s PWB scales) with other frequently used measures indicate moderate to strong associations between two scales (self-acceptance and environmental mastery) and single- and multi-item scales of happiness, life satisfaction, and depression. Moreover, the remaining four dimensions of well-being (positive relations with others, purpose in life, personal growth, and autonomy) showed mixed or weak relationships with these prior indicators.18
No data were found within our search parameters for the validity and reliability of the SWLS, WBS, or the HRA tool.
Accessibility/implementation. A successful wellness intervention hinges upon effective measurement of wellness before and after the intervention. Such programs have the goal of empowering others toward self-care and personal control over health and wellness.
One study found that a hospital-based wellness clinic is feasible, well-used, and perceived by most to have positive health benefits. 37 These health benefits include decreased work stress, improved mood/sleep, and an overall improved lifestyle. After visiting the hospital-based wellness clinic, 97 percent of participants (n=2,756) reported that they would advise a friend or coworker to visit the clinic for consultation and treatment. Such programs could significantly improve health status and cause a shift toward a state of wellness.9 Another study found that employees who participated in an organizational wellness program showed less job absenteeism and greater job satisfaction.38 Wellness intervention programs also benefit the economics of the organization.31 Another study demonstrated that a comprehensive health promotion program (Highmark Wellness) significantly lowered healthcare costs and produced a positive return on investment (ROI) ($1.65 for every dollar spent on the program).18 Wellness program participants averaged annual savings of $181.78 per person, in comparison to nonparticipants (p<.0001). These examples provide emerging evidence in support of the feasibility of wellness instruments and wellness program interventions in the health care and organizational setting.18,27,39–44
Discussion
The reviewed studies of wellness assessment tools demonstrate strong reliability values for the following instruments: WEL, 5F-Wel, PWS, OLP, and the BMS-WBCI. However, the evidence is insufficient to assert a specific instrument’s use in clinical practice. As effective as wellness interventions might seem, without effectual assessment tools to measure wellness, clinicians and researchers are left to deduce effects of treatment from secondary measurements and subjective appraisal. The use of an accurate wellness tool would likely assist clinicians in better understanding which treatment approach would achieve the greatest health benefits for each individual patient. Additionally, the proprietary nature of many of these assessments could be a significant barrier to regular use and presents another limitation to feasibility and implementation.
This review revealed that descriptions of wellness vary, and the term lacks a singular definition. It is important to establish a clear definition to minimize variability when assessing for wellness. It is essential for this working definition to include specific dimensions that can be measured in the clinical setting. Among the wellness definitions, the WHO’s 2004 definition conceptualizes wellness best as the optimal state of health for individuals and groups, not merely the absence of disease or infirmity, with two focal concerns: 1) the realization of the fullest potential of an individual physically, psychologically, socially, spiritually, and economically and 2) the fulfillment of each individual’s role expectations in the family, community, place of worship, workplace, and other settings.
Limitations. By limiting this review to English papers and assessments, our review might have limited applicability in international and/or non-English speaking cultures. Furthermore, the data available on wellness assessments are relatively lacking, with the notable absence of well-controlled, longitudinal wellness research studies. Finally, because the definitions underpinning wellness assessments are in constant flux, the accuracy of these assessments can shift as the definition of wellness evolves.
Conclusion
Through a systematic review of published literature, we sought to explore wellness definitions, the clinical utilization of varied wellness assessment instruments, and the validity, reliability, and accessibility of these instruments in the assessment of wellness. Our review reveals the need among the medical community to develop a consensus on defining wellness to complement emphasis on treating and preventing disease with health promotion. Such a consensus could, in turn, drive the development and validation of more precise wellness assessment and measurement methods. Although wellness can be assessed using the currently available tools, as described in this article, there is room for improvement and for creation of a more accurate, shorter, and more encompassing assessment. The current assessments are based only on our current definition of wellness, so longitudinal studies tracking the different aspects of wellness and their implications over time are necessary. We hope that this review encourages more research on wellness assessment tools and assists clinicians and researchers in accessing to the wellness assessments tools most suitable for their needs and the needs of their patients.
References
- Naci H, Ioannidis J. Evaluation of wellness determinants and interventions by citizen scientists. JAMA. 2015;314(2):121–122.
- Polak R, Pojednic R, Phillips E. Lifestyle medicine education. Am J Lifestyle Med. 2015;9(5):361–367.
- Rachele J, Cockshaw W, Brymer E. Towards an operational understanding of wellness. JSLaM. 2013;7(1):3–12.
- Constitution of the World Health Organization Annex. Updated October 2006. http://www.who.int/governance/eb/who_constitution_en.pdf. Accessed 1 Oct 2018.
- Breslow L. A quantitative approach to the World Health Organization definition of health: physical, mental and social well-being. Int J Epidemiol. 1972;1(4):347–355.
- The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41(10):1403–1409.
- Hetler B. The six dimensions of wellness model. National Wellness Institute (site). https://cdn.ymaws.com/www.nationalwellness.org/resource/resmgr/pdfs/sixdimensionsfactsheet.pdf. Accessed 1 Oct 2018.
- Hunter J, Leeder S. Patient questionnaires for use in the integrative medicine primary care setting—a systematic literature review. Eur J Integr Med. 2013;5(3):194–216.
- Nagykaldi Z, Voncken-Brewster V, Aspy C, Mold, J. Novel computerized health risk appraisal may improve longitudinal health and wellness in primary care: a pilot study. Appl Clinic Inform. 2013;4(1):75–87.
- Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012.
- World Health Organization Constitution. 1949. https://www.loc.gov/law/help/us-treaties/bevans/m-ust000004-0119.pdf. Accessed 1 Oct 2018.
- Saxena S, Orley J. Quality of life assessment: the World Health Organization perspective. Eur Psychiatry. 1997;12(3):263s–266s.
- Renger R, Soto, M, Erin T, et al. Optimal living profile: an inventory to assess health and wellness. Am J Health Behav. 2000;24(6):403–412.
- Nobile M. The WHO definition of health: a critical reading. Med Law. 2014;33(2):33–40.
- Witmer JM, Sweeney TJ, Myers JE. The Wheel of Wellness. Greensboro, NC: Authors;1988:10.
- Myers J, Sweeney T, Witmer J. The wheel of wellness counseling for wellness: a holistic model for treatment planning. J Couns Dev. 2000;78(3):251–266.
- Smith B, Tang K, Nutbeam D. WHO health promotion glossary: new terms. Health Promot Int. 2006;21(4):340–345.
- DeStefano T, Richardson P. The relationship of paper-and-pencil wellness measures to objective physiological indexes. J Couns Dev. 1992;71(2):226–230.
- Hey W, Calderon K, Carroll H. Use of body-mind-spirit dimensions for the development of a wellness behavior and characteristic inventory for college students. Health Promot Pract. 2006;7(1):125–133.
- Jones J, Frazier S. Assessment of self-esteem and wellness in health promotion professionals. Psychol Rep. 1994;75(2):833–834.
- Palombi B. Psychometric properties of wellness instruments. J Couns Dev. 1992;71(2):221–225.
- Houts P, Doak C, Doak L, Loscalzo M. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61(2):173–190.
- Hermon D, Hazler R. Adherence to a wellness model and perceptions of psychological well-being. J Couns Dev. 1999;77(3):339–343.
- Myers J. The indivisible self: an evidence-based model of wellness. J Individ Psychol. 2004;60(3):234–245.
- Degges-White S. Transitions, wellness, and life satisfaction: implications for counseling midlife women. J Ment Health Couns. 2006;28:133–150.
- Myers HJ, Sweeney T. A factor structure of wellness: theory, assessment, analysis, and practice. J Couns Dev. 2004;82(3):354–364.
- Rachele J, Cuddihy T, Washington T, McPhail S. The association between adolescent self-reported physical activity and wellness: the missing piece for youth wellness programs. J Adolesc Health. 2014;55(2):281–286.
- Schafer M. Assessing Soldiers’ Wellness Holistically: An Evaluation of Instruments Applicable to Primary Care [dissertation]. Tuscon: University of Arizona; 2012.
- Adams T, Bezner J, Steinhardt M. The conceptualization and measurement of perceived wellness: integrating balance across and within dimensions. Am J Health Promot. 1997;11(3):
208–218. - Adams T, Garner L, Woodruff S. Construct validation of the perceived wellness survey. Am J Health Stud. 1998;14(4):212–219.
- Naydeck B, Pearson J, Ozminkowski R, et al. The impact of the highmark employee wellness programs on 4-year healthcare costs. J Occup Environ Med. 2008;50(2):146–156.
- Mareno N. Further validation of the body-mind-spirit wellness behavior and characteristic inventory for college students. South Online J Nurs Res. 2010;10(4).
- Lebensohn P, Dodds S, Benn R, et al. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. 2013;45(8):541–549.
- Thompson H, Demiris G, Rue T, et al. A holistic approach to assess older adults’ wellness using e-health technologies. Telemed J E Health. 2011;17(10):794–800.
- Ryff C, Keyes C. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–727.
- Myers J, Truluck M. Health beliefs, religious values, and the counseling process: a comparison of counselors and other mental health professionals. Couns Values. 1998;42(2):106–123.
- Duncan A, Liechty J, Miller C, et al. Employee use and perceived benefit of a complementary and alternative medicine wellness clinic at a major military hospital: evaluation of a pilot program. J Altern Complement Med. 2011;17(9):809–815.
- Parks K, Steelman L. Organizational wellness programs: a meta-analysis. J Occup Health Psychol. 2008;13(1):58–68.
- Adams T, Bezner J, Drabbs M, et al. Conceptualization and measurement of the spiritual and psychological dimensions of wellness in a college population. J Am Coll Health. 2000;48(4):165–173.
- Brissette I, Wales K, O’Connell M. Evaluating the Wellness School Assessment Tool for use in public health practice to improve school nutrition and physical education policies in New York. J Sch Health. 2013;83(11):757–762.
- Myers J, Luecht R, Sweeney T. The factor structure of wellness: reexamining theoretical and empirical models underlying the Wellness Evaluation of Lifestyle (WEL) and the Five-Factor Wei. Meas Eval Couns Dev. 2004;36(4):194–208.
- Rachele J, Cuddihy T, Barwais F, McPhail S. Valid and reliable assessment of wellness among adolescents: Do you know what you’re measuring?. Int J Wellbeing. 2013;162–172.
- Roscoe L. Wellness: a review of theory and measurement for counselors. J Couns Dev. 2009;87:216–226.
- Wallace J, Lemaire J, Ghali W. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–1721.
- Chang C. Cultural adaptation of the Wellness Evaluation of Lifestyle (WEL): An assessment challenge. Meas Eval Couns Dev. 2003;35(4):239–250.





