
by Tammie Lee Demler, PharmD, MBA, BCGP, BCPP; and Carolyn O’Donnell, PharmD, PGY-2
Drs. Demler and O’Donnell are with the New York State Office of Mental Health at Buffalo Psychiatric Center and State University of New York at Buffalo School of Pharmacy and Pharmaceutical Sciences, Department of Pharmacy Practice in Buffalo, New York. Dr. Demler is with the State University of New York at Buffalo School of Medicine, Department of Psychiatry in Buffalo, New York.
Funding: No funding was received for this article.
Disclosures: The authors have no conflicts of interest relevant to the contents of this article.
Innov Clin Neurosci. 2023;20(1–3):32–38.
Abstract
Objective: Individuals with serious mental illness (SMI) are recognized to be among the highest risk patients to experience more severe symptoms of COVID-19, not only due to poor baseline health and associated disparity, but also due to medications prescribed to manage their illness that are known to compromise immunity even further. Clozapine, a gold standard antipsychotic used in the treatment for refractory schizophrenia, is considered to be the antipsychotic with the greatest risk of compromising immunity due to its potential to cause blood dyscrasia, including leukopenia and rarely, but potentially, agranulocytosis. The objective of this study is to determine if there is any potential hematological consequence for the use of COVID-19 messenger ribonucleic acid (mRNA) vaccines or the impact of active severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in patients receiving clozapine therapy. Since there is controversy over the rate of vaccine hesitancy in patients with SMI, we also examined the rate of vaccine acceptance in our subject population.
Design: This study was a retrospective chart review conducted at a 160-bed state psychiatric inpatient hospital in upstate New York evaluating the impact of COVID-19 vaccination, SARS-CoV-2 infection, and vaccine acceptance in patients prescribed clozapine.
Results: Both the administration of COVID-19 mRNA vaccines and SARS-CoV-2 infection did not appear to significantly influence the hematologic values that are monitored by the United States (US) Food and Drug Administration (FDA) to ensure safe use of clozapine. When offered vaccination, most patients hospitalized for SMI were willing to accept it.
Conclusion: With the likelihood of COVID-19 mRNA vaccinations becoming a recommended routine vaccination, requiring periodic boosters, patients receiving clozapine therapy have been observed to not be at higher risk of adverse hematological consequences when the mRNA vaccine is administered. Furthermore, inpatient psychiatry settings should be considered an optimal site of vaccination to improve vaccination efforts in our communities.
Keywords: Clozapine, SARS-CoV-2 infection, COVID-19 infection, COVID-19 related morbidity, mRNA vaccines, vaccine hesitancy, serious mental illness (SMI), inpatient psychiatric facility
It has been observed that individuals with serious mental illness (SMI) are at higher risk for more severe severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and COVID-19-related morbidity.1 Vaccination has been widely accepted as the best protection against COVID-19, especially in combination with other preventative measures, such as the use of hand hygiene and personal protective equipment (PPE; e.g., wearing masks). Vaccine hesitancy within the mental health community is of great concern, yet research has demonstrated that individuals with SMI are willing to get vaccinated, and their decision of whether or not to get vaccinated is observed to be based on their personal opinion about the vaccine rather than other factors. Thus, it is important for the healthcare team to provide evidence-based education and reassurance for those with contrary opinions, in addition to promoting access to vaccines, to improve vaccination rates.2 Inpatient settings have been identified as a prime target site to offer early access to vaccination, since discharge to outpatient care with plans for later vaccination in the community can pose challenges, such as limited transportation and access to vaccines.
Individuals with SMI, especially schizophrenia, may be more susceptible to COVID-19 due to poor self-care, increased risk of pneumonia, and comorbidities.1 Hospitalized patients diagnosed with SMI are often prescribed medications that may compromise baseline metabolic and immunologic factors. Clozapine, a gold standard second-generation antipsychotic (SGA) intervention used to treat refractory schizophrenia, is associated with an increased risk of blood dyscrasia that, in rare cases, may lead to agranulocytosis, and therefore requires risk evaluation mitigation strategies (REMS) to ensure safe use. Patients with schizophrenia spectrum disorders (SSDs) using clozapine may have a higher risk of infection than patients using other antipsychotics, and for patients who are infected, clozapine intoxication, pneumonia, and delirium are reported complications of COVID-19.3 Pharmacotherapeutic interventions to treat COVID-19 remain problematic for patients taking clozapine due to potential drug-drug interactions, so prevention and mitigation with vaccination continues to be the preferred strategy.4
A literature review conducted via EMBASE and MEDLINE from 1975 to 2021 examined the relationships among clozapine, serious mental illness, SARS-CoV-2 infection, COVID-19, COVID-19-related morbidity, and inpatient psychiatric facilities. At the beginning of the COVID-19 pandemic, clinicians raised concerns about continuing clozapine treatment, not only because of the challenges in meeting the REMS blood monitoring requirements with lockdowns, mandatory quarantine with isolation, and efforts to minimize personal contact between patients and healthcare providers, but also because of the leukopenic potential associated with clozapine that could potentially be exacerbated by infection.3 Lymphopenia, but not neutropenia, was commonly reported in 83 percent of patients in a case series of more than 1,000 patients in China.5 However, neutrophilia is now considered to be an early indication of potential COVID-19 infection, predicting a more severe disease course.6,7
Bonaccorso et al8 retrospectively explored a case series of 10 psychiatric inpatients who were also diagnosed with COVID-19 to determine whether there was an increased risk of neutropenia in these patients. Using a linear regression model to estimate whether there was a significant drop in the neutrophil count during SARS-CoV-2 infection, they evaluated data collected from 10 patients, seven of whom were male, which demonstrated that there were significant drops in average neutrophil count (ANC) from baseline, with the mean relative reduction in ANC being -0.2729 (standard deviation [SD]: 0.1666), and ANC values during SARS-CoV-2 infection were 83.77 percent of the baseline ANC. These values continued to decrease to 95 percent of observed baseline, even roughly a month after resolution of the infection. The authors concluded that a significant drop in patient neutrophil count may occur in patients taking clozapine who contract SARS-CoV-2 infection. However, the drop they observed was only temporary.8 Tomita et al9 reported two cases of what they described as neutropenia induced by COVID-19 vaccination in patients who had been receiving clozapine for a number of years.9
Pereira et al10 describe the case of a patient diagnosed with schizophrenia who had been taking clozapine for 14 years who tested positive for COVID-19 but remained asymptomatic throughout his quarantine. The patient developed late-onset agranulocytosis, which resolved after clozapine was discontinued; however, the authors were unable to determine whether clozapine or COVID-19, either separately or in combination, was responsible for the genesis of the severe granulocytopenia. They reported that the decrease of white blood cells (WBCs) began two months before the patient tested positive for COVID-19, and the progressive granulocytopenia became even more severe with the co-occurrence of COVID-19.10
Clozapine use has been associated with increased annual utilization of antibiotics and significantly reduced immunoglobulin levels, which may contribute to increased rates of pneumonia and sepsis-related mortality.11 While there is debate over the potential increased risk of patients who use clozapine experiencing COVID-19 infection, there are preliminary observations that report a protective effect of clozapine, with less risk of infection and less symptom severity, when compared to other antipsychotics, such as haloperidol. These findings should be considered with caution, as more studies with greater numbers of patients in diverse settings are needed in order to potentially generalize the results.12
Clozapine by itself can cause inflammation, particularly during titration that is too rapid for sensitive patients. Clozapine may increase the risk of infection and is thought to be more strongly associated with the risk of pneumonia, which is linked to high mortality rates in patients around the world who use clozapine.13
The trajectory of the neutrophil lifespan and level of activity may be altered by both infection and neutropenia. When the immune system initially identifies an infection, cytokines release signals for neutrophils and macrophages circulating in the plasma to migrate to the area of infection. In experimental models, this resulted in an initial decrease in plasma concentrations of neutrophils and macrophages, which reached their nadir on Day 1.14,15 Typically, there is an initial decrease of circulating neutrophils seen in the first stage of bacterial infections, which is later offset by a rise in neutrophil concentrations in response to increasing bacteria counts, peaking at four days postinfection. Reduction in neutrophil release from bone marrow occurs as the bacterial load from the initial infection begins to decrease. This typically occurs seven days after the onset of infection.14,15
Gee et al1 evaluated whether the reduction in WBCs, driven by lower levels of lymphocytes that have been observed with COVID-19 infection, may result in neutropenia in patients receiving clozapine at the time of infection. To date, neutropenia during COVID-19 has not been reported.1 Through a retrospective review of 56 patients who were taking clozapine at the time they tested positive for COVID-19, the authors reported observed reductions in ANC (p=0.005), lymphocyte counts (p=0.003), and WBC counts (p<0.001) between baseline and the first seven days of COVID-19 infection. However, cell counts had returned to baseline levels by Days 8 to 14. Six patients (11%) experienced neutropenia, which was defined as ANC of less than 2.0×109/L, and of those six patients, four discontinued clozapine therapy due to reaching a neutropenic threshold severe enough to require mandatory cessation of clozapine. The data presented strongly suggests that mild neutropenia experienced during COVID-19 infection in patients who are well established on clozapine is more likely associated with the virus, rather than being a consequence of clozapine treatment.1
Clozapine serum concentrations can also be influenced by a variety of factors, including interpatient pharmacogenomic differences; pharmacokinetic (PK) complications, including drug interactions; and physiologic influences of inflammation and infection. Davis et al16 described a case of acute infection leading to significantly increased clozapine concentrations that resulted in toxicity and appeared to be the first indication of severe medical illness. Elevated clozapine levels are consistent with infection-related inflammation inhibiting cytochrome P450 1A2 (CYP1A2) and diminished clozapine metabolism. Case studies indicate that COVID-19 can be associated with toxic clozapine levels, requiring monitoring to maintain therapeutic levels and judicious dose adjustments to prevent relapses of psychosis.17–20 Systemic inflammation can increase clozapine levels, but little, if anything, is known about the impact of vaccination on clozapine serum concentrations.13 Bayraktar et al21 reported that COVID-19 infection-related clozapine intoxication could induce postinfection cytokine release, downregulating the metabolism of clozapine in the CYP450 system. It was hypothesized that COVID-19 vaccination could induce the same effect on clozapine concentration that is observed in active infection, and that messenger ribonucleic acid (mRNA) COVID-19 vaccines resulted in strong cluster of differentiation (CD) 4-positive (+) and CD8+ cell and antibody responses that lead to the production of cytokines, such as interferon (IFN)-gamma, which could decrease the efficacy of CYP1A2 and CYP3A4 isoenzymes and potentially result in elevated serum concentration of clozapine.21
The literature discussed above asserts that the potential of elevated serum concentration of clozapine would likely result in unplanned treatment cessation, due to the emergence of what could be considered exaggerated clozapine side effects resulting from possible CYP downregulation. Thus, relapse in psychotic symptoms may occur as a result of withdrawal of clozapine. Therefore, it is recommended that, following COVID-19 vaccine administration, clinicians should monitor ANC and clozapine serum concentrations closely in patients using clozapine and be mindful of the potential PK consequences.
Vaccine hesitancy in SMI. Despite the expected heightened risk of SARS-CoV-2 infection and COVID-19-related morbidity and mortality in patients with a diagnosis of mental illness, vaccine acceptance and hesitancy in this population has been largely unknown, especially in earlier stages of the COVID-19 pandemic. In an effort to provide some insight, Shahani et al22 shared their institutional successes on vaccine outreach in the University of Texas Health Harris County Psychiatric Center (HCPC), a 274-bed, freestanding, safety-net, inpatient psychiatric hospital, considered to be the largest provider of inpatient psychiatric care in the Houston metropolitan area. Between March 29, 2021, and May 21, 2021, a total of 418 adult patients were offered the COVID-19 vaccine; however, only 198 (47%) accepted the first dose. The demographic majority of HCPC patients who were offered the vaccine were male (63%, n=266), younger than the age of 50 years (85%, n=354), admitted involuntarily (65%, n=273), and had completed less than a high school education (57%, n=236). A vaccine hesitancy survey revealed that common reasons for refusal included preference to wait and see what other people do (64%, n=16), lack of trust in the pharmaceutical industry (64%, n=16), lack of trust in media for information on the vaccine (64%, n=16), and being concerned about risks associated with the COVID-19 vaccine (60%, n=15). It is important to note that 92 percent (n=23) of these patients expressed concern about COVID-19 illness, and 76 percent (n=19) expressed trust in their physicians to talk about the risks and benefits of vaccines.22
Design and Methods
Through retrospective analysis, the blood panels of all inpatients prescribed clozapine who received the COVID-19 mRNA vaccine and met inclusion criteria (n=26) at an inpatient state psychiatric facility were assessed. This study was approved by the Institutional Review Board (IRB) through the New York State Office of Mental Health. Patients at a state psychiatric facility in Western New York were included in the study if they were prescribed clozapine during their inpatient stay during October 2020 through December 2021 and received the COVID-19 vaccine. Patients were excluded from the study if they had a criminal procedure law designation (CPL), were initiated on clozapine only after receiving both vaccinations, or did not receive either vaccination.
Results
We did not see any increased risk of infection or severity of medical illness in our subjects. Of the 26 patients in the study, only one patient was COVID-19-positive during their inpatient hospital stay, but the patient was asymptomatic and did not require acute intervention. Although serum concentrations were not routinely monitored, we did observe 10 dose changes that occurred during the period of vaccine administration; however, half of those changes were dose decreases. The need for decreased doses could be interpreted as a potential COVID-19 mRNA vaccine-induced CYP downregulation and subsequently increased serum concentrations of clozapine, resulting in exaggerated medication effects requiring dose adjustment (Table 1). All dose increases were observed in weekly and biweekly patients, as would be expected with newly initiated clozapine regimens. Dose changes, including titrations, along with the increased risk of neutropenic changes are most likely to occur in the first few months of treatment, but the magnitude of the intended dose titration could have been theoretically flattened with CYP downregulation. Thus, the possibility of this PK impact cannot be excluded, even in the remaining five patients who received dose increases. We continued to report dose changes that were observed, highlighting the patient who experienced the greatest number of clozapine dose changes reported by date, designated by monitoring frequency (Tables 2 and 3).

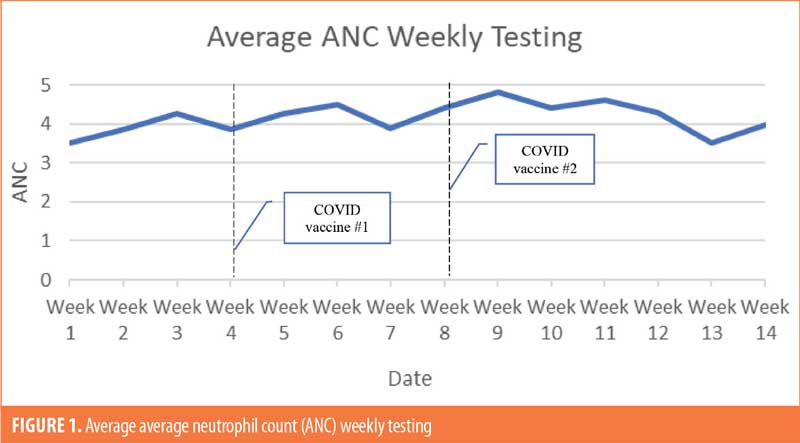
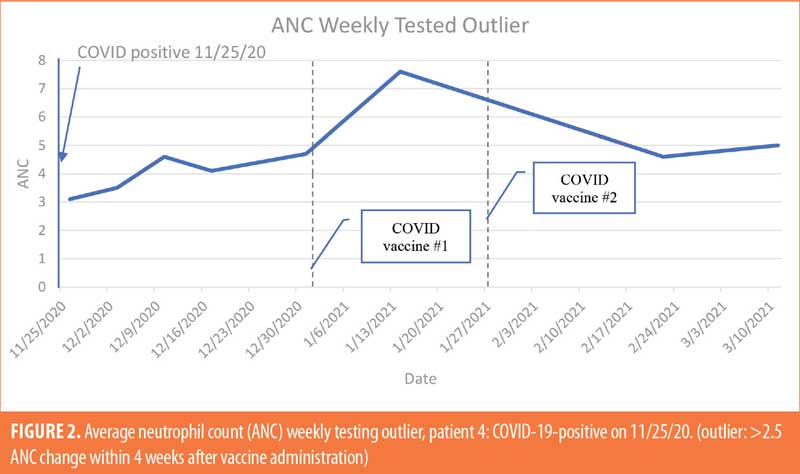
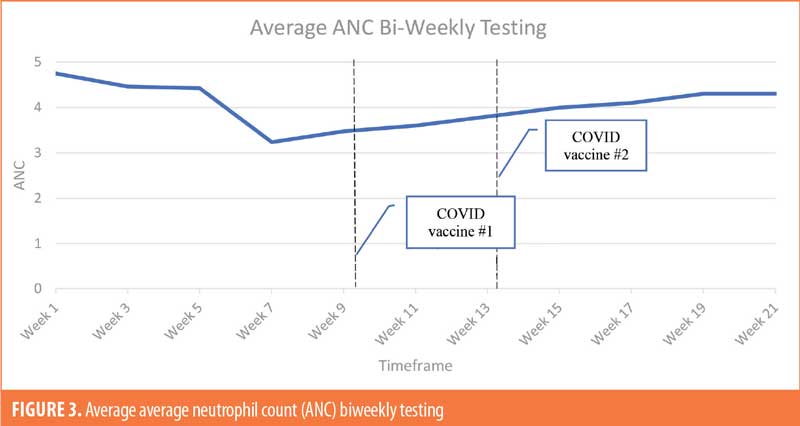
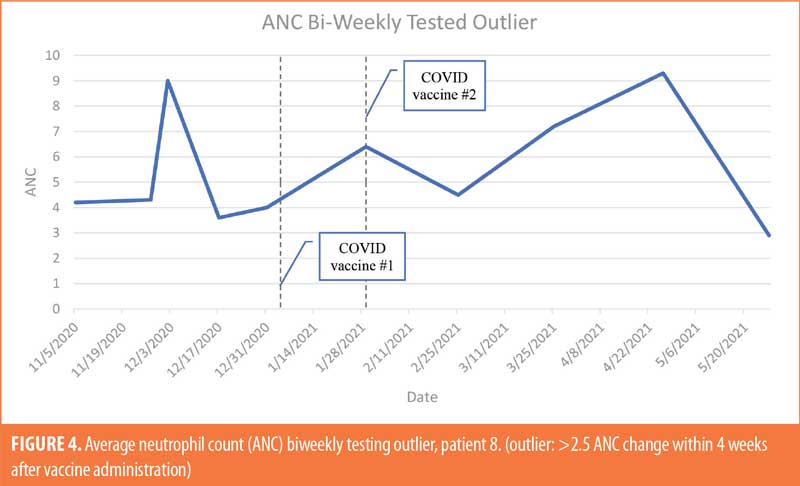
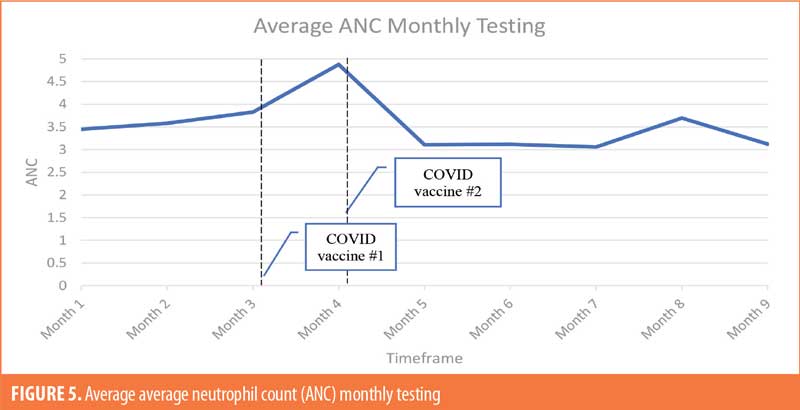
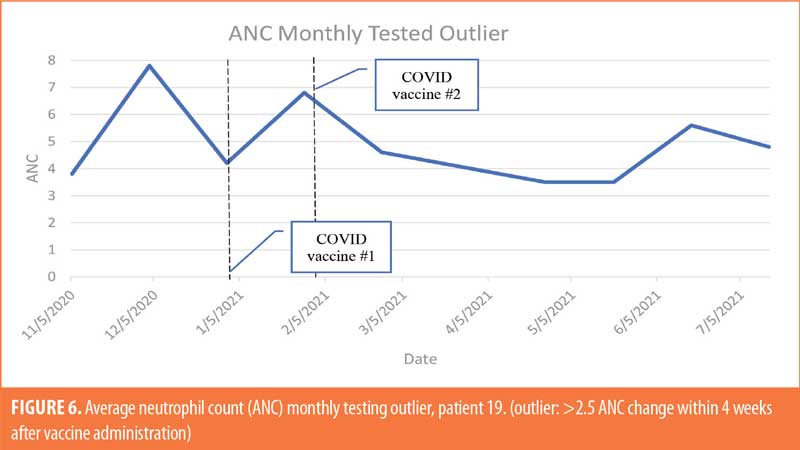
The patient population (Table 4; n=26) was 35-percent female and 65-percent male. The majority of patients were White (69%), 19 percent were Black, and 12 percent were not specified. The majority of patients were of non-Hispanic ethnic origin (n=24) with the remaining patients not specified but not Hispanic (n=2). The patients included in the study ranged in age from 22 to 71 years old, with the greatest number of patients being aged 60 years or older (n=11). For ANC testing, there were six patients receiving weekly ANC testing, eight patients receiving biweekly ANC testing, and 12 patients receiving monthly ANC testing (Figures 1–6). Three of the patients in our patient population were identified as hematologic outliers, with a magnitude of ANC change greater than 2.5 observed within four weeks of vaccine administration. These three patient outliers were evenly divided into groups of clozapine monitoring frequencies; one monthly, one biweekly, and one weekly patient, with the weekly patient outlier having tested positive for asymptomatic COVID-19 infection during this time (Figure 2). Table 5 shows the dates of vaccination for each patient.
Of the patients initially reviewed for the study (n=62) who were taking clozapine, eight patients were excluded from the study for refusing the vaccine, which means there was a 90-percent patient acceptance rate of the COVID-19 vaccine. Of the eight patients who did not receive the vaccine, five were discharged, and we were unable to provide additional educational opportunities in regard to the importance of the COVID-19 vaccine prior to discharge. There were 12 patients excluded due to not having ANC values before or after their COVID-19 vaccine or having gaps in ANC values due to discharges to other facilities.
Discussion
Based on the data collected at a state inpatient psychiatric facility in upstate New York, the majority of patients, even those taking a large pill burden, were at low risk of increased vulnerability to dyscrasia when COVID-19 mRNA vaccines were administered. It was also evident that our inpatient facility was an ideal vaccination provider and patients are at an advantage when offered early access to safe and efficacious vaccines. Considering that transportation and access to vaccinations in outpatient care could be a challenge for patient populations with SMI, inpatient psychiatric settings could be a site of vaccination to improve vaccination efforts in the community.
Limitations
The study site had a limited number of patients meeting inclusion criteria, leading to a small sample size. The patients were also similar in demographics, with most of the patients being White and non-Hispanic/non-Latinx.
Conclusion
The COVID-19 vaccine does not appear to contribute to dyscrasia in patients prescribed clozapine. The purpose of this study was to gain additional clinical knowledge about the potential hematologic impact of the COVID-19 vaccination on patients diagnosed with SMI who were taking clozapine. Because clozapine is regarded as the gold-standard antipsychotic intervention for refractory schizophrenia, it is important to avoid any concomitant factors that could contribute to clozapine failure, which would include mandatory cessation with severe neutropenia. Although REMS-required clozapine cessation is no longer permanent, rechallenge may not offer the same robust benefit as an uninterrupted clozapine regimen. Since clozapine is specifically associated with the potential to cause blood dyscrasia and may increase what is already recognized to be a compromised baseline immunity in these patients, additional knowledge regarding the potential hematologic impact is critical. A secondary objective was to examine the rate of vaccine acceptance in patients diagnosed with SMI and hospitalized due to their illness. The majority of patients included in our study accepted vaccination, and therefore, we encourage healthcare providers to encourage vaccination and provide education to reassure patients of the safety and efficacy of COVID-19 vaccination, even if there is initial hesitancy.
References
- Vai B, Mazza MG, Delli Colli C, et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry. 2021;8(9):797–812.
- Danenberg R, Shemesh S, Tzur Bitan D, et al. Attitudes of patients with severe mental illness towards COVID-19 vaccinations: a preliminary report from a public psychiatric hospital. J Psychiatr Res. 2021;143:16–20.
- Veerman SRT, Bogers JPAM, Cohen D, Schulte PFJ. COVID-19: risks, complications, and monitoring in patients on clozapine. Pharmacopsychiatry. 2022;55(1):48–56.
- United States Food and Drug Administration. Fact sheet for patients, parents, and caregivers: emergency use authorization (EUA) of paxlovid for coronavirus disease 2019 (COVID-19). Revised 26 Sep 2022. https://www.fda.gov/media/155051/download. Accessed 19 Jan 2023.
- Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720.
- Gee S, Taylor D. COVID-19 infection causes a reduction in neutrophil counts in patients taking clozapine. J Psychiatry Neurosci. 2021;46(2):E232–E237.
- Zuo Y, Yalavarthi S, Shi H, et al. Neutrophil extracellular traps in COVID-19. JCI Insight. 2020;5(11):e138999.
- Bonaccorso S, Ricciardi A, Ouabbou S, et al. Clozapine, neutropenia and Covid-19: should clinicians be concerned? 3 months report. Brain Behav Immun Health. 2021;13:100212.
- Tomita T, Sakamoto Y, Saito M, et al. Two patients with schizophrenia treated with clozapine developed neutropenia after receiving a COVID-19 vaccine. Int Med Case Rep J. 2022;15:29–33.
- Pereira VC, de Stefani DZ, Braga AGO, et al. Severe granulocytopenia in a patient on long-term use of clozapine and with COVID-19. Psychiatry Res. 2021;305:114171.
- Ponsford M, Castle D, Tahir T, et al. Clozapine is associated with secondary antibody deficiency. Br J Psychiatry. 2018;214(2):1–7.
- Prokopez CR, Vallejos M, Lopredo LS, et al. An analysis of the possible protective effect of antipsychotics for SARS-CoV-2 in patients under treatment for severe mental illnesses. Schizophr Res. 2021;233:99–100.
- de Leon J, Ruan CJ, Verdoux H, Wang C. Clozapine is strongly associated with the risk of pneumonia and inflammation. Gen Psychiatr.
- Shuman M, Lee Demler T, Trigoboff E, Opler LA. Hematologic impact of antibiotic administration on patients taking clozapine. Innov Clin Neurosci. 2012;9(11–12):18–30.
- Takumi K, Garssen J, de Jonge R, et al. Release kinetics and cell trafficking in relation to bacterial growth explain the time course of blood neutrophils and monocytes during primary Salmonella infection. Int Immunol. 2005;17(1):85–93.
- Davis EAK, Hightower T, Cinnamon KA. Toxic clozapine level as first indication of severe, acute infection. Ment Health Clin. 2022;12(1):45–48.
- Tio N, Schulte PFJ, Martens HJM. Clozapine intoxication in COVID-19. Am J Psychiatry. 2021;178(2):123–127.
- Cranshaw T, Harikumar T. COVID-19 infection may cause clozapine intoxication: case report and discussion. Schizophr Bull. 2020;46(4):751.
- Dotson S, Hartvigsen N, Wesner T, et al. Clozapine toxicity in the setting of COVID-19. Psychosomatics. 2020;61(5):577–578.
- Clark SR, Warren NS, Kim G, et al. Elevated clozapine levels associated with infection: a systematic review. Schizophr Res. 2018;192:50–56.
- Bayraktar İ, Yalçın N, Demirkan K. The potential interaction between COVID-19 vaccines and clozapine: a novel approach for clinical trials. Int J Clin Pract. 2021;75(8):e14441.
- Shahani L, Lane SD, Soares JC. COVID-19 vaccine hesitancy in the inpatient psychiatric setting. Psychiatr Serv. 2021;72(11):1360–1361.





