 by Simona Portaro, MD, PhD; Laura Ciatto, PT; Loredana Raciti, MD, PhD; Enrico Aliberti, MSc; Riccardo Aliberti, Msc; Antonino Naro MD, PhD; and Rocco Salvatore Calabrò, MD, PhD
by Simona Portaro, MD, PhD; Laura Ciatto, PT; Loredana Raciti, MD, PhD; Enrico Aliberti, MSc; Riccardo Aliberti, Msc; Antonino Naro MD, PhD; and Rocco Salvatore Calabrò, MD, PhD
All authors are with IRCCS Centro Neurolesi “Bonino-Pulejo” in Messina, Italy.
FUNDING: No funding was provided for this study.
DISCLOSURES: The author has no conflicts of interest relevant to the content of this article.
ABSTRACT: Primary lateral sclerosis (PLS) is an adult-onset idiopathic disorder of the upper motor neuron system. Robot-aided rehabilitation with the Lokomat-Pro (LT) allows maximizing motor training by finely and individually controlling motor activation. No data are currently available on the use of robot-aided rehabilitation in PLS. The aim of this case study was to evaluate the effectiveness of a customized robotic rehabilitation protocol in PLS. A 54-year-old woman, diagnosed with PLS five years before admission, came to our clinic to undergo rehabilitation training due to gait difficulties with spastic paraparesis. The patient was treated with two different approaches: conventional physiotherapy followed by a combined approach (i.e. PT plus LT). After the conventional PT rehabilitation, no significant functional improvement was noted. However, the combined approach led to a significant improvement in functional motor skills, including walking, balance and lower limb muscle strength, and spasticity. Our experimental training combining robot-aided and conventional rehabilitation could be a promising approach to mitigate the PLS disability burden.
Keywords: Motor neuron disease, primary lateral sclerosis, robotic rehabilitation, lokomat
Innov Clin Neurosci. 2021;18(4–6):XXXX
Motor neuron diseases (MND) are a group of heterogeneous disorders inducing degeneration of upper and/or lower motor neurons.1 Primary lateral sclerosis (PLS) accounts for only 3 to 5 percent of adult-onset MND, and it involves the upper motor neurons only.2 PLS clinically presents with slowly progressive symmetric spinobulbar spasticity and pathologically increased deep tendon reflexes.3 However, its early diagnosis can be challenging due to its nondisease specific core clinical symptoms and the need for a differential diagnosis.2,3 The Gordon criteria require a symptomatic period of four years before making a PLS diagnosis, since MND, including amyotrophic lateral sclerosis (ALS), may initially manifest with upper motor neuron signs.4
Despite the ongoing research to develop pharmacological treatment options for MND, insufficient attention is paid to the rehabilitation therapy.5 The main goal of physiotherapy is actually to limit the decline in muscle strength and decrease pain and spasticity, which worsen the disease burden and quality of life.6,7 In particular, a strictly monitored exercise program has been proposed to potentially reduce motor deterioration and decrease the deconditioning and muscle atrophy that can result from progressive inactivity in patients with ALS.7 Experimental data have demonstrated moderate effects and benefits of submaximal resistive exercises, which are considered safe, especially in the early stages of the MND.8 On the other hand, excessive or high resistance exercises are contraindicated and are associated with muscle overwork damage.8 Thus, it is recommended to avoid exceeding the aerobic threshold for motor exercise.
Robot-aided rehabilitation is promising because it maximizes motor training by finely and individually controlling motor activation, thus improving functional ambulation in patients with different neurological disorders.9-13 Moreover, robot-aided rehabilitation is based on the principle of motor relearning that results from intensive, repetitive, and task-oriented motor activities requiring a patient’s active participation.13 Such a training is thought to restore neural plasticity and brain functional connectivity following brain damage and be potentially useful in some neurodegenerative diseases involving the central and peripheral nervous systems.14-16
Despite these promising treatments, there is very little evidence on the usefulness of robotics in the MND rehabilitation field.17-20 Further, no published data have demonstrated the feasibility and the usefulness of robot-aided rehabilitation in PLS patients. We hypothesized that such an approach could be effective in the treatment of neurodegenerative diseases involving the upper motor neurons, such as PLS. Herein, we report the case of a 54-year-old woman with PLS who was treated with the combined approach of conventional rehabilitation plus robot-aided gait training (RAGT) by means of the Lokomat®Pro V6 Free-D module (Hocoma AG; Volketswil, Switzerland), and showed a significant improvement in functional ambulation. The informed written consent was obtained from the patient for the experimental treatment and data publication.
Case Description
A 54-year-old Caucasian woman, diagnosed five years prior to presentation, came to our institute to undergo a rehabilitation training due to progressive worsening in gait and balance. Family history was negative for neuromuscular disorders. Since the age of 34, the patient reported on episodic difficulty swallowing liquids. Since the age of 49, the patient reported lower limb muscle weakness with falls. After two years, the patient began manifesting upper limb muscle weakness with difficulty in grasping. Based on the symptoms, a brain and cervical MRI was ordered, which showed a symmetrical hyperintensity signal of the corticospinal tracts. As her clinical condition progressively worsened, she was admitted to the neurology unit of another hospital where she was diagnosed with “probable PLS.” After the patient was admitted to our outpatient program, neurological assessment showed gait difficulties with spastic paraparesis, especially involving the left side, requiring the use of a rollator when she walked. A very mild muscle hypotrophy was detected distally at the four limbs with asymmetric involvement (left>right). Retractions of the achilles tendons and brisk deep tendon reflexes prevailing on the left side and clone of the feet were also revealed. There were no abnormalities in sensibility, cerebellar, and sphinteric functions.
Rehabilitation Protocol
Rationale. As there are no specific guidelines to treat this rare disease, we asked the patient to undergo a research protocol to compare the effects of physiotherapy (PT) alone with PT plus RAGT. We hypothesized that the use of RAGT may be more effective, compared to PT alone, in improving functional ambulation and disease burden due to a repetitive, task-oriented exercise that entrains neuroplasticity mechanisms involved in neural damage recovery.21 Thus, this same mechanism might be useful to counteract the neurodegenerative process.22 Moreover, the higher intensity of the exercise, compared to PT alone, is completely assisted, which can be modulated per the patient’s needs, which helpes prevent exceeding the patient’s aerobic threshold, which is critical when treating MND.23 In particular, aerobic exercise training activates the Type I slow-twitch oxidative muscle fibers, which typically contract slower and at a lower intensity.24 Such muscle fibers allow the endurance work to be done for long periods of time, increasing the size and number of these Type I muscle fibers and improving the endurance performances before fatigue sets in. The transition of myofibers from Type II to Type I may allow for enhanced muscle adaptability.25
Anaerobic exercise, on the other hand, improves the power and strength of muscles by increasing hypertrophy or size, due to the particular characteristics of the anaerobic activity. This is shortlived due to the lack of oxygen that triggers the lactic acid production. The buildup of lactate is what causes fatigue. Moreover, the anaerobic exercise increases glycolysis, boosting the ATP levels and hormone production, which causes muscle hypertrophy.26
In addition to modifying the muscle fiber types and mass, exercise also causes an initial increase in free radical production and oxidative stress, which is counteracted by the subsequent activation of the endogenous antioxidative defense mechanism.26-27 A new homeostasis is achieved; thus, regular exercise of moderate intensity appears to result in a lower basal state of oxidative stress level.26,27 Depending on the duration and intensity of the exercise and the age of the person, myokines, such as IL-6, are released during physical intensive exercise and benefit health by inducing adipose tissue reduction and muscle growth and myogenesis, as well as regulate energy metabolism. On the other hand, physical inactivity, due to age or a sedentary behaviour, seems to impair myokine response, partially explaining the increase in chronic diseases in these conditions.
Rehabilitation Protocol
Procedures. The first period of treatment was carried out by using conventional low-intensity PT in the outpatient program, three times a week for eight weeks, with each session lasting up to 60 minutes. There were periods of rest as per the patient’s need, and the patient did not exceed aerobic threshold. This was ensured by monitoring oxygen saturation with a pulse oximeter and avoiding fatigue. The PT focused on improving walking resistance, muscle strength, and balance. This consisted of passive mobilization, with stretching exercises, active-assisted exercises, respiratory treatment aiming at maintaining lung function, tissue oxygenation and resistance, and balance and gait training.
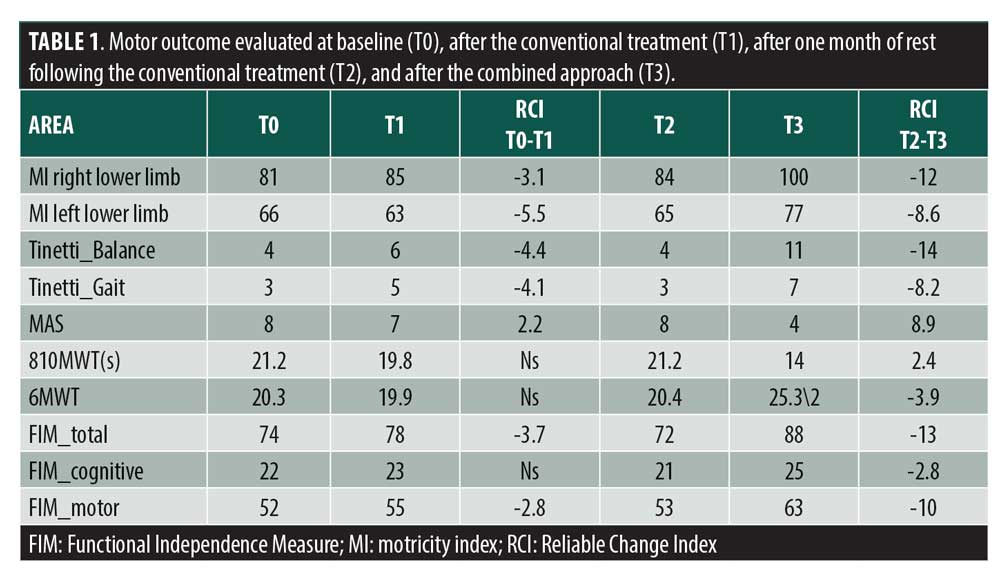
After conventional treatment, the patient had not gained any significant functional recovery post PT, based on the considered outcome measures (Table 1). One month later, she underwent treatment with specific RAGT, combined with PT for two months. Specifically, the patient was provided with three weekly RAGT sessions (24 rehabilitation sessions) and PT to potentiate the residual functional abilities. In each RAGT session, which lasted about 45 minutes, the patient was required to walk straight forward with the provision of the visual feedback of the RAGT virtual reality games.
The RAGT module used to treat the patient is a robotic device consisting of a motorized gait orthosis with computer-controlled linear actuators integrated into each hip and knee joint, a body-weight support system (BWS), and a treadmill. Gait and driving force were adjusted according to the patient’s needs to optimize functional training on sagittal, frontal, and transverse planes. The applied free-D module allowed pelvic rotation and weight shifting with a physiological gait. The system also assessed the rigidity of the patient’s hips and knee joints and the isometric force exerted, respectively, by the hip and knee extension from the L-STIFF and LFORCE software module. The feedback module enhanced by the virtual reality screen provided instructive, stimulating, interactive, and direct stimuli to the patient while walking, projecting the results of the exercises on a display to improve patient motivation and fostering motor and cognitive recovery. The exercises were mainly based on activities in which the patient had to collect and/or avoid objects randomly distributed in the virtual environment. The exercises were adapted to the motor and cognitive abilities and to the specific needs of the patient, obtaining personalized feedback. The BWS was initially set at 80 percent, and gradually reduced to 20 percent. Treadmill speed was initially set at 0.19 meters/second, to ensure greater perception of load on lower limbs and greater awareness and continuous correction of the gait cycle, according to the RAGT device manual. The speed was gradually increased to reach the one perceived as comfortable by the patient (max. 0.5 m/s). The conduction force of the device was varied symmetrically for the right and left lower limbs, starting from 100 percent to 40 percent. Therefore, the RAGT parameters were kept constant through the sessions. The vital signs were monitored continuously during the sessions and, after each RAGT, the patient was allowed to rest for 10 minutes. At the beginning of each session, the patient underwent a 5- to 10-minute period of adaptation to the device according to the user manual. This included the correct positioning of the straps and cuffs, the alignment in an acceptable range of movement, consideration of the RAGT parameters, time required to reach the maximum tolerated BWS daily, the duration of the walk, the walking speed, and the driving force of the device supplied to each leg.
The PT was always carried out before the RAGT sessions but after at least one hour of rest, and was performed with the same modalities. At the end of the training, the patient was asked to rate the experience with the device using a 10-point Likert scale.
Outcome Measures
The outcome measures were as follows:
Motricity Index to measure strength in upper and lower extremities28
Six Minutes Walking Test (6MWT) to measure the integrated global response of multiple cardiopulmonary and musculoskeletal systems involved in exercise, providing information on functional capacity, response to therapy and prognosis across a broad range of chronic conditions29
Tinetti Scale to measure gait and balance30
Modified Ashwort Scale (MAS) to measure resistance during passive soft-tissue stretching, thus measuring spasticity31
Ten Meters Walking Test (10MWT) to assess walking speed in meters per second, functional mobility, gait, and vestibular function over a short distance32
Functional Independence Measure (FIM) to explore individual’s physical, psychological and social functions in response to rehabilitation or medical intervention33
These outcome measures were administered at baseline (T0), after PT (T1), after one month of rest following the PT (T2), and after the combined approach (T3). The primary goal was to obtain a significant improvement in gait speed, endurance, and balance (as per the Reliable Change Index, RCI) at the end of PT and RAGT rehabilitation protocol. The boundary value for statistical significance within the RCI was ≥1.96 (1.96 equates to the 95% confidence interval [CI]).
Results
The patient completed the training without side effects and found the device useful and motivating (8/10 Likert Scale). At baseline (T0), the motor evaluation showed a reduced gait velocity and endurance and an impaired balance; the patient required a consistent time to complete the 10MWT. The FIM scale showed a moderate assistance level. At the end of PT (T1), we found a mild, nonsignificant improvement in all the outcome measures, except for the 6MWT and the cognitive item of the FIM scale. At the end of the 1-month period of rest (T2), she got the same scorings at T0. After two months of the combined approach (PT plus RAGT sessions) (T3), the patient showed significant improvement in all outcome measures.
Discussion
To the best of our knowledge, this is the first case of RAGT in a patient with PLS. Our combined approach induced a more evident improvement in walking, balance, and lower-limb muscle strength and spasticity compared to PT alone, thus reducing the overall disability burden. To date, many studies have shown robotic devices to be useful in treating several neurological diseases.14-17,34,35 However, few studies have focused on rare neuromuscular disorders.7,21-24 PLS exclusively involves the upper motor neurons. Physiotherapy, including muscle stretching, balance and gait training, and occupational therapy, may reduce muscle atrophy, improve endurance, and counterbalance the negative effects induced by the neurodegeneration process by potentiating the cardiovascular, respiratory, endocrine, musculoskeletal, and immune systems. A recent study carried out on patients with ALS showed that a strictly monitored exercise program might significantly slow motor wasting and weakness processes.7 The incomplete activation of muscle fibers due to the progressive impairment of motor neuron recruitment with a concomitant impaired oxidative function explains patient fatigue, which is correlated to muscle wasting.36 RAGT may be considered a valuable tool to improve muscle force and slow neuromuscular deterioration due to the ability to administer aerobic exercises in a controlled manner. The efficacy of neurorobotics in improving motor function depends on the high frequency and intensity of repetition of task-oriented movements, resulting in motor learning.9 In particular, with the addition of robotic exoskeletons, therapists are able to treat patients with lower extremity weakness or paralysis more safely and efficiently, allowing them to perform high-frequency robotic-assisted stepping that resembles normal gait pattern more effectively than PT gait training. Given that RAGT has been demonstrated to be less energy demanding due to the BWS, this approach may postpone the onset of fatigue and allow longer training sessions of repeated task-oriented practice.37 In addition, RAGT has been reported to be less cardiorespiratory stressful for aerobic training. These results may also provide support for the safe use of RAGT in neurological patients with cardiorespiratory problems.37
As shown in a previous study, exoskeletons could be useful to recover mobility in people with neurological impairment due to central nervous system (CNS) diseases (i.e. stroke, owing to mechanisms of brain plasticity and connectivity remodulation that are specifically targeted by the robotic device).14 Thus, rehabilitation techniques targeting motor systems could be beneficial in improving gait capacity in patients with neurological disorders, including MND. Moreover, neuroplasticity mechanisms have been linked to improvements in motor functioning in patients with myotonic dystrophy Type 1, further suggesting that robotics may also boost neuralplasticity in neuromuscular disorders.16 Our patient was provided a combined conventional and robotic rehabilitative approach to further enhance the neuroplasticity mechanisms, by harnessing motor learning processes, through concomitant use of virtual reality. Providing patients with an online feedback (visuomotor in particular) is believed to be essential in triggering sensorimotor areas in the mirror neuron system. This has a striking importance concerning both motor imitation and (re)learning.14 The simple exposure to a video containing motoric sequences potentially reactivates the residual damaged cortical motor neurons.39 By repetition, mirror neuron system activation is thought to improve movement recovery by reinforcing the motor circuits responsible for the execution of the observed actions.15,38 Mirror therapy may influence the neural circuitry that reprograms the motor act by the visual guidance of consistent, simple illusory movement of the avatar in the virtual reality environment or, more likely, by the visual guidance of the mismatch between the movement one performs and the movement that is observed.38,39 Moreover, we hypothesize that the RAGT counterbalanced the deregulation of the central pattern generator that follows the deterioration of the corticospinal tract with the prevalence of the “nonpyramidal” descending pathways. This may be relevant to the increase or decrease of the amplitude of the monosynaptic stretch reflex in response to an imposed muscle lengthening, indicating some degree of learning in the spinal cord (i.e. spinal intelligence).39 We can only speculate on such an issue because we did not perform a gait analysis. Furthermore, the beneficial effects raised by the RAGT might be mediated by inhibiting oxidative stress due to the corticospinal degeneration, as the RAGT favors the oxidative metabolism.40
Even though our data are promising concerning functional ambulation outcome in PLS, the natural course of MND raises caution to generalize our findings and suggest the use of RAGT in patients with PLS. Patients with neuromuscular diseases should be trained more intensively with RAGT at the beginning of the disease when their physical condition is better. A gradual reduction of RAGT intensity up to the use of different robotic and substitution devices should be applied as patient condition progressively deteriorates. This is in the opposite direction of the training we usually apply in acquired brain injury, where intensity and functional challenge increase as the patient improves.16 Future studies on larger patient cohorts are needed to confirm our results and evaluate the long-term effects of this promising combined approach to realize the best patient-tailored rehabilitation protocol.
References
- Foster LA, Salajegheh MK. Motor neuron disease: pathophysiology, diagnosis, and management. Am J Med. 2019;132(1):32–37.
- Pringle CE, Hudson AJ, Munoz DG, et al. Primary lateral sclerosis. Clinical features, neuropathology and diagnostic criteria. Brain. 1992;115(Pt 2):495–520.
- Singer MA, Kojan S, Barohn RJ, et al. Primary lateral sclerosis: clinical and laboratory features in 25 patients. J Clin Neuromuscul Dis. 2005;7(1):1–9.
- Gordon PH, Cheng B, Katz IB, et al. The natural history of primary lateral sclerosis. Neurology. 2006;66(5):647–653.
- Dorst J, Ludolph AC, Huebers A. Disease-modifying and symptomatic treatment of amyotrophic lateral sclerosis. Ther Adv Neurol Disord. 2017;9;11:1756285617734734.
- Chiò A, Benzi G, Dossena M, et al. Severely increased risk of amyotrophic lateral sclerosis among Italian professional football players. Brain. 2005;128(Pt 3):472–476.
- Lunetta C, Lizio A, Sansone VA, et al. Strictly monitored exercise programs reduce motor deterioration in ALS: preliminary results of a randomized controlled trial. J Neurol. 2016;263(1):52–60.
- Svensson M, Lexell J, Deierborg T. Effects of physical exercise on neuroinflammation, neuroplasticity, neurodegeneration, and behavior: what we can learn from animal models in clinical settings. Neurorehabil Neural Repair. 2015;29(6):577–589.
- Bruni MF, Melegari C, De Cola MC, et al. What does best evidence tell us about robotic gait rehabilitation in stroke patients: a systematic review and meta-analysis. J Clin Neurosci. 2018;48:11–17.
- van Hedel HJA, Severini G, Scarton A, et al. Advanced robotic therapy integrated centers (ARTIC): an international collaboration facilitating the application of rehabilitation technologies. J Neuroeng Rehabil. 2018;15(1):30.
- Furnari A, Calabrò RS, De Cola MC, et al. Robotic-assisted gait training in Parkinson’s disease: a three-month follow-up randomized clinical trial. Int J Neurosci. 2017;127(11):996–1004.
- Calabrò RS, Cacciola A, Bertè F, et l. Robotic gait rehabilitation and substitution devices in neurological disorders: where are we now? Neurol Sci. 2016;37(4):503–514.
- Calabrò RS, De Luca R, Leo A, et al. Lokomat training in vascular dementia: motor improvement and beyond! Aging Clin Exp Res. 2015;27(6):935–957.
- Calabrò RS, Naro A, Russo M, et al. Shaping neuroplasticity by using powered exoskeletons in patients with stroke: a randomized clinical trial. J Neuroeng Rehabil. 2018;15(1):35.
- Calabrò RS, Naro A, Russo M,et al. The role of virtual reality in improving motor performance as revealed by EEG: a randomized clinical trial. J Neuroeng Rehabil. 2017;14(1):53.
- Portaro S, Naro A, Chillura A, et al. Toward a more personalized motor function rehabilitation in myotonic dystrophy type 1: the role of neuroplasticity. PLoS One. 2017;12(5):e0178470.
- Sanjak M, Bravver E, Bockenek WL, et al. Supported treadmill ambulation for amyotrophic lateral sclerosis: a pilot study. Arch Phys Med Rehabil. 2010;91(12):1920–1929.
- Zhang H, Chang BC, Andrews J, et al. A robotic neck brace to characterize head-neck motion and muscle electromyography in subjects with amyotrophic lateral sclerosis. Ann Clin Transl Neurol. 2019;6(9):1671–1680.
- Portaro S, Cimino V, Accorinti M, et al. A promising tool for flail arm in amyotrophic lateral sclerosis rehabilitation: a case report. Eur J Phys Rehabil Med. 2019;55(4):515–518.
- Calabrò RS, Portaro S, Manuli A, et al. Rethinking the robotic rehabilitation pathway for people with amyotrophic lateral sclerosis: a need for clinical trials. Innov Clin Neurosci. 2019;16(1-2):11–12.
- Esquenazi A, Talaty M. Robotics for lower limb rehabilitation. Phys Med Rehabil Clin N Am. 2019;30(2):385–397.
- Hirsch MA, van Wegen EEH, Newman MA, Heyn PC. Exercise-induced increase in brain-derived neurotrophic factor in human Parkinson’s disease: a systematic review and meta-analysis. Transl Neurodegener. 2018;7:7.
- Kim YH. Robotic assisted rehabilitation therapy for enhancing gait and motor function after stroke. Prec and Future Med. 2019; 3(3): 103-115.
- Metaxas TI, Mandroukas A, Vamvakoudis E, et al. Muscle fiber characteristics, satellite cells and soccer performance in young athletes. J Sports Sci Med. 2014;13(3):493–501.
- Castro MJ, Apple DF Jr, Hillegass EA, Dudley GA. Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol. 1999;80(4):373–378.
- Mackey AL, Karlsen A, Couppé C, et al. Differential satellite cell density of type I and II fibres with lifelong endurance running in old men. Acta Physiol (Oxf). 2014;210(3):612–627.
- Cobley JN, Moult PR, Burniston JG, et al. Exercise improves mitochondrial and redox-regulated stress responses in the elderly: better late than never! Biogerontology. 2015;16(2):249–264.
- Cameron D, Bohannon RW. Criterion validity of lower extremity Motricity Index scores. Clin Rehabil. 2000;14(2):208–211.
- Enright PL. The six-minute walk test. Respir Care. 2003;48(8):783–785.
- Balance LC. Gait Test Proves Simple Yet Useful. P.T. Bulletin, 1993; 2/10:9 & 40 Tinetti ME. Performance-oriented Assessment of Mobility Problems in Elderly Patients. JAGS 1986; 34:119–126.
- Ansari NN, Naghdi S, Arab TK, Jalaie S. The interrater and intrarater reliability of the Modified Ashworth Scale in the assessment of muscle spasticity: limb and muscle group effect. NeuroRehabilitation. 2008;23(3):231–237.
- Watson MJ. Refining the ten-metre walking test for use with neurologically impaired people. Physiotherapy. 2002;88(7): 386–397
- Linacre JM, Heinemann AW, Wright BD, et al. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil. 1994;75(2):127–132.
- Morone G, Paolucci S, Cherubini A, et al. Robot-assisted gait training for stroke patients: current state of the art and perspectives of robotics. Neuropsychiatr Dis Treat. 2017;13:1303–1311.
- Mehrholz J, Thomas S, Werner C, et al. Electromechanical-assisted training for walking after stroke. Cochrane Database Syst Rev. 2017;5(5):CD006185.
- Lanfranconi F, Ferri A, Corna G, et al. Inefficient skeletal muscle oxidative function flanks impaired motor neuron recruitment in Amyotrophic Lateral Sclerosis during exercise. Sci Rep. 2017;7(1):2951.
- Lefeber N, Swinnen E, Kerckhofs E. The immediate effects of robot-assistance on energy consumption and cardiorespiratory load during walking compared to walking without robot-assistance: a systematic review. Disabil Rehabil Assist Technol. 2017;12(7):657–671.
- Garrison KA, Winstein CJ, Aziz-Zadeh L. The mirror neuron system: a neural substrate for methods in stroke rehabilitation. Neurorehabil Neural Repair. 2010;24(5):404–412.
- Ramírez-Jarquín UN, Tapia R. Excitatory and inhibitory neuronal circuits in the spinal cord and their role in the control of motor neuron function and degeneration. ACS Chem Neurosci. 2018;9(2):211–216.
- Chen GQ, Mou CY, Yang YQ, et al. Exercise training has beneficial anti-atrophy effects by inhibiting oxidative stress-induced MuRF1 upregulation in rats with diabetes. Life Sci. 2011;89(1-2):44–49.





