by Rocco Salvatore Calabrò, MD, PhD; Giuseppe Gervasi, MD, PhD; Antonino Naro, MD, PhD; Rosaria De Luca, PhD; Michelangelo Marullo, MD; and Placido Bramanti, MD
by Rocco Salvatore Calabrò, MD, PhD; Giuseppe Gervasi, MD, PhD; Antonino Naro, MD, PhD; Rosaria De Luca, PhD; Michelangelo Marullo, MD; and Placido Bramanti, MD
Drs. Calabró, Naro, de Luca, Marullo, and Bramanti are with the IRCCS Centro Neurolesi “Bonino Pulejo” in Messina, Italy; and Dr. Gervasi is with the Torvergata University in Rome, Italy.
Innov Clin Neurosci. 2016;13(1–2):10–14.
Funding: No funding was received for the preparation of this manuscript.
Financial Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Key Words: Neurogenic ED, erectile dysfunction, sexual health, quality of life
Abstract: Objective: Neurogenic erectile dysfunction can be broadly defined as an inability to sustain or maintain a penile erection due to neurologic impairment. Sexual problems can occur due to any lesion affecting the central and peripheral nervous system. The aim of this study was to evaluate the prevalence and causes of erectile dysfunction in a group of hospital inpatients suffering from neurologic disorders. Methods: Three-hundred and twenty six male patients admitted to the Neurorehabilitation Unit of IRCCS Centro Neurolesi “Bonino-Pulejo” in Messina Italy from March 2012 to June 2013 were screened for erectile dysfunction using the International Index of Erectile Function questionnaire. The patients who reported erectile dysfuntion underwent vascular, neurophysiological, and hormonal testing, and were divided into two groups according to their lesion sites: G1 (lesions above the S2–S4 center) and G2 (lesions below the S2–S4 center). Results: Of the 326 admitted patients, 126 patients (38.6%), mean age of 54.56±11.74 years (age range 27–82 years), were affected by erectile dysfunction (i.e., scored ?21 on the questionnaire). A statistically significant correlation between International Index of Erectile Function questionnaire scores and location of the neurologic lesions was observed in G2 (r=0.22) with an increased risk of erectile dysfuntion of around 2:1 (odds ratio=1.87) without influences related to aging. Conclusion: The occurence of erectile dysfunction is significantly more prevalent among neurologically disabled men, particularly those with lesions below S2–S4, than among men without neurologic disability. Considering the prevalence of erectile dysfunction among neurologically disabled men, sexual functioning should be regularly evaluated during acute and long-term rehabilitation, and any existing sexual dysfunction should be addressed in the treatment plan.
Introduction
Penile erection is a neurovascular event characterized by the dilation of arteries that cause the corpora cavernosa and corpora spongiosum of the penis to fill with blood; simultaneously, the ischiocavernosus and bulbospongiosus muscles compress the veins of the corpora cavernosa, which prevents the blood from exiting. Erectile function requires the participation of autonomic and somatic nerves (i.e., sacral parasympathetic [pelvic], thoracolumbar sympathetic [hypogastric and lumbar chain], and somatic [pudendal] nerves), with the hypothalamic and limbic pathways playing significant roles. Several medical conditions, beyond aging per se, are associated with erectile dysfunction (ED).[1,2]
Neurologic ED can be broadly defined as an inability to sustain or maintain a penile erection, owing to central and/or peripheral neurologic impairment. Neurologic disorders can change the processing of sexual stimuli to preclude arousal, to decrease or increase desire, or to curtail genital engorgement, since the interruption of the long spinal tracts between the cortex and sacral cord and/or the pelvic autonomic nerves interferes with genital engorgement, climax, and ejaculation.[3]
Neurologic diseases can also challenge the physical ability of the individual to embrace, stimulate, engage in intercourse, and maintain urinary and bowel continence during sexual activity. All these factors may lead to a primary or secondary neurogenic ED. Thus, a proper diagnostic work-up that includes patient history, physical examination, and laboratory testing to determine sexual hormone levels, evaluate pudendal nerve somatosensory-evoked potential (pSEP) and bulbospongiosus reflex, and evaluate penile blood flow via a penile Doppler ultrasound are needed in all patients affected by neurologic disorders.[4,5] Notably, medication history plays an important role since there are many drugs commonly used in neurologic patients, such as antidepressants, neuroleptics, sedatives, beta blockers, and diuretics, that can lead to sexual side effects.
Several studies[6–8] have demonstrated how medical conditions affecting vascular functioning (e.g., diabetes, local atheromatous plaques) are associated with ED, but to date, few studies have explored the effect of neurologic diseases on ED,[9] particularly in patients attending a neurorehabilitation ward. Moreover, although sexual dysfunction is common in male patients with neurologic disorders, its quantification is limited by the paucity of validated, user-friendly scales.[10] The aim of this study was to evaluate the prevalence of ED in a group of inpatients attending a rehabilitation ward due to neurologic disabilities, as well as to investigate the main organic causes of ED and its relationship with the neurologic lesion site.
Materials and Methods
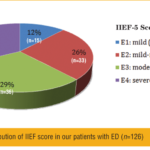
All male patients who attended the Neurorehabilitation Unit of IRCCS Centro Neurolesi “Bonino-Pulejo” in Messina from March 2012 to June 2013 were screened for ED using the International Index of Erectile Function (IIEF)-5.[11] Patients were affected by different neurologic disorders, including brain (i.e., stroke, traumatic brain injury, and multiple sclerosis), spinal (i.e., traumatic and vascular), and peripheral nerve (i.e., compressive, diabetic) pathologies. The IIEF-5 is a self-administered, five-question tool that explores different sexuality aspects related to erection. Each of the five questions is answered by the patient using a 1 to 5 scale (1=very low, 2=low, 3=moderate, 4=high, 5=very high), so that the level of ED may be divided into mild (17–21 points), mild-moderate (12–16 points), moderate (8–11 points), and severe (5–7 points).
Based on the results of the IIEF-5 questionnaire, patients who reported ED were enrolled in our study and were subdivided into two groups according to the location of neurologic damage: G1 included patients with lesions over the sacral spine center [S2–S4]) and G2 included patients with lesions below S2–S4, including the peripheral nerve.
All study subjects gave informed consent, and the study protocol was approved by our clinic’s institutional review board.
All enrolled patients underwent p-SEP to investigate the physiological nervous mechanism of their erectile functioning, and echo-color-Doppler examination of the penile arteries to exclude possible vascular and blood flow abnormalities in the corpora cavernosa. Testosterone and prolactin blood levels were also evaluated.
Statistical analysis was conducted using SPSS 21v software. The differences between the two groups according to the location of the neurologic lesions, subject age, p-SEP and Doppler results, and hormone levels were analyzed using the chi-square test. A multimodal regression analysis to study the relationships among the IIEF scoring, the neurologic lesion location, and subject age was also done. Statistical significance was set at a P<0.05.
Results
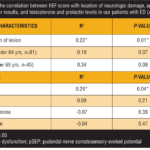
Three-hundred and twenty-six male patients were admitted to our clinic from March 2012 to June 2013 and were administered the IIEF-5. Out of these patients, 126 individuals (38.6%), with a mean age of 54.56±11.74 years (age range 27–82), reported ED (scoring ?21 on the IIEF-5). Eighty-eight of the subjects with ED (69.8%) were in stable relationships. None of the subjects with ED reported any psychiatric issues (e.g., depression). Out of the 126 subjects with ED, 100 (79.3%) had supra-sacral lesions and 25 (19.8%) had lesions involving the lower motor neuron. The distribution of the subjects with ED according to their IIEF-5 scores is shown in Figure 1, with the greatest number of patients having either “moderate” (n=36) or “severe”(n=42) ED. However, a higher range of ED severity was observed in the G2 group (i.e., in those subjects with peripheral nerve disorders or sacral lesions). In other words, in the G1 group, one subject (4.2%) had mild ED and 14 (58.3%) had severe ED, and in the G2 group, 14 subjects had mild ED (13.7%) and 27 had severe ED (26.5%). A positive trend (p=0.01) was demonstrated in the presence of altered p-SEP parameters, with the lowest prevalence (5.9%) in those subjects with “mild” ED and the highest in those with “severe” ED (64.7%). Twenty-two patients with ED (17.4%) had alterations in penile blood flow, with no statistical difference between G1 and G2 groups. No differences were found regarding age or hormonal status between the two groups. A statistically significant correlation between the IIEF score and the location of the neurologic lesion was observed (r=0.22, Table 1), with an increased risk of 2:1 (odds ratio [OR]=1.87) for ED in patients with lesions under the Onuf sacral center (S2–S4) and without influences related to age, as shown by the multimodal regression model. Moreover, we found a positive correlation (r=0.29) between the G2 patients and their IIEF scores.
Discussion
ED is a highly prevalent problem that increases with age among men. In 2010, the Italian National Community of Andrology estimated ED to be prevalent in 13 percent of healthy male volunteers aged 20 to 85, with its frequency increasing from two-percent prevalence in men under 35 years to 48-percent prevalence in men over the age of 70 years.[12] These data are in line with other epidemiological studies, including the Cologne Male Survey[13] and the Massachusetts Male Aging Study,[14] with a 19.2-percent and a 40-percent prevalence rate, respectively.
In our relatively young sample (mean age 54 years) of men with neurologic disease, we found a 38.6-percent (n=48) prevalence of ED, which is significantly higher than the average worldwide prevalence of 20 percent,[12–14] highlighting the negative impact a disabling neurologic disorder can have on erectile function. Interestingly, moderate to severe ED was found in more than half of our subjects with ED, and seemed to be more related to damage to the peripheral nervous system than to the central nervous system.
Nonetheless, sexual problems can be caused by any lesion affecting the central or peripheral nervous systems. Epilepsy, demyelinating disorders, brain or spinal cord injuries, and their treatments can often cause ED and/or ejaculation dysfunctions and affect sexual desire.[9] Peripheral ED can be secondary to the disruption of sensory nerves that bring local information to the brain or to the disruption of autonomic nerves that mediate arterial dilatation and trabecular smooth muscle relaxation. Central origins of ED can be caused by a lack of excitation as well as increasing inhibition of central autonomic pathways.[15] The most significant cause of ED in the general world population is spinal cord injury,[3] and its level of severity can be affected by the location of the lesion. According to our own research,[3] in individuals with upper motor neuron lesions, 95 percent are capable of reflexogenic erection, while in those with lower motor neuron lesions only 25 percent can achieve psychogenic erection. Moreover, more than 90 percent of the individuals with an incomplete lesion retain erectile function.[3]
Many authors[16,17] report that ED is mainly due to organic conditions (including aging) that alter the normal physiology of the corpora cavernosa. ED has been largely attributed to local vascular impairment.[17] Indeed, many urologists and andrologists consider ED caused by peripheral neuropathy to be an iatrogenic complication of bladder, prostate, or rectal surgery.[19–22] Unfortunately, ED in patients with neurologic disorders is often neglected by their treatment team, which can lead to negative management implications.[18]
Individuals with neurologic disorders, especially young men, might consider sexual loss as the most devastating aspect of their disorder.[24] The quality of an individual’s personal relationships, sexual ones in particular, exerts great impact on his or her self-esteem and support network.[25] Entrenched socio-cultural beliefs can create significant barriers that may prevent individuals with neurologic disabilities from exploring their sexuality, and these false beliefs may be more disabling than the physical impairment itself.[24,25] When a sexual encounter results in frustration and stress rather than gratification, a vicious psychoneuroendocrine cycle of distress and depression with a consequent ED may occur.[23]
Although we did not evaluate the psychological component of sexual dysfunction in our group, we believe that adequate psychological counseling should be part of the treatment plan to help patients with neurologic disabilities and their partners regain intimacy.
Limitation. We believe that the ED in the subjects of our study was mostly related to neurologic disorders, as other causes of ED (e.g., vascular, endocrine-metabolic abnormalities) were ruled out through proper investigation. However, although the use of psychotropic drugs in our sample was low (20%), we did not study the impact these medications may have had on our subjects’ sexual functioning, which limits our conclusion.
Conclusion
Our study suggests that the occurence of ED is significantly more prevalent among neurologically disabled men, particularly those with lesions below S2–S4, than among men without neurologic disability. We believe it is important for clinicians to recognize that people with neurologic disabilities have sexual desires, and any concerns these individuals have regarding their sexual functioning should be thoroughly addressed by their healthcare providers. The recovery of sexual function is no less important to these patients than any other aspect of functional rehabilitation from a disabling disease or injury.[24] Too often, physicians do not consider sexuality to be as important as the injury or illness that brought the patient to the rehabilitation clinic.[18] However, we believe that all of the physical, psychological, and emotional changes that occur after a neurologic injury should be addressed by the rehabilitation team. Considering the prevalence of ED among neurologically disabled men and the potential negative impact it can have on their quality of life, sexual functioning should be regularly evaluated during acute and long-term rehabilitation, and any existing sexual dysfunction should be addressed in the treatment plan.
References
1. Sáenz de Tejada I, Angulo J, Cellek S, et al. Physiology of erectile function. J Sex Med. 2004;1:254–265.
2. Giuliano F, Rampin O. Neural control of erection. Physiol Behav. 2004;83:189–201.
3. Calabrò RS. Male Sexual Dysfunction in Neurologic Disease, from pathophysiology to rehabilitation. New York: Nova Publisher Inc; 2011.
4. Meuleman EJ, Diemont WL. Investigation of erectile dysfunction: diagnostic testing for vascular factors in erectile dysfunction. Urol Clin North Am. 1995;22:803–819.
5. Diemont WL, Meuleman EJ. Neurologic testing in erectile dysfunction. J Androl. 1997;18:345–350.
6. Foresta C, Caretta N, Corona G, et al. Clinical and metabolic evaluation of subjects with erectile dysfunction: a review with a proposal flowchart. Int J Androl. 2009;32:198–211.
7. Vlachopoulos C, Rokkas K, Ioakeimidis N, Stefanadis C. Inflammation, metabolic syndrome, erectile dysfunction, and coronary artery disease: common links. Eur Urol. 2007;52:1590–1600.
8. Basson R, Schultz WW. Sexual sequelae of general medical disorders. Lancet. 2007;369:409–424.
9. Rees PM, Fowler CJ, Maas CP. Sexual function in men and women with neurologic disorders. Lancet. 2007;369:512–525.
10. Hatzimouratidis K, Amar E, Eardley I, et al. European Association of Urology. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol. 2010;57:804–814.
11. Cappelleri JC, Rosen RC, Smith MD, et al. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54:346–351.
12. Mirone V1, Ricci E, Gentile V, Basile et al. Determinants of erectile dysfunction risk in a large series of Italian men attending andrology clinics. Eur Urol. 2004;45(1):87–91.
13. Braun M, Wassmer G, Klotz T, et al Epidemiology of erectile dysfunction: results of the Cologne Male Survey. Int J Impot Res. 2000;12:305–311.
14. Derby CA, Barbour MM, Hume AL, McKinlay JB. Drug therapy and prevalence of erectile dysfunction in the Massachusetts Male Aging Study cohort. Pharmacotherapy. 2001;21:676–683.
15. Calabrò RS, Polimeni G, Bramanti P. Recent advances in the treatment of neurogenic erectile dysfunction. Recent Pat CNS Drug Discov. 2014;9:41–53.
16. Papagiannopoulos D1, Khare N, Nehra A. Evaluation of young men with organic erectile dysfunction. Asian J Androl. 2015;17:11–16.
17. Ludwig W, Phillips M. Organic causes of erectile dysfunction in men under 40. Urol Int. 2014;92:1–6.
18. Valles-Antuña C, Fernandez-Gomez J, Fernandez-Gonzalez F. Peripheral neuropathy: an underdiagnosed cause of erectile dysfunction. BJU Int. 2011;108:1855–1859.
19. Krishnan R, Katz D, Nelson CJ, Mulhall JP. Erectile function recovery in patients after non-nerve sparing radical prostatectomy. Andrology. 2014;2:951–954.
20. Wittmann D, Carolan M, Given B, et al. What couples say about their recovery of sexual intimacy after prostatectomy: toward the development of a conceptual model of couples’ sexual recovery after surgery for prostate cancer. J Sex Med. 2015;12:494–504.
21. Attaallah W, Ertekin C, Tinay I, Yegen C. High rate of sexual dysfunction following surgery for rectal cancer. Ann Coloproctol. 2014;30:210–215.
22. Burkhard FC, Studer UE, Wuethrich PY. Superior functional outcome after radical cystectomy with orthotopic bladder substitution with restrictive intraoperative fluid management: a followup study of a randomized clinical trial. J Urol. 2015;193:173–178.
23. Calabrò RS, De Luca R, Conti-Nibali V, et al. Sexual dysfunction in male patients with multiple sclerosis: a need for counseling. Int J Neurosci. 2014;124:547–557.
24. Calabrò RS, Gervasi G, Bramanti P. Male sexual disorders following stroke: an overview. Int J Neurosci. 2011;121:598–604.
25. Aisen ML. Neurologic rehabilitation: sexuality and reproductive health. Handb Clin Neurol. 2013;110:229–237.