by Maria Fe Garcia-Rada, MPS, and Robert E. Litman, MD
Ms. Fe Garcia-Rada and Dr. Litman are with CenExel CBH Health in Gaithersburg, Maryland. Dr. Litman is additionally with Georgetown University Medical School in Washington, DC.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Innov Clin Neurosci. 2024;21(1–3):13–18.
Abstract
Objective: This study aimed to examine the impact of the COVID-19 pandemic on patients with serious mental illness (SMI), specifically relating to psychiatric morbidity, pandemic-induced stress, and ability to cope with pandemic-related precautionary measures, restrictions, and disruptions to daily life.
Design: A cross-sectional survey study of 277 clinical trial patients was conducted. This sample included nonpsychiatric controls (n=139) and patients with a diagnosis of bipolar disorder, major depressive disorder (MDD), or schizophrenia (n=138) located at five clinical trial sites across the United States. A univariate analysis was performed to obtain general frequencies of the sample. Unpaired t-tests were used in comparing the groups on numerical variables, and analysis of variance (ANOVA) was performed to identify differences when comparing three or more categories.
Results: Patients with SMI were more likely to report wearing face masks, avoiding large gatherings, and endorsing the use of precautionary measures, despite receiving a COVID-19 vaccine (p<0.001). A total of 70.3 percent (n=97) of all patients with SMI reported experiencing at least one episode of symptom worsening, 48 percent reported experiencing suicidal ideation, and 66 percent reported a need for increased mental healthcare due to COVID-19-related distress. Patients with SMI reported higher levels of stress, compared to controls, with patients with MDD having the highest levels of stress (p<0.001).
Conclusion: These findings demonstrate an increased vulnerability to symptom worsening in patients with SMI during a pandemic and suggest the need to account for pandemic-induced psychological stress in clinical trial design, subject selection, and symptoms ratings.
Keywords: Clinical trials, mood disorders, COVID-19, pandemic, psychiatry
While many studies have investigated the psychological impact of the COVID-19 pandemic on the general population,1 less is known regarding the effects of COVID-19 pandemic-related stress on individuals with premorbid psychiatric illnesses, especially those with serious mental illness (SMI), which is defined as a mental, behavioral, or emotional disorder that causes significant functional impairment.2 Early in the pandemic, clinical concerns were raised regarding the potential for poorer outcomes due to the pandemic in patients with SMI, who are considered to be an especially vulnerable population.3 For instance, patients with SMI diagnosed with schizophrenia or bipolar disorder often have disorder-related cognitive deficits and comorbid medical conditions, placing this population at an increased risk for infection and adverse outcomes from COVID-19.3 Structural barriers (e.g., unstable housing) can also place individuals with SMI at greater risk for exposure to infection. Other risk factors for patients with SMI include changes in the delivery or frequency of mental healthcare services, especially outpatient care; while in-person services can increase the risk of transmission, the lack of these types of services can contribute to service disengagement, medication nonadherence, distress, and, ultimately, exacerbation of symptoms.4 Consistent with these concerns, accumulated evidence suggests that increased mortality from COVID-19 infection is associated with premorbid psychiatric illness, particularly schizophrenia spectrum diagnoses.5–7
In addition, heightened levels of psychological distress and psychiatric symptoms have been reported among psychiatric patients during the COVID-19 pandemic. Comprehensive reviews analyzing published surveys of patient cohorts with SMI have shown higher levels of anxiety, depression, insomnia, weight gain, acute stress, and suicidal ideation among those with a preexisting mental illness, compared to healthy controls in most,1,8–16 although not all,17,18 studies.
Several studies have reported a disproportionate impact of the pandemic on patients with affective disorders, compared to those with psychotic disorders, including evidence that patients with affective disorders score higher on measures of pandemic-induced psychological distress when compared to individuals with psychotic disorders.15,19 Interestingly, despite increases in symptoms and stress, studies have reported that patients with SMI are engaging in the use of protective measures, such as compliance with stay-at-home orders and use of face masks, at rates comparable to healthy controls.20–22
In a previous investigation, we surveyed 94 patients with SMI who were clinical trial participants in non-COVID-19-related trials from June through September 2020.23 Consistent with other studies in the literature, we found that their knowledge, risk perception, and use of precautionary safety measures during the pandemic were robust and mirrored the general population. Also, while 62 percent of patients reported experiencing moderate or extreme levels of distress, high levels of stress were correlated with positive coping skills, with the highest levels of stress found in patients with major depressive disorder (MDD).23
In this investigation, we aimed to replicate and extend these results concerning COVID-19-related knowledge, risk perception, and use of precautionary measures by conducting a new survey in a separate and larger group of clinical trial patients with SMI and nonpsychiatric control clinical trial subjects. We measured pandemic stress for both groups utilizing Kessler’s Psychological Distress Scale (K10). We surveyed patients specifically for their clinical status, including worsening symptoms, worsening of illness, and suicidal ideation during the pandemic. It was predicted that pandemic-induced stress would be significantly higher in patients with SMI and that pandemic-induced stress would positively correlate with worsening psychiatric clinical status.
Methods
Participants. The study sample (n=277) included adults with a diagnosis of MDD, bipolar disorder, or schizophrenia (n=138) and control subjects without a psychiatric diagnosis (n=139). Both psychiatric patients and controls were selected for participation in the survey from various clinical trial sites located in five distinct geographic areas across the United States (Montgomery County, Maryland; Fulton County, Georgia; Broward County, Florida; Salt Lake County, Utah; and Los Angeles County, California), based on current or previous participation in a clinical trial, and their willingness and ability to complete a survey.
Assessments. A cross-sectional questionnaire assessing the impact of COVID-19 was utilized, which consisted of over 60 questions pertaining to demographics, COVID-19 infection and vaccination status, COVID-19-related healthcare services, COVID-19-related knowledge, concerns regarding COVID-19, risk perception, and use of precautionary measures.23 The current questionnaire was revised and expanded to include questions that exclusively surveyed patients with SMI for their clinical status, including worsening symptoms, worsening of illness, and suicidal ideation during the pandemic.
Pandemic-induced psychological stress was assessed in all participants using K10, a 10-item self-report scale with well-established reliability and validity that measures anxiety and depressive symptoms present within the past 30 days and yields a global measure of psychological distress.24 Responses for each question are scored on a five-point Likert scale ranging from 1 (“none of the time”) to 5 (“all of the time”). The responses to each item are added, and a total score is derived.
Procedures. Participants were identified through current or previous participation in an industry-sponsored clinical trial and were approached in person by a trained interviewer at the time of their in-clinic study visit. They were provided with the rationale and overview of the study and were invited to answer a set of questions about the impact of the COVID-19 pandemic. After obtaining informed consent from participants, the interviewer administered the questionnaire face-to-face, recording all participant responses through Qualtrics. Data collection occurred from April to July 2021.
Data analysis. Univariate analysis was performed to obtain general frequencies of the sample’s descriptive characteristics. Sociodemographic variables and prevalence rates for COVID-19 disease management were estimated for both arms of the study. T-tests were used when comparing numerical variables (e.g., age, total K10) between patients with SMI and healthy controls. Analysis of variance (ANOVA) was used to compare numerical variables between SMI diagnostics. Categorical variables (e.g., sex, race, income, etc.) were compared using Pearson’s Chi-squared test of independence.
Distress categories were obtained and scored from 1 to 4, where 1 was assigned to patients with a K10 score less than 20, and 4 for patients with a K10 score of 30 or higher.24 A median-split dichotomization was used for the total K10 scores to classify patients with SMI between low- and high-stress. Participants with a K10 score of 19 or lower were grouped into the low-stress category (i.e., K10 total: 10–19), while those with a total score of 20 or higher were grouped into the high-stress category (i.e., K10 total: 20–50). Differences between low- and high-stress were evaluated using Pearson’s Chi-squared test. An alpha level of 0.05 was used throughout the analysis. R/R Studio was used for all the statistical analyses.
Results
Sample characteristics. A total of 277 individuals were surveyed, including 138 subjects with SMI and 139 non-SMI controls. Both groups were comparable in age (patients with SMI—mean: 41.5 years, standard deviation [SD]: 12.9 years; non-SMI controls—mean: 38.0 years, SD: 14.0 years). However, compared to controls, patients with SMI were predominantly male, Black/African American, unemployed, earning less than $30,000 a year, and living alone without family (p<0.001). In addition, more patients with SMI were unmarried (p<0.01) and lacking a high school diploma (p<0.04; Table 1). All patients with SMI had lifetime diagnoses of either schizophrenia (50%), bipolar disorder (17%), or MDD (29%).
COVID-19 disease management and use of precautionary measures. The incidence of COVID-19 infection was significantly lower in the SMI cohort, with seven out of 138 patients (5.1%) reporting infection, compared to 19 (13.7%) of non-SMI control subjects (p<0.05). More controls reported being exposed to the virus, compared to patients with SMI (44% vs. 21%; p<0.001). Approximately half of each group of subjects had been vaccinated (SMI cohort: 51%, non-SMI cohort: 55%; p>0.05). Overall, both subject groups quarantined and obtained diagnostic testing at similar rates and at similar healthcare settings, including clinical trial sites. In addition, while both groups reported using precautionary measures, patients with SMI were more likely than control subjects to socially distance, avoid large gatherings and crowds, and continue using precautionary measures postvaccination (p<0.001).
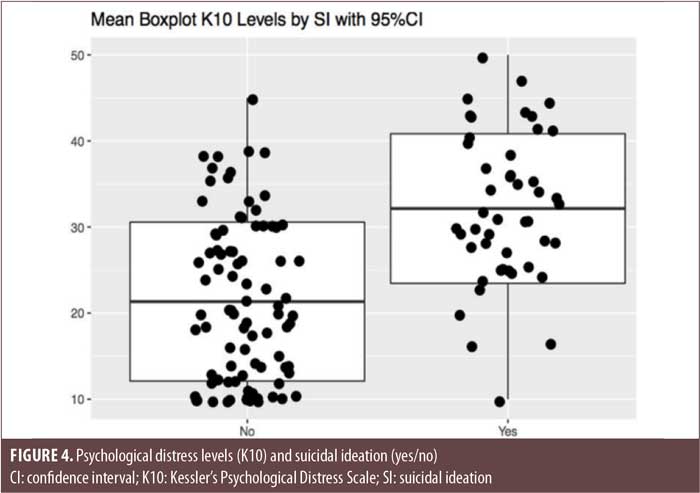
Increases in psychiatric morbidity and psychological distress (K10). Ninety-seven of 138 patients with SMI (70%) reported worsening of psychiatric symptoms during the surveyed pandemic period, including worsening of depression (29%), anxiety (28%), change in sleep patterns (24%), paranoid ideas (11%), auditory hallucinations (10%), and mania (4%). Symptoms of depression and anxiety were more prevalent among patients with MDD or bipolar disorder, but only worsening of depressive symptoms among patients with MDD was significant (p<0.05). Worsening of psychosis was only reported by patients with schizophrenia. Suicidal ideation was reported by 48 patients with SMI (35%), and suicide attempts during the pandemic period were only reported by patients with bipolar disorder or schizophrenia. Patients with MDD had significantly lower suicide attempts during the pandemic, compared to patients with bipolar disorder or schizophrenia (p<0.05). Sixty-six patients with SMI (48%) reported seeking increased levels of mental healthcare, including more frequent outpatient appointments with mental health providers (61%), increases or changes in medications (59%), visits to emergency rooms for mental healthcare (20%), and admission to a psychiatric hospital (15%). There were no other statistically significant differences for these variables across diagnostic groups.
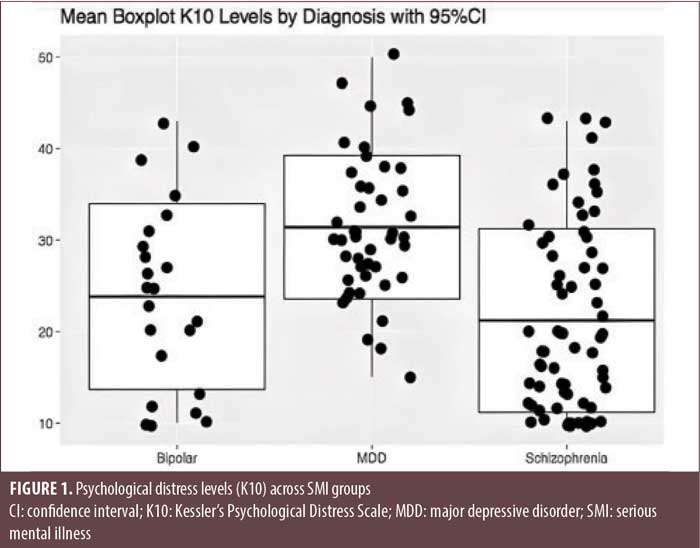
Patients with SMI had significantly higher K10 total scores, compared to non-SMI control subjects (SMI cohort, mean [SD]: 25.03 [10.39] vs. non-SMI cohort: 15.50 [6.59]; p<0.001). Patients with SMI were more prevalent in the high-stress group, compared to non-SMI controls. Among patients with SMI, those with MDD had the highest K10 total scores, which were significantly higher than the scores of patients with schizophrenia, while K10 total scores for patients with bipolar disease were intermediate between both groups (MDD, mean [SD]: 31.40 [7.85]; bipolar disorder: 23.83 [10.14]; schizophrenia: 21.22 [10.03]; p<0.001). There was a higher number of patients with MDD in the high-stress group, compared to patients with bipolar disorder or schizophrenia (Table 2 and Figure 1).
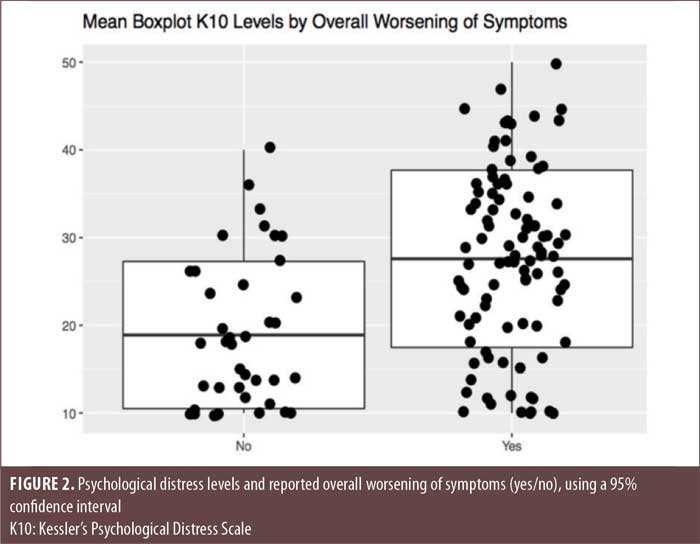
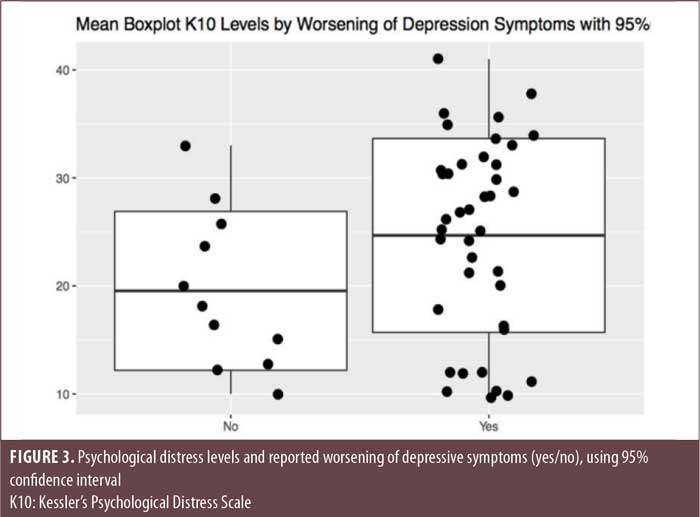
Finally, while there were no differences between SMI diagnostic groups regarding psychiatric morbidity, overall symptom worsening and suicidal ideation were found to be statistically, significantly associated with higher levels of pandemic-induced stress, as measured by the K10, in patients with SMI (Figures 2 and 3). This was also the case for worsening of depression, although this did not reach statistical significance (Figure 4).
Discussion
In this survey of 277 clinical trial participants during the COVID-19 pandemic, we found that clinical trial participants with SMI acted similarly to non-SMI participants regarding efforts to prevent infection, including viral testing, knowledge of COVID-19 risk factors, personal protective measures, seeking medical assistance for COVID-19, and obtaining COVID-19 vaccinations. In addition, compared to non-SMI controls, patients with SMI had significantly lower rates of COVID-19 infection and prior COVID-19 exposure and were more likely to continue partaking in social distancing and precautionary measures.
We found that nearly three-quarters of clinical trial participants with SMI reported worsening of psychiatric symptoms (e.g., depression, anxiety, auditory hallucinations, paranoia, and suicidal ideation) during the pandemic, accompanied by increases in mental healthcare interventions, including outpatient clinician visits, changes in medications, emergency room visits, and hospitalizations. We also found that, in comparison to non-SMI controls, patients with SMI had significantly higher levels of pandemic-induced psychological stress, as measured by K10 total score. Specifically, patients with MDD had the highest K10 total scores, and MDD was the most prevalent diagnosis in the high-stress group, although all SMI diagnostic groups had significantly higher K10 scores, compared to non-SMI controls.
Perhaps most importantly, we found that high levels of psychological stress, as measured by the K10, were associated with overall worsening of psychiatric symptoms and suicidal ideation. The latter finding has particular relevance to other observations of increased levels of suicidal ideation among psychiatric populations, including SMI, and underlines the need for special attention to be paid to the potential of heightened suicidal risk in psychiatric patients during a pandemic, even in clinically stable outpatients who are not infected with COVID-19.25 It also suggests that preventative therapeutic interventions designed to relieve pandemic-induced stress among patients with SMI might be important to reduce suicidal ideation/behavior and overall psychiatric morbidity, especially during new onset COVID-19 infection related to the appearance of new variants.
Our findings regarding the effects of the COVID-19 pandemic in a second sample of clinical trial participants with SMI surveyed at a later time in the pandemic (April–July 2021) substantially replicated our previous findings, using similar methodology to our previous sample of 94 clinical trial participants with SMI earlier in the pandemic (June–September 2020).23 These findings are consistent with other published reports, which suggest that patients with SMI have adequate knowledge on COVID-19 risks and are responsibly using precautionary measures and quarantine in an effort to safeguard themselves and prevent the spread of infection.20–22 These findings are also in agreement with the majority of studies and reviews that report worsening of psychiatric symptoms and increased psychological stress in individuals with premorbid psychiatric illness, particularly in patients with affective disorders,4–8 although the availability of studies longitudinally measuring symptoms before and after pandemic onset note little to no effect on psychiatric symptoms or suicide.16
Limitations. The significance of these findings is limited by the small sample size and convenience sampling, which lacks power and representability to draw extensive conclusions. Our utilization of a cross-sectional design and lack of longitudinal measures might have limited the accuracy of our results concerning changes in symptoms, as previously noted. Response bias might have been present, given that the survey was interviewer-administered and sensitive information was being collected. However, these limitations are mitigated by the fact that we were able to replicate and extend our previous findings with the inclusion of a non-SMI control sample of clinical trial participants, which validated previous observations regarding the robust use of protective measures by clinical trial participants with SMI. While it remains possible that, due to differences in frequency of outpatient care and resources, our findings in clinical trial participants with SMI might not be generalizable to the majority of patients with SMI who do not participate in clinical trials, it is encouraging that our findings are consistent with the results of studies in non-clinical trial patients with SMI.
Conclusion
The findings of this study demonstrate the ability of stable outpatients with SMI to protect themselves from COVID-19 infection and illness through the robust use of precautionary measures, medical services, and vaccination in both the clinic and research settings, despite evidence of pandemic-induced stress, exacerbation of psychiatric illness, increased susceptibility to COVID-19 infection, and increased morbidity and mortality from COVID-19 infection observed in the seriously ill psychiatric patient population.5 While our findings are consistent with the majority of reports on pandemic-related effects on stress and symptoms in patients with premorbid psychiatric illness, there is still a need for longitudinally designed studies to prospectively characterize changes in psychiatric symptoms and pandemic-induced stress and their relationship with viral infection, mortality, and suicide risk, with the aim of providing better preventative and protective therapeutic interventions to psychiatrically vulnerable individuals during a pandemic.
References
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542.
- SMI Adviser. What is serious mental illness? https://smiadviser.org/about/serious-mental-illness. Accessed 16 Feb 2023.
- Kozloff N, Mulsant B, Stergiopoulos V, Voineskos A. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr Bull. 2020;46(4):752–757.
- Shinn AK, Viron M. Perspectives on the COVID-19 pandemic and individuals with serious mental illness. J Clin Psychiatry. 2020;81(3):20com13412.
- Fond G, Nemani K, Etchecopart-Etchart D, et al. Association of mental health disorders with mortality among patients with COVID-19 in 7 countries. JAMA Psychiatry. 2021;78(11):1209–1217.
- Li L, Li F, Fortunati F, et al. Association of a prior psychiatric diagnosis with mortality among hospitalized patients with coronavirus disease 2019 (COVID-19) infection. JAMA Netw Open. 2020;3(9):e2023282.
- Nemani K, Li C, Olfson M, et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78(4):380–386.
- Fleischmann E, Dalkner N, Fellendorf FT, et al. Psychological impact of the COVID-19 pandemic on individuals with serious mental disorders: a systematic review of the literature. World J Psychiatry. 2021;11(12):1387–1406.
- Neelam K, Duddu V, Anyim N, et al. Pandemics and pre-existing mental illness: a systematic review and meta-analysis. Brain Behav Immun Health. 2021;10:100177.
- Puangsri P, Jinanarong V, Wattanapisit A. Impact on and care of psychiatric patients during the outbreak of COVID-19. Clin Pract Epidemiol Ment Health. 2021;17:52–60.
- Brosch K, Meller T, Pfarr JK, et al. Which traits predict elevated distress during the COVID-19 pandemic? Results from a large, longitudinal cohort study with psychiatric patients and healthy controls. J Affect Disord. 2022;297:18–25.
- Sole B, Verdolini N, Amoretti S, et al. Effects of the COVID-19 pandemic and lockdown in Spain: comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC STUDY. J Affect Disord. 2021;281:13–23.
- García-Fernández L, Romero-Ferreiro V, Padilla S, et al. The impact on mental health patients of COVID-19 outbreak in Spain. J Psychiatr Res. 2021;136:127–131.
- Lasevoli F, Fornaro M, D’Urso G, et al. Psychological distress in patients with serious mental illness during the COVID-19 outbreak and one-month mass quarantine in Italy. Psychol Med. 2021;51(6):1054–1056.
- Sun Q, Qin Q, Basta M, et al. Psychological reactions and insomnia in adults with mental health disorders during the COVID-19 outbreak. BMC Psychiatry. 2021;21(1):19.
- Dickerson F, Katasafanas E, Newman T, et al. Experience of persons with serious mental illness during the COVID-19 pandemic. Psychiatr Serv. 2022;73(2):133–140.
- Pinkham AE, Ackerman RA, Depp CA, et al. A longitudinal investigation of the effects of the COVID-19 pandemic on the mental health of individuals with pre-existing severe mental illnesses. J Psychiatr Res. 2020;294:113493.
- Pan KY, Kok AAL, Eikelenboom M, et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety or obsessive-compulsive disorders. Lancet Psychiatry. 2021;8(2):
121–129. - Hölzle P, Aly L, Frank W, et al. COVID-19 distresses the depressed while schizophrenic patients are unimpressed: a study on psychiatric inpatients. Psychiatry Res. 2020;291:113175.
- Maneepongpermpoon P, Pitanupong J. Knowledge, risk perception, precautionary behavior and level of worry towards the 2019 coronavirus disease (COVID-19) among psychiatric outpatients. Siriraj Med J. 2020;73(1):1–9.
- Pinkham AE, Ackerman RA, Depp CA, et al. COVID-19-related psychological distress and engagement in preventative behaviors among individuals with severe mental illnesses. NPJ Schizophr. 2021;7(7).
- Zhu JH, Li W, Huo XN, et al. The attitude towards preventative measures and knowledge of COVID-19 inpatients with severe mental illness in economically underdeveloped areas of China. Psychiatr Q. 2021;92(2):683–691.
- Garcia-Rada M, Litman RE. Impact of COVID-19 pandemic on psychiatric patients at clinical trial sites. Innov Clin Neurosci. 2022;19(10–12):24–28.
- Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalence’s and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976.
- Zhu Y, Li Y, Xu X. Suicidal ideation and suicide attempts in psychiatric patients during the COVID-19: a systematic review and meta-analysis. Psychiatry Res. 2022;317:114837.





