 by Ashok Baral, MBBS; Rajan Gyawali, MBBS; Dikshya Upreti, MBBS; Atindra Mishra, MD; and Anoop Krishna Gupta, MD
by Ashok Baral, MBBS; Rajan Gyawali, MBBS; Dikshya Upreti, MBBS; Atindra Mishra, MD; and Anoop Krishna Gupta, MD
Ashok Baral, Rajan Gyawali, Dr. Upreti, and Dr. Gupta are with the Department of Psychiatry at the National Medical College in Birgunj 44300, Nepal. Dr. Mishra is with the Department of Pediatrics at the National Medical College in Birgunj 44300, Nepal.
FUNDING: No funding was provided for this study.
DISCLOSURES: The author has no conflicts of interest relevant to the content of this article.
ABSTRACT: Acute disseminated encephalomyelitis (ADEM) is an autoimmune inflammatory disease of the central nervous system that is characterized by widespread demyelination, predominantly involving the white matter of the brain and spinal cord. Often caused by a viral infection or vaccination, its clinical features include an acute encephalopathy with multifocal neurologic signs and deficits in children. It can present with psychosis, depression, or abnormal behavior, and it might mimic a dissociative disorder. This report involves a similar rare case of a 14-year-old female patient who presented with fluctuating weakness of body, slurring of speech, tremor, loss of responsiveness, and abnormal behavior after her fever waned. Diagnosis of dissociative disorder was considered in the absence of neurological findings and ongoing significant stressor. Eventually, it turned out to be ADEM, which was confirmed by late neurological manifestations and radiological evaluation. Neuroimaging also revealed its differences from multiple sclerosis.
Keywords: Acute disseminated encephalomyelitis (ADEM), multiple sclerosis, dissociative stupor, psychiatric presentation
Innov Clin Neurosci. 2021;18(7–9):44-46
Acute Disseminated Encephalomyelitis (ADEM) is a rare disease of central nervous system inflammation. Its incidence is 0.4/100,000/year of adolescent population. Natural viral infection causes the disease 20-times more than through vaccination.1,2 Its similarities with other immune-mediated inflammatory disorders, like multiple sclerosis (MS), are evident.3 It can present with several neurological and psychiatric symptoms with varying severity. Though complete recovery is common, untreated cases might turn out to be hemorrhagic variants with high mortality.4
We present the case of a teenage patient with similar enigmatic presentation at National Medical College Birgunj in southern Nepal. Informed written consent was taken from the patient’s guardian to submit this case for publication.
Case Report
A 14-year-old female patient had familial conflicts after her romantic relationship was revealed. Upon confrontation by her parents, the patient decided to end her relationship. Two days later, she developed a high-grade fever, which was abrupt in onset, continuous, as high as 103 degrees Fahrenheit and associated with myalgia. Fever subsided after three days of antibiotic regimen. Then, the patient was discharged. Seven days later, the patient developed fever and was admitted in the pediatric ward. Serum biochemical and hematological investigations were within normal limits. The cerebrospinal fluid study was normal as well. Empirical treatment with intravenous antibiotic and antipyretic was instituted. Fever subsided, but the patient started having nightmares with excessive screaming. During daytime, there were 2 to 3 episodes of alternating unresponsiveness where each episode lasted for around half an hour. The patient gained responsiveness spontaneously. There was no tongue bite, frothing from the mouth, urinary incontinence, or memory deficits. The electroencephalogram was normal as well. The next day, the patient developed episodic weakness in all four limbs along with slurred speech, generalized body numbness, and trembling. These symptoms were evident during daytime, in front of attendants, but not during sleep. Psychiatric consultation was sought. Patient history was uneventful; the patient attained developmental milestones as her other siblings. Other general physical and systemic examinations were within normal limits. In the absence of substantial organic finding and temporal correlation with ongoing conflict, the diagnosis of dissociative stupor was considered. The patient was then shifted to psychiatry ward.
In the psychiatry ward, antibiotics and antipyretics were stopped, and a low dose of sertraline was started. In the next two days, the patient’s fever escalated from 100 to 102 degrees Fahrenheit. Just when pyrexia of unknown origin was being considered, the patient developed difficulty swallowing solid and later to liquid food in addition to the above symptoms. On observation, there was persistent irritability and restlessness. The patient could not sit properly or hold her neck. There was no voluntary effort to maintain normal posture, but she responded to painful stimuli by moans only. The patient’s mouth remained half-open most of the time with a fixed gaze, if not disturbed, and she showed smooth pursuit eye movement while tracing moving objects.
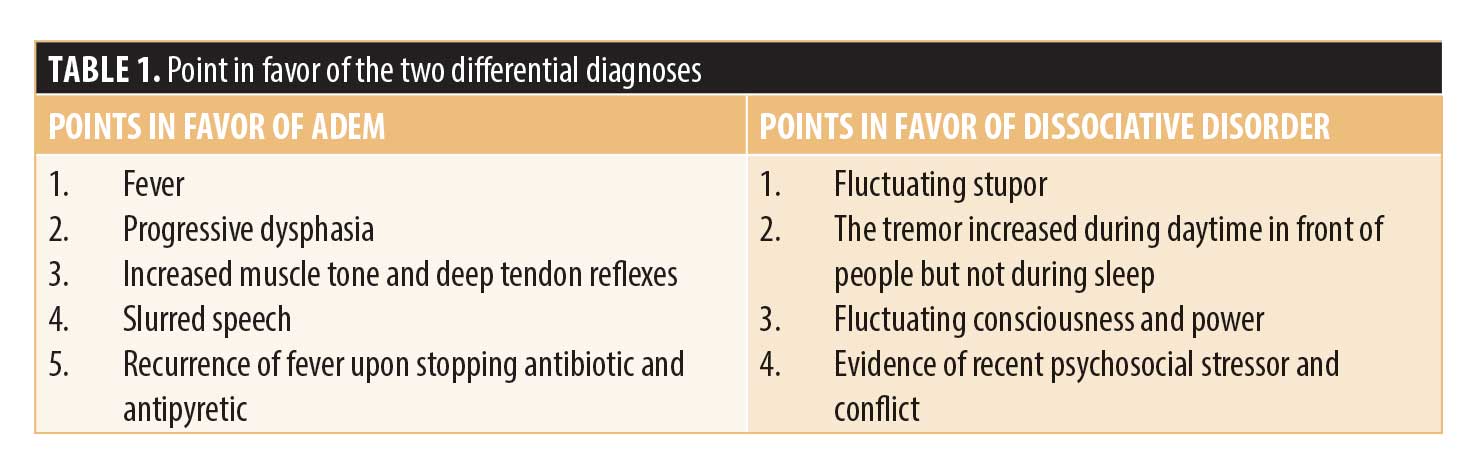
Detailed neurological examination revealed increased tone of bilateral upper and lower limbs and brisk deep tendon reflexes (+++). Brain magnetic resonance imaging (MRI) showed symmetric T2/FLAIR hyperintensity involving bilateral substantia nigra. The additional cystic lesion was seen in prefrontal region suggestive of a neuroepithelial cyst. Points in favor of neurological and psychiatric diagnoses have been tabulated below (Table 1).
Pediatric consultation-liaison team was called in the absence of a dedicated neurology department. Based on above findings, a revised diagnosis of post-infection ADEM was determined. The patient was given intravenous methylprednisolone followed by oral prednisolone 40mg per day, and it was planned to taper this treatment over the next four weeks. Broad-spectrum antibiotics were added, too. The patient gradually improved over the next five days. The patient was later discharged. It had been planned to monitor the patient for neurocognitive sequelae in the form of executive function deficits during follow-ups.
Discussion
The index patient had developed abnormal behavior with unresponsiveness following a possible viral illness. Early presentation and initial evaluation suggested a probable diagnosis of dissociative stupor. Other than unexplained fever, no organic abnormality had developed till the patient was in the pediatric ward. Parental conflicts and behavioral symptoms are not uncommon in the adolescent age group, and their presence misguided the treating clinicians toward a functional disorder. This report highlights how an uncommon neurological case can be easily considered as dissociative or functional disorder in the pediatric or medical ward. It cannot be denied that proper neurological examination can be undermined once the psychiatric or functional disorder is considered, even in the medical unit. This underscores the importance of consultation liaison in day-to-day practice.
Even when the dissociative disorder was suspected, the deteriorating condition of the patient and regular neurological examination in the psychiatric ward revealed the organic neuropathology. It is well known that delayed management of ADEM can result in serious neurological illness.5 The clinical differentiating points among ADEM, MS, and dissociative disorder have been summarized in Table 2. Regular monitoring and examination of the patient can prevent morbidity and mortality.
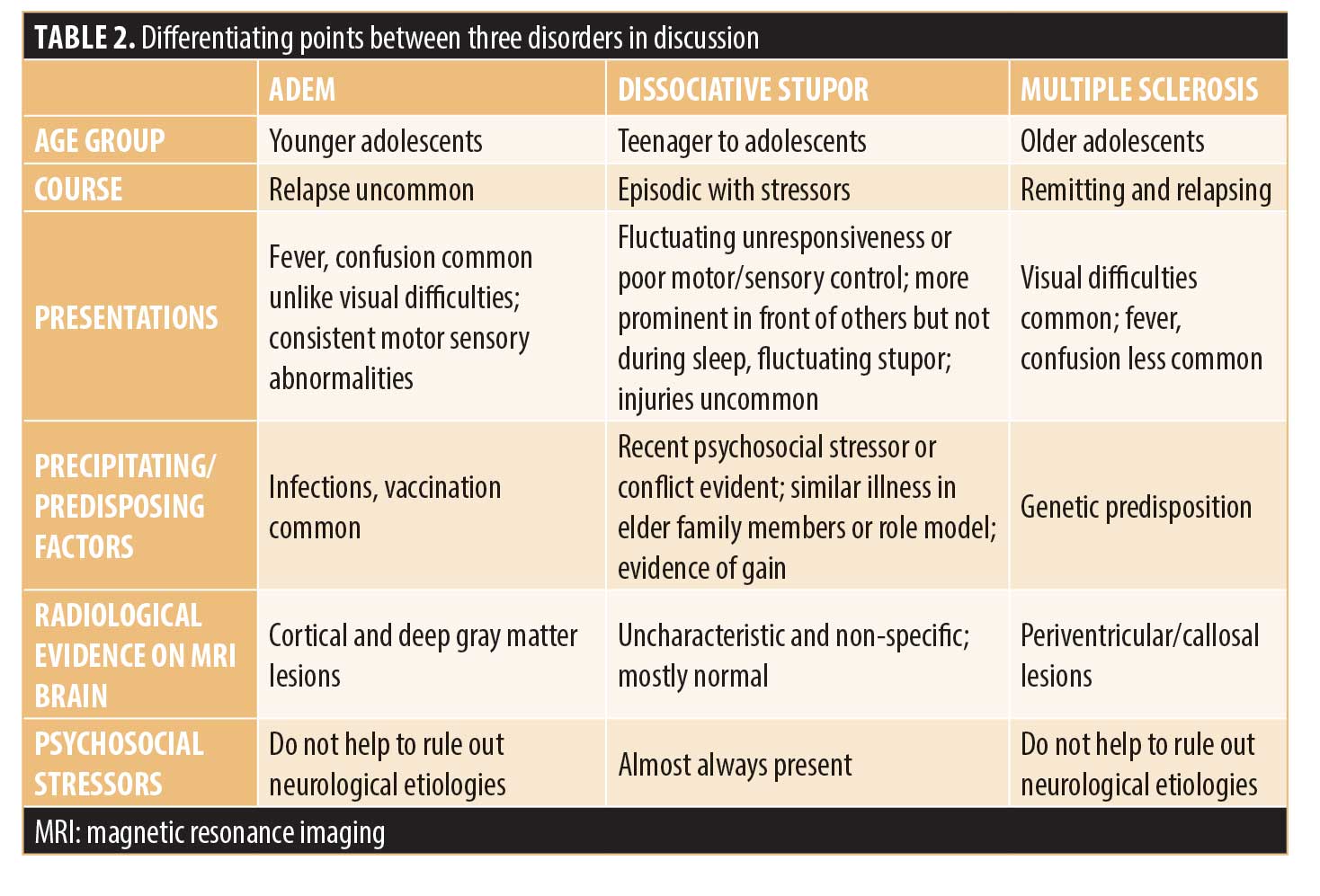
The diagnosis of ADEM can be made by clinical and radiological features in absence of specific biological markers, such as anti-myelin oligodendrocyte glycoprotein (MOG) antibodies in cerebrospinal fluid.6,7 The monophasic course of ADEM is usually common, but recurrent and multiphasic forms can be present at times, raising similarities with MS.8 However, MS occurs in relatively older patients without encephalopathy. It has monosymptomatic presentation and with unilateral optic neuritis. Neuroimaging in MS reveals periventricular lesions or high T2 signal in the calloso-septal interface that were absent in this case.9,10
Neuropsychiatric manifestations of ADEM have not only been reported as early presentations in previous case reports but also as main presentation of relapse.2 These manifestations include manic symptoms, confusion, paranoid delusion, and depression.11,12 Such presentations should also remind of other differentials like systemic lupus erythematosus, N-methyl-D-aspartate (NMDA)-receptor encephalitis, and central nervous system (CNS) vasculitis during clinical evaluation.9,11 It is advised to consider these differential diagnoses while evaluating any young febrile patient with behavioral problems before considering psychiatric illness. Moreover, mortality is higher with ADEM than with dissociative disorders. This warrants clinicians’ attention and high degree of clinical suspicion.
Acknowledgments
The authors want to thank Dr. Amit Jha and Mr. Ashok Sah for editing English language of the manuscript.
References
- Tenembaum SN. Acute disseminated encephalomyelitis. Handb Clin Neurol. 2013;112:1253–1262.
- Garg RK. Acute disseminated encephalomyelitis. Postgrad Med J.
2003;79(927):11–17. - Menge T, Hemmer B, Nessler S, et al. Acute disseminated encephalomyelitis: an update. Arch Neurol. 2005;62(11):1673–1680.
- Anlar B, Basaran C, Kose G, et al. Acute disseminated encephalomyelitis in children: outcome and prognosis. Neuropediatrics. 2003;34(04):194–199.
- Tenembaum S, Chamoles N, Fejerman N. Acute disseminated encephalomyelitis: a long-term follow-up study of 84 pediatric patients. Neurology. 2002;59(8):1224–1231.
- Hynson JL, Kornberg AJ, Coleman LT, et al. Clinical and neuroradiologic features of acute disseminated encephalomyelitis in children. Neurology. 2001;56(10):1308–1312.
- Leake JA, Albani S, Kao AS, et al. Acute disseminated encephalomyelitis in childhood: epidemiologic, clinical and laboratory features. J Pediatr Infect Dis. 2004;23(8):756–764.
- Schwarz S, Mohr A, Knauth M, et al. Acute disseminated encephalomyelitis: a follow-up study of 40 adult patients. Neurology. 2001;56(10):1313–1318.
- Alper G. Acute disseminated encephalomyelitis. J Child Neurol.
2012;27(11):1408–1425. - Dale RD, De Sousa C, Chong WK, et al. Acute disseminated encephalomyelitis, multiphasic disseminated encephalomyelitis and multiple sclerosis in children. Brain.
2000;123(12):2407–2422. - Habek M, Brinar M, Brinar VV, Poser CM. Psychiatric manifestations of multiple sclerosis and acute disseminated encephalomyelitis. Clin Neurol Neurosurg. 2006;108(3):290–294.
- Moscovich DG, Singh MB, Eva FJ, Puri BK. Acute disseminated encephalomyelitis presenting as an acute psychotic state. J Nerv Ment Dis. 1995;183(2):116–117.





