 by Jonathan R. Scarff, MD
by Jonathan R. Scarff, MD
Dr. Scarff is with the Behavioral Health Service Line, Kenner Army Health Clinic, in Fort Lee, Virginia.
Funding: No funding was provided.
Disclosures: Disclaimer: The views expressed in this article are those of the author and do not reflect official policy or position of the Kenner Army Health Clinic, the Department of the Army, or the Department of Defense.
Abstract: Postpartum depression (PPD) in women is common and adversely affects the mother, infant, and family unit. Treatments include psychotherapy and pharmacotherapy, but not all women experience response or remission, and response might be delayed. A precipitous decrease in allopregnanolone levels and failure of GABAA receptors to adapt to this change might contribute to PPD. Administered intravenously, brexanolone (BRX) is a solution of allopregnanolone that modulates the GABAA receptor and restores third-trimester levels, thus allowing for receptor adaptation and symptom improvement. In clinical studies, patients receiving BRX experienced a rapid reduction or remission of depression. Due to the risk for sedation or syncope, it is only available through a national registry, and administration and monitoring must occur in a supervised medical setting. Further studies are needed to explore its long-term efficacy.
Keywords: postpartum, depression, GABAA, brexanolone, allopregnanolone
Innov Clin Neurosci. 2019;16(11–12):32–35
Postpartum depression (PPD) in women is often defined as a major depressive episode (MDE) occurring one month postpartum, though it is sometimes defined as either a major or minor depressive episode occurring up to one year postpartum.1,2 It has an incidence of 8 to 20 percent among new mothers in the United States; data regarding prevalence are scarce due to possible underreporting by mothers and variable criteria for time of onset.3,4 In contrast with nonpostpartum women experiencing a depressive episode, women with PPD might additionally present with restlessness and agitation, impaired concentration and decision-making, and less prominent depressed mood.5 Risks of untreated PPD include maternal suicide, impaired infant attachment, and delays in the child’s height, weight, and behavioral development.6,7
Risk factors and potential causes include stressful life events, marital conflict, single parenthood, presence of anxiety, history of a previous episode of PPD, and hormonal fluctuations.3,8 Hormonal changes implicated in PPD include the precipitous decrease in progesterone and estradiol after delivery, dysregulation of the hypothalamus–pituitary–adrenal (HPA) axis with hypersecretion of cortisol in individuals with depressive episodes, and low levels of oxytocin in third-trimester women who later developed PPD.9 However, it is unknown to what degree such hormone changes might contribute to PPD, and these changes might not be present among all women with PPD.
Psychotherapy, such as cognitive behavioral therapy, is recommended as first-line treatment for mild-to-moderate PPD due to rapid efficacy, lack of adverse effects on mother and infant, and no impact on breastfeeding.10 Pharmacotherapy, either individually or in combination with psychotherapy, is advised for moderate-to-severe PPD.10,11 Selective serotonin inhibitors, particularly sertraline and citalopram, are recommended due to minimal effects on breastfeeding; common adverse effects include headache, gastrointestinal distress, fatigue, insomnia, sweating, and possible worsening mood or anxiety.10 Fluoxetine is generally discouraged due to its long half-life and presence in breast milk, while paroxetine is not recommended due to the risk for congenital heart defects.10
The efficacy of pharmacotherapy is not established specifically for women with PPD due to a lack of clinical trials and ethical constraints with using pregnant participants.12 A retrospective study comparing women with PPD and non-PPD found that time to remission was greater among women with PPD (one month or more), and they generally required more than one antidepressant, even though both groups ultimately achieved remission.13,14 Given the prevalence and adverse impact of PPD, as well as the limitations of current pharmacological treatments (i.e., adverse effects and response time), alternative treatments are needed.
Progesterone and its metabolite allopregnanolone are positive allosteric modulators of the GABAA receptor, and both GABAA levels and receptor activity are diminished in patients with depression.15,16 These hormone levels rise steadily until parturition and then decline precipitously, so decreased hormone concentrations and a lack of GABAA receptor adaptation might contribute to PPD.17,18 As such, increasing postpartum allopregnanolone levels to earlier third-trimester levels and then slowly tapering to prepartum levels might facilitate receptor adaptation and alleviate PPD.
Approved in March 2019 to treat PPD, brexanolone (BRX) is a buffered, isotonic solution of 5mg/mL allopregnanolone in 250mg/mL sulfobutylether-β-cyclodextrin that is administered intravenously over 60 hours. This article reviews the efficacy, safety, dosing, precautions, advantages, limitations, and future areas for exploration for BRX.
Dosing and Administration
BRX is available in 100mg/20mL vials and is administered as a single infusion intravenously over 60 hours in a supervised medical setting.19 It is initiated at 30mcg/kg/hour for four hours, increased to 60mcg/kg/hour for 20 hours, maintained at 90mcg/kg/hour for 28 hours (or 60mcg/kg/hour if a higher dose is not tolerated), decreased to 60mcg/kg/hour for four hours, and finally lowered to 30mcg/kg/hour for the last four hours.19 Prior to infusion, patients should inform prescribers if they are taking sedating medications due to the risk for excessive sedation. To ensure accurate assessment of sedation, the infusion is started during daytime waking hours. Patients must receive continuous pulse-oximetry monitoring and be reviewed every two hours for excessive sedation or loss of consciousness, and the infusion should be stopped in the case of hypoxia or sedation (but it can be resumed if the sedation resolves).19 The dose should be decreased or stopped in the case of worsening depression or suicidal ideation. Patients are discouraged from driving or engaging in activities requiring alertness until any sedation resolves.19 During infusions, patients should avoid alcohol and be accompanied during interactions with their children.
Efficacy and Tolerability
Four studies evaluated the antidepressant effect of BRX administered as a single infusion over 60 hours, with details noted in Table 1. All studies enrolled women ages 18 to 45 years, and the primary outcome measure (except where noted) was changed in total score on the 17-item Hamilton Rating Scale for Depression (HAM-D).20 Remission was defined by the following HAM-D scores: no depression/remission (0–7 points); mild depression (8–16 points); moderate depression (17–23 points); and severe depression (≥ 24 points).21 The first study was an open-label trial of four women in a perinatal psychiatric inpatient unit with a major depressive episode (MDE) that had begun no earlier than the third trimester and no later than three months postpartum and was classified as severe.22 All four participants received BRX 60mcg along with psychotherapy, while two were continued on stable doses of antidepressant (sertraline) and another was continued on an unspecified psychotropic medication. Primary study outcomes were safety and tolerability, as assessed by reported adverse effects and physical and psychiatric evaluations. The secondary outcome measure was efficacy, as assessed using change in total HAM-D score. All patients completed the infusions. At 60 hours, the mean total HAM-D score had decreased from 26.5 to 1.8 points (p=0.001 vs. baseline), corresponding to symptom remission; this increased slightly to 5.3 points at Hour 84. All four patients reported adverse effects—most commonly, sedation (n=2). Less common side effects (n=1 each) included infusion site discomfort, pain, or erythema; rash; thyroid-stimulating hormone increase; dizziness; flushing; and oropharyngeal pain. All were transient and of mild or moderate severity, and no deaths, serious adverse events, or discontinuations occurred.
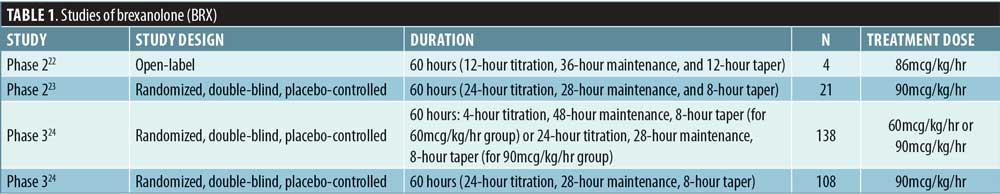
The second study enrolled ambulatory individuals with an MDE that began no earlier than the third trimester but no later than one month postpartum.23 Twenty-one women were randomly assigned to the BRX (n=10) and placebo (n=11) groups. Three participants in each group were receiving antidepressants, and all participants completed the infusions. At 60 hours, the mean reduction in HAM-D total score from baseline was 21.0 points (standard error [SE]: 2.9 points) in the BRX group compared to 8.8 points (SE: 2.8 points) in the placebo group (difference: −12.2, 95% confidence interval [CI]: −20.77 to −3.67; p=0.0075; effect size: 1.2). Seven patients in the BRX group achieved symptom remission compared to only one patient in the placebo group; the percentage of responders was not provided. Four patients in the BRX group had adverse events compared to eight in the placebo group. The most frequently reported adverse events in the BRX group were dizziness (2 patients in the BRX group vs. 3 patients in the placebo group) and somnolence (2 vs. 0). Moderate treatment-emergent adverse events were reported in two patients in the BRX group (sinus tachycardia, n=1; somnolence, n=1) and in two patients in the placebo group (infusion site pain, n=1; tension headache, n=1). Additionally, one patient in the placebo group had a severe treatment-emergent adverse event (insomnia). No deaths, serious adverse events, or discontinuations because of adverse events were reported in either group.
The third study recruited ambulatory female patients with MDE onset occurring no earlier than the third trimester and no later than one month postpartum.24 In total, 138 women were randomly assigned to receive BRX 60mcg (n=47), BRX 90mcg (n=45), or placebo (n=46). Patients in all groups were taking antidepressants as follows: BRX 60mcg (n=14), BRX 90mcg (n=13), or placebo (n=30). Two patients (one in the BRX 60mcg group and one in the placebo group) withdrew from the study due to adverse effects, while 23 patients discontinued because they did not receive the infusion, were lost to follow-up, or withdrew consent. At 60 hours, the mean reduction in HAM-D total score was 19.5 points (SE 1.2) in the BRX 60mcg group and 17.7 points (SE 1.2) in the BRX 90mcg group as compared with 14.0 points (SE: 1.1) in the placebo group (difference: −5.5, 95% CI: −8.8 to −2.2; p=0.0013 for the BRX 60mcg group and difference: −3.7, 95% CI: −6.9 to −0.5; p=0.0252 for the BRX 90mcg group).
Nineteen patients in the BRX 60mcg group and 22 in the BRX 90mcg group had adverse events as compared with 22 patients in the placebo group. The most frequently reported adverse events were headache (13 patients in the BRX groups vs. 7 patients in the placebo group), dizziness (12 patients in the BRX groups vs. 1 patient in the placebo group), and somnolence (9 patients in the BRX groups vs. 3 patients in the placebo group). One patient in the BRX group reported suicidal ideation with attempt.
The fourth study also recruited ambulatory female patients with MDE onset occurring no earlier than the third trimester and no later than one month postpartum.24 In total, 108 women were randomly assigned to the BRX (n=54) or placebo (n=54) groups. Twelve patients in the BRX group and 15 patients in the placebo group were receiving antidepressants. Two patients in the BRX group withdrew from the study due to a treatment-related adverse effect, while six patients discontinued the study because they did not receive the infusion, were lost to follow-up, or withdrew consent. At 60 hours, the mean reduction in HAM-D total score was 14.6 points (SE: 0.8) in the BRX group as compared with 12.1 points (SE: 0.8) in the placebo group (difference: −2.5, 95% CI: −4.5 to −0.5; p=0.0160). An integrated analysis of data from the third and fourth studies found that 70 patients in the BRX 90mcg group were responders, and 26 of them achieved remission compared to 16 remitters in the placebo group.
In the fourth study, the most frequently reported adverse events in the BRX group were headache (9 patients vs. 7 patients in the placebo group), dizziness (5 patients vs. 4 patients in the placebo group), and somnolence (4 patients vs. 2 patients in the placebo group). One patient experienced altered consciousness and syncope.
Safety
BRX is categorized as a Schedule IV drug by the Drug Enforcement Administration (DEA). Despite its modulation of the GABAA receptor, there were no signs or symptoms of “drug liking,” dependence, withdrawal, misuse, abuse, or diversion during clinical trials. In a randomized crossover study examining abuse potential, 40 nondependent recreational drug users (drugs not specified) were randomized to receive placebo, a therapeutic dose of BRX (90mcg), a supratherapeutic dose of BRX (180mcg or 270mcg), or alprazolam (1.5mg or 3mg).25 The incidence of euphoric mood with BRX was dose-dependent: 3.1 percent (n=1) with 90mcg, 9.4 percent (n=3) with 180mcg, and 12.5 percent (n=4) with 270mcg and less often compared to alprazolam 3mg (n=6; 19.4%). No data were available for the incidence of euphoria with the 1.5mg alprazolam dose.25 Information on the time to onset and the duration of euphoria in affected patients receiving BRX was unavailable.
Metabolism and Precautions
Following infusion, BRX is renally metabolized by keto-reduction, glucuronidation, and sulfation.19 Circulating metabolites are pharmacologically inactive and are excreted in nearly equal amounts in urine and feces. It carries a “black box warning” due to the risk for somnolence and excessive sedation; therefore, it is only available for healthcare facilities and patients who are enrolled in a Risk Evaluation and Mitigation Strategy registry.19 Although BRX does not have contraindications, it should be avoided in pregnant women and those with end-stage renal disease.19 It can be offered to patients with mild-to-severe renal impairment or any level of hepatic impairment.19 Although 1 to 2 percent of BRX enters breast milk, available data do not suggest a significant risk of adverse reactions in breastfed infants.
Advantages and Limitations
BRX is the first FDA-approved treatment for PPD, a condition that has profound adverse effects on mothers, infants, the family unit, and society. Advantages of BRX include its novel mechanism of action, larger effect size, and quicker response and remission compared to conventional oral treatments.23 Limitations include a need for hospitalization for intravenous administration and inpatient monitoring, though an oral formulation currently under development might mitigate these limitations. An additional limitation is the estimated $34,000 cost of one infusion prior to any available discounts and excluding costs associated with hospitalization.26 This might preclude access for uninsured patients or first require failures of conventional treatments in order to receive insurance authorization.
Conclusion
BRX might be an ideal treatment in women with access to hospitals and who have a history of severe PPD with a prolonged recovery time or limited response to psychotherapy or serotonin reuptake inhibitors. The findings of efficacy studies are limited because they did not report outcomes for study subjects beyond 30 days; therefore, further trials are needed to assess BRX’s long-term efficacy and safety and its place in treatment algorithms.
Acknowledgment
The author wishes to thank Marilyne Kpetemey, PhD, for her helpful clarifications during the preparation of this article.
References
- American Psychiatric Association. Depressive Disorders. In: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Press Inc.; 2013: 155–188.
- Committee on Obstetric Practice. The American College of Obstetricians and Gynecologists Committee Opinion No. 630: screening for perinatal depression. Obstet Gynecol. 2015;125(5):1268–1271.
- Anokye R, Acheampong E, Budu-Ainooson A, et al. Prevalence of postpartum depression and interventions utilized for its management. Ann Gen Psychiatry. 2018;9(17):18.
- Ko JY, Rockhill KM, Tong VT, et al. Trends in postpartum depressive symptoms—27 States, 2004, 2008, and 2012. MMWR Morb Mortal Wkly Rep. 2017;66(6):153–158.
- Bernstein IH, Rush AJ, Yonkers K, et al. Symptom features of postpartum depression: are they distinct? Depress Anxiety. 2008;25(1):20–26.
- Farías-Antúnez S, Xavier MO, Santos IS. Effect of maternal postpartum depression on offspring’s growth. J Affect Disord. 2018;228:143–152.
- Faleschini S, Rifas-Shiman SL, Tiemeier H, et al. Associations of prenatal and postnatal maternal depressive symptoms with offspring cognition and behavior in mid-childhood: a prospective cohort study. Int J Environ Res Public Health. 2019;16(6). pii:E1007.
- Andrews-Fike C. A review of postpartum depression. Primary Care Companion J Clin Psychiatry. 1999;1(1):9.
- Brummelte S, Galea LA. Postpartum depression: etiology, treatment and consequences for maternal care. Horm Behav. 2016;77:153–166.
- Molenaar NM, Kamperman AM, Boyce P, Bergink V. Guidelines on treatment of perinatal depression with antidepressants: an international review. Aust N Z J Psychiatry. 2018;52(4):320–327.
- Kim DR, Epperson CN, Weiss AR, Wisner KL. Pharmacotherapy of postpartum depression: an update. Expert Opin Pharmacother. 2014;15(9):1223–1234.
- Van Ravesteyn LM, Lambregtse van den Berg MP, Hoogendijk WJG, et al. Interventions to treat mental disorders during pregnancy: a systematic review and multiple treatment meta-analysis. PLoS One. 2017;12:e0173397.
- Cox EQ, Sowa NA, Meltzer-Brody SE, Gaynes BN. The perinatal depression treatment cascade: baby steps toward improving outcomes. J Clin Psychiatry. 2016;77(9):1189–1200.
- Hendrick V, Altshuler L, Strouse T, Grosser S. Postpartum and nonpostpartum depression: differences in presentation and response to pharmacologic treatment. Depress Anxiety. 2000;11(2):66–72.
- Majewska MD, Harrison NL, Schwartz RD, et al. Steroid hormone metabolites are barbiturate-like modulators of the GABA receptor. Science. 1986;232(4753):1004–1007.
- Romeo B, Choucha W, Fossati P, Rotge JY. Meta-analysis of central and peripheral γ-aminobutyric acid levels in patients with unipolar and bipolar depression. J Psychiatry Neurosci. 2018;43(1):58–66.
- Luisi S, Petraglia F, Benedetto C, et al. Serum allopregnanolone levels in pregnant women: changes during pregnancy, at delivery, and in hypertensive patients. J Clin Endocrinol Metab. 2000;85(7):2429–2433.
- Schüle C, Nothdurfter C, Rupprecht R. The role of allopregnanolone in depression and anxiety. Prog Neurobiol. 2014;113:79–87.
- Sage Therapeutics. ZULRESSO™ (Brexanolone) Prescribing information. Cambridge, MA. March 2019.
- Hamilton M. A rating scale for depression. J Neuro Neurosurg Psychiatry. 1960;23:56–62.
- Zimmerman M, Martinez JH, Young D, et al. Severity classification on the Hamilton Depression Rating Scale. J Affect Disord. 2013;150(2):384–388.
- Kanes SJ, Colquhoun H, Doherty J, et al. Open-label, proof-of-concept study of brexanolone in the treatment of severe postpartum depression. Hum Psychopharmacol. 2017;32(2).
- Kanes S, Colquhoun H, Gunduz-Bruce H, et al. Brexanolone (SAGE-547 injection) in post-partum depression: a randomised controlled trial. Lancet. 2017;390(10093):480–489.
- Meltzer-Brody S, Colquhoun H, Riesenberg R, et al. Brexanolone injection in post-partum depression: two multicentre, double-blind, randomised, placebo-controlled, Phase 3 trials. Lancet. 2018;392(10152):1058–1070.
- Sage Therapeutics. Brexanolone injection, for intravenous use. Sponsor briefing document. Presented at the Joint Meeting of the Psychopharmacologic Drug Advisory Committee and Drug Safety and Risk Management Advisory Committee; November 2, 2018; Silver Spring, MD.
- Howard J. FDA approves first postpartum depression drug. Available at: https://www.cnn.com/2019/03/19/health/postpartum-depression-drug-fda-bn/index.html. Accessed August 24, 2019.





