
by David Wyndham Lawrence, MD, MPH
Dr. Lawrence is with the Faculty of Medicine, University of Toronto in Toronto, Canada; Mount Sinai Hospital, Sinai Health System in Toronto, Canada; and Faculty of Kinesiology & Physical Education, University of Toronto in Toronto, Canada.
Funding: No funding was provided for this article.
Disclosures: The author has no conflicts of interest relevant to the content of this article.
Innov Clin Neurosci. 2023;20(7–9):37–39.
Abstract
Background: Migraine is a common neurovascular disorder with a pathophysiology related to the serotonin (5-hydroxytryptamine; 5-HT) system. Pharmacologic modulation of 5-HT receptors has demonstrated efficacy in the acute treatment of migraines. Psilocybin, a classic psychedelic with 5-HT receptor activity, has demonstrated therapeutic potential in the management of neuropsychiatric conditions. To date, no reports have investigated the effect of psilocybin administered acutely during a migraine episode.
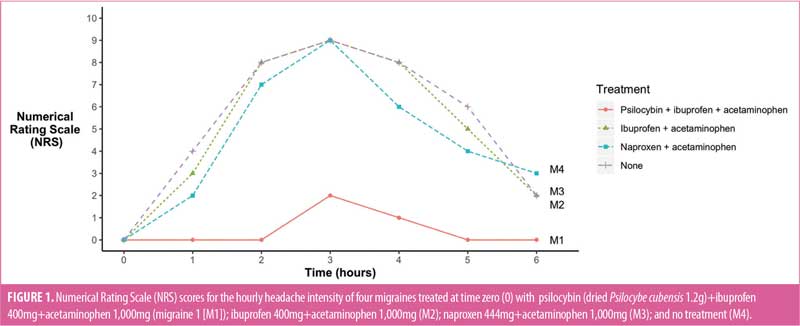
Case presentation: The case of a 33-year-old male patient with a history of migraines with aura, who had acute administration of oral psilocybin (in the form of the dried fruiting body of Psilocybe cubensis mushrooms) at migraine onset is presented. Headache intensity was rated hourly using the Numerical Rating Scale (NRS) and compared to three previous migraines. Profound reductions in headache intensity and emetic episodes were reported during the migraine treated acutely with oral psilocybin administration, compared to three previous migraines.
Discussion: The severe, disabling, and treatment-resistant nature of migraines warrants continued surveillance for novel pharmacologic interventions. The established congruous pathophysiology of migraine and pharmacology of psilocybin, via the 5-HT receptor system, positions psilocybin as a potential therapeutic target.
Conclusion: While this report highlights the potential role of psilocybin in the acute management of migraines, it is essential to note that it should not be considered a basis for guiding clinical practice at this point. Further research is necessary to establish the safety and efficacy of psilocybin as a treatment option for migraines.
Keywords: Psilocybin, psychedelics, migraine, treatment, pharmacology, headache
Migraine is a common neurovascular disorder that affects approximately 10 to 15 percent of the general population.1–3 Migraines are characterized by severe headache and often present with concomitant antecedent aura, nausea, emesis, photophobia, and phonophobia.4–7 The pathogenesis of migraine is a complex process, commencing with a premonitory or prodrome phase, which is followed by an aura phase, headache phase, and postdrome phase.5,8 The premonitory phase involves multiple cortical and subcortical regions, while trigeminovascular activation and cortical spreading depression is associated with the headache phase.8
The comprehensive pathophysiology of migraine remains to be fully elucidated;5 however, the serotonin (5-hydroxytryptamine; 5-HT) system has been implicated as a pivotal factor in the development of this condition.9–11 In humans, there are seven 5-HT receptor families (5-HT1–7), several of which have been associated with migraines and have emerged as promising therapeutic targets.10,12 The 5-HT receptors that are most strongly associated with migraine syndrome are 5-HT1B–1D, 5-HT2B–2C, and 5-HT1F.11 One noteworthy therapeutic example is sumatriptan, a medication of the triptan class, which was among the first to selectively target specific 5-HT receptors, demonstrating high-affinity 5-HT1B and 5-HT1D receptor agonism.10,12 Ergot derivatives, which also have known 5-HT1B and 5-HT1D receptor agonism, have been used for decades for the abortive treatment of migraines, but are currently not first-line agents due to concerns over the side effect and safety profile.5,11,13 Recent advances have also uncovered pathways involving the calcitonin gene-related peptide (CGRP) within the pathophysiology of migraine, leading to the introduction of a new class of therapeutics, monoclonal antibiotics that function as antagonists of the CGRP molecule or its receptor.14
Recently, there has been a renewed interest in the therapeutic potential of psilocybin in the treatment of neuropsychiatric conditions,15–17 with early reports examining its role in the management of migraines.18,19 In a small (n=10) double-blind, placebo-controlled, crossover study, a single dose of prophylactic psilocybin significantly reduced weekly migraine days, independent of the intensity of the acute psychotropic effects, with no adverse events (AEs).19 However, a double-blind study investigated the role of five doses of psilocybin on headache in 18 healthy volunteers and observed a dose-dependent increase in transient delayed headache.20 These findings highlight the necessity for further research to delineate a role, if any, for psilocybin in the management of headaches. Furthermore, no study to date has examined the therapeutic potential of psilocybin administered acutely during a migraine episode.
Psilocybin is primarily recognized as a potent 5-HT2A receptor agonist, which accounts for its psychedelic properties.21,22 Although the 5-HT2A receptor has previously garnered interest in relation to migraine pathophysiology and treatment,23,24 it has since been excluded as a contributing receptor.11 Correspondingly, recent research has revealed that psilocybin, and, more accurately, the active metabolite psilocin, interacts with a multitude of 5-HT receptors, including the 5-HT2B, 5-HT1D, 5-HT1E, 5-HT1A, 5-HT5A, 5-HT7, 5-HT6, 5-HT2C, and 5-HT1B receptors.25–27 Despite this, current trends emphasize the importance of understanding the global effects of psychedelics from a whole-brain perspective, rather than focusing solely on individual brain regions or receptor interactions,28,29 as this could potentially reveal alternative therapeutic avenues.
This case report explores the potential of psilocybin administration as an abortive treatment for migraine. As a complex and prevalent neurological condition,5 ongoing surveillance for novel and effective therapeutic approaches for migraines is warranted. The growing interest in the therapeutic potential of psilocybin, along with its interaction with various serotonin receptors, presents a unique opportunity to investigate its efficacy in migraine management. By examining the effects of psilocybin administration during an acute migraine episode, this case report aims to contribute to the understanding of its potential therapeutic role, safety, and tolerability. The findings from this case report could inform future research and potentially pave the way for new treatment strategies in the field of migraine management.
Case Presentation
We present the case of a 33-year-old male patient with a history of intermittent migraine with aura since childhood. The reported migraine pattern was stable, with a migraine frequency of once every 3 to 6 months. The migraine peak severity was 6 to 10 out of 10 on the Numerical Rating Scale (NRS), lasting an average of five hours (range: 4–6), with associated nausea, emesis, photophobia, and phonophobia. Previous acute pharmacological treatments included sumatriptan, naproxen, acetaminophen, and metoclopramide, with minimal effectiveness. He had no other neuropsychiatric conditions and was not taking any other medications. He had 10 to 12 previous experiences with a moderate dose of psilocybin.
The patient reported orally administering 1.2g of the dried fruiting body of Psilocebe cubensis mushroom, ibuprofen 400mg, and acetaminophen 1,000mg at the onset of an aura. The aura was characterized by scintillating scotoma, left temporal inferior quadrantanopia, and paraesthesias of the left first and second fingers, as well as the lip. The patient recorded the headache intensity hourly using the NRS and the number of episodes of emesis.
Data was available from three previous migraines with aura, occurring approximately three, six, and 12 months prior to the index migraines. These prior migraines were treated acutely with ibuprofen 400mg and acetaminophen 1,000mg, naproxen 444mg and acetaminophen 1,000mg, and no treatment, respectively. Compared to the previous three migraines, the NRS scores following acute psilocybin treatment were profoundly lower. The peak NRS scores following psilocybin treatment were between 0 and 2, compared to 6 to 9 during the peak severity of the previous comparison migraines (Figure 1). Moreover, only one episode of emesis was reported following psilocybin treatment, compared to approximately four episodes during each of the three previous migraines. The patient denied any adverse effects following psilocybin use.
Discussion
In this case report, a healthy 33-year-old male patient with a history of migraine with aura self-administered oral psilocybin at the onset of a migraine episode, resulting in a noticeable reduction in headache intensity, compared to three previous migraines. As far as the author is aware, no prior reports have described the response to psilocybin when taken acutely at the onset of a migraine.
The first study investigating the migraine-suppressing effects of psilocybin was a double-blind, placebo-controlled, crossover study involving 10 adults with migraine.19 A single administration of oral synthetic psilocybin (0.143mg/kg) led to a significantly greater reduction in weekly migraine days from baseline during the subsequent two-week period, compared to placebo. Furthermore, psilocybin treatment resulted in significantly greater reductions from baseline in weekly migraine attacks, pain severity, attack-related functional impairment, and weekly migraine abortive days, compared to placebo. This exploratory study demonstrated that psilocybin was well-tolerated and may provide safe, enduring migraine prophylaxis for up to two weeks following a single administration. Interestingly, the observed therapeutic effects of psilocybin appeared to be independent from the acute psychotropic effects, suggesting that the therapeutic properties might not rely on the typical perceptual changes associated with psychedelics.19
5-HT receptors are intimately involved in both the pathophysiology of migraine5,9,11 and the pharmacology of psilocybin.25–27 However, it is premature and out of the scope of this study to propose a potential pharmacological pathway of psilocybin as it relates to migraine episodes. Moreover, understanding the effects of psychedelics might be better approached from a dynamic, whole-brain perspective, rather than solely focusing on region-, network-, or receptor-specific changes.28 This case report should act as a catalyst for discussion and further research into the potential role of psilocybin in migraine management and should not be considered as a basis for informing clinical practice at this stage.
Limitations. The limitations of this study are considerable. First, it is a single observational case report comparing different treatments under potentially varying migraine conditions, with no control or repeated measures. Second, the psychoactive effects, such as mood and dissociative effects, of the psilocybin treatment were not documented and, thus, not included in this report. Consequently, if the therapeutic effect of psilocybin is indeed valid, determining the precise mechanism remains elusive, as it could be related to nociceptive properties or psychoactive psychedelic properties, such as enhancing mood, alleviating psychological distress, or creating a distraction effect, among others.
Conclusion
This case study describes a 33-year-old male patient with a history of periodic migraine with aura who observed a substantial decrease in headache intensity after the acute use of psilocybin, in contrast to three previous migraines managed with different medications or no treatment. Although the precise mechanism of action is still uncertain, this case emphasizes the potential application of psilocybin in migraine treatment and calls for more in-depth research. Nevertheless, it is crucial to acknowledge the limitations of this individual case report, such as the lack of a control or repeated measures and the absence of documentation regarding psychoactive effects during the treatment. Consequently, this report should act as a stimulus for further discussion and exploration of the potential role of psilocybin in migraine management, but it should not be viewed as a foundation for guiding clinical practice at this point.
References
- Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210.
- Stewart WF, Wood C, Reed ML, et al. Cumulative lifetime migraine incidence in women and men. Cephalalgia. 2008;28(11):1170–1178.
- Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–349.
- Goadsby PJ, Evers S. International Classification of Headache Disorders – ICHD-4 alpha. Cephalalgia. 2020;40(9):887–888.
- Ferrari MD, Goadsby PJ, Burstein R, et al. Migraine. Nat Rev Dis Primers. 2022;8(1):2.
- Jensen R, Stovner LJ. Epidemiology and comorbidity of headache. Lancet Neurol. 2008;7(4):354–361.
- Launer LJ, Terwindt GM, Ferrari MD. The prevalence and characteristics of migraine in a population-based cohort: the GEM study. Neurology. 1999;53(3):537–542.
- Dodick DW. A Phase-by-phase review of migraine pathophysiology. Headache. 2018;58 Suppl 1:4–16.
- Panconesi A. Serotonin and migraine: a reconsideration of the central theory. J Headache Pain. 2008;9(5):267–276.
- Villalon CM, VanDenBrink AM. The role of 5-hydroxytryptamine in the pathophysiology of migraine and its relevance to the design of novel treatments. Mini Rev Med Chem. 2017;17(11):928–938.
- Leone M, Rigamonti A, D’Amico D, et al. The serotonergic system in migraine. J Headache Pain. 2001;2(Supp1):S43–S46.
- de Vries T, Villalón CM, MaassenVanDenBrink A. Pharmacological treatment of migraine: CGRP and 5-HT beyond the triptans. Pharmacol Ther. 2020;211:107528.
- Tfelt-Hansen P, Saxena PR, Dahlof C, et al. Ergotamine in the acute treatment of migraine: a review and European consensus. Brain. 2000;123(Pt 1):9–18.
- Mohanty D, Lippmann S. CGRP inhibitors for migraine. Innov Clin Neurosci. 2020;17(4–6):39–40.
- Lawrence DW, Sharma B, Griffiths RR, Carhart-Harris R. Trends in the top-cited articles on classic psychedelics. J Psychoactive Drugs. 2021:53(4):283–298.
- Carhart-Harris R, Giribaldi B, Watts R, et al. Trial of psilocybin versus escitalopram for depression. N Engl J Med. 2021;384(15):1402–1411.
- Griffiths RR, Johnson MW, Carducci MA, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181–1197.
- Andersson M, Persson M, Kjellgren A. Psychoactive substances as a last resort–a qualitative study of self-treatment of migraine and cluster headaches. Harm Reduct J. 2017;14(1):60.
- Schindler EAD, Sewell RA, Gottschalk CH, et al. Exploratory controlled study of the migraine-suppressing effects of psilocybin. Neurotherapeutics. 2021;18(1):534–543.
- Johnson MW, Sewell RA, Griffiths RR. Psilocybin dose-dependently causes delayed, transient headaches in healthy volunteers. Drug Alcohol Depend. 2012;123(1–3):132–140.
- Kwan AC, Olson DE, Preller KH, Roth BL. The neural basis of psychedelic action. Nat Neurosci. 2022;25(11):1407–1419.
- Nichols DE. Psychedelics. Pharmacol Rev. 2016;68(2):264–355.
- Mylecharane EJ. 5-HT2 receptor antagonists and migraine therapy. J Neurol. 1991;238 Suppl 1:S45–S52.
- Srikiatkhachorn A, Suwattanasophon C, Ruangpattanatawee U, et al. 5 -HT2A receptor activation and nitric oxide synthesis: a possible mechanism determining migraine attacks. Headache. 2002;42(7):566–574.
- Coppola M, Bevione F, Mondola R. Psilocybin for treating psychiatric disorders: a psychonaut legend or a promising therapeutic perspective? J Xenobiot. 2022;12(1):41–52.
- Dodd S, Norman TR, Eyre HA, et al. Psilocybin in neuropsychiatry: a review of its pharmacology, safety, and efficacy. CNS Spectr. 2022:1–11.
- Ray TS. Psychedelics and the human receptorome. PLoS ONE. 2010;5(2):e9019.
- Girn M, Rosas FE, Daws RE, et al. A complex systems perspective on psychedelic brain action. Trends Cogn Sci. 2023;27(5):433–445.
- Carhart-Harris RL, Friston KJ. REBUS and the anarchic brain: toward a unified model of the brain action of psychedelics. Pharmacol Rev. 2019;71(3):316–344.


