Innov Clin Neurosci. 2016;13(7–8):15–16.
 Dear Editor:
Dear Editor:
Borderline personality disorder (BPD) is over-represented in prison populations, with 25 to 50 percent of incarcerated individuals suffering from this disorder.[1] As an empirical illustration of this association, Sansone et al[2] reported correlations of 0.32 and 0.47 between 27 criminal behaviors and two measures of BPD. Given these evolving associations between criminal behavior and BPD, no study to date has compared the strength of these associations among more than two assessment measures for BPD in a less criminally inclined sample (e.g., psychiatric inpatients)—the focus of the current study.
Potential participants comprised 167 men and women admitted to an inpatient psychiatric facility in the United States. Exclusion criteria were informally assessed by the recruiter (D.A.S.) and included intellectual, medical, psychiatric, or cognitive impairment of a severity to impair the individual’s ability to complete a survey. A total of 14 individuals were excluded from participation (3 with vision problems, 4 intellectually disabled/illiterate, 4 psychotic, 3 malingering). Of the candidates approached, 145 (95%) agreed to participate: 55 men and 89 women (one participant declined to report gender), with a mean age of 38.06 years (standard deviation [SD]=13.06). The majority self-identified as “White” (74%), with 16 percent “Black” and 10 percent of other ethnicities. The majority (87%) had at least completed high school, with 39 percent reporting a four-year college degree or higher. Approximately 41 percent reported never having been married, with 18 percent married, 27 percent divorced, 10 percent separated, and three percent widowed.
Upon admission, all participants were invited to complete a survey, which contained four measures for BPD. The elements of informed consent were provided on the cover page of the survey, and completion of the survey was assumed to function as informed consent (stated on the cover page). The project was approved by the sponsoring hospital’s institutional review board.
The first of the four measures was the Self-Harm Inventory (SHI), which is a 22-item, yes/no, self-report inventory designed to index deliberate self-harm behaviors3 and assess symptoms of BPD.[3,4] Cronbach’s alpha was 0.81.
The second measure for BPD was the borderline personality scale of the Personality Diagnostic Questionaire-4 (PDQ-4),[5] which is a 9-item, true/false, self-report questionnaire that reflects the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria for the disorder.[6] Cronbach’s alpha was 0.74
The third measure for BPD was the McLean Screening Inventory for Borderline Personality Disorder (MSI-BPD),[7] which is a 10-item, yes/no, self-report measure that explores BPD symptomatology. Cronbach’s alpha was 0.78.
The final measure for BPD was the 15-item BPD scale of the Structured Clinical Interview for DSM-IV Axis II Disorders–Personality Questionnaire (SCID-II-PQ),[8] which is a 120-item, true/false, self-report questionnaire that assesses each personality disorder in the DSM-IV.[6] Cronbach’s alpha was 0.86.
The survey also included a measure of criminal behavior, the Antisocial Behavior Questionnaire (ABQ),[9] which is a 16-item, yes/no, self-report checklist that explores a range of 16 nonviolent (e.g., drunk driving, shoplifting, drug trafficking) and violent (e.g., assault, robbery, rape) criminal behaviors. Cronbach’s alpha was 0.87.
As for analyses, we calculated zero-order correlations between the four BPD measures and the ABQ total score as well as the 16 individual behaviors (Table 1). A Bonferroni-corrected alpha of 0.003 (0.05/17.0) was used for each BPD measure to indicate statistical significance. In addition, Steiger’s t-test for dependent correlations[10] was used to examine differences in correlation magnitude across the four measures.
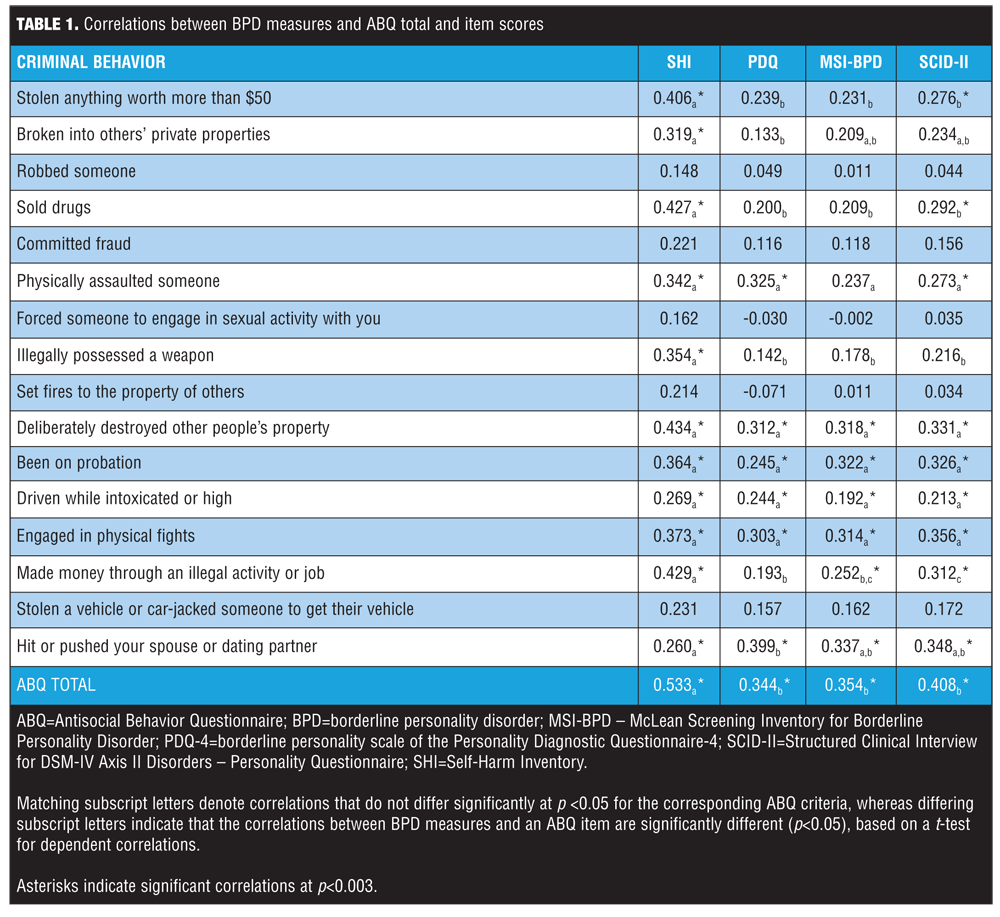
Overall, while all BPD measures evinced significant correlations with the ABQ total score, the SHI correlation was associated with the largest magnitude. With respect to individual behaviors, the BPD measures were typically associated with a range of non-violent and violent acts, except some of the most severe (and thus, less frequent [<10%]) behaviors (arson, rape, robbery, fraud, car-jacking). In all but one instance, where differences existed in correlation magnitudes, the SHI outperformed the other BPD measures. The lone exception was for domestic violence, for which the other BPD measures evinced a larger association relative to the SHI.
According to measures in this study, BPD is moderately to strongly associated with a range of criminal behaviors among psychiatric inpatients, likely owing to these individuals’ extreme proclivity toward disinhibition and poor emotional regulation. Compared with the other measures, the SHI, which is a more behaviorally oriented measure, typically performed better, such that higher scores were likely to be a more reliable indicator of overt criminal risk. For clinicians, findings indicate that higher scores on the SHI should invite further queries into past antisocial behavior.
The potential limitations of this study include the small sample size, lack of confirmation of endorsed antisocial behaviors, and use of self-report measures for BPD (i.e., risk of false positives). Given these potential limitations, this study expands our understanding of the evolving relationship between criminality and BPD.
References.
1. Sansone RA, Sansone LA. Borderline personality and criminality. Innov Clin Neurosci. 2009;10(6):16–20.
2. Sansone RA, Lam C, Wiederman MW. The relationship between illegal behaviors and borderline personality symptoms among internal medicine outpatients. Compr Psychiatry. 2012;53:176–180.
3. Sansone RA, Wiederman MW, Sansone LA. The Self-Harm Inventory (SHI): development of a scale for identifying self-destructive behaviors and borderline personality disorder. J Clin Psychol. 1998;54:973–983.
4. Sansone RA, Sansone LA. Measuring self-harm behavior with the Self-Harm Inventory. Innov Clin Neurosci. 2010;7(4):16–20.
5. Hyler SE. Personality Diagnostic Questionnaire, PDQ-4. New York: New York State Psychiatric Institute; 1994.
6. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Press, Inc.; 1994.
7. Zanarini MC, Vujanovic AA, Parachini EA, et al. A screening measure for BPD: the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD). J Pers Disord. 2003;17:568–573.
8. First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II). Washington, DC: American Psychiatric Press, Inc; 1997.
9. Sellbom M, Ben-Porath YS, Patrick CJ, et al. Development and construct validation of MMPI-2-RF indices of global psychopathy, fearless-dominance, and impulsive-antisociality. Personal Disord. 2012;3:17–38.
10. Steiger JH. Tests of comparing elements of a correlation matrix. Psychol Bull. 1980;87:245–251.
With regard,
Randy A. Sansone, MD; Martin Sellbom, PhD; and Douglas A. Songer, MD
Dr. Sansone is a Professor Emeritus in the Departments of Psychiatry and Internal Medicine at Wright State University School of Medicine in Dayton, Ohio, and previous Director of Psychiatry Education at Kettering Medical Center in Kettering, Ohio; Dr. Sellbom is an Associate Professor in the Research School of Psychology at The Australian National University in Canberra, Australia; and Dr. Songer is an Associate Professor in the Department of Psychiatry at Wright State University School of Medicine in Dayton, Ohio, and affiliated with Premier Health Partners in Dayton, Ohio.
Funding/financial disclosures.
The authors received no funding nor have any conflicts of interest relevant to the content of this letter.


