by Carolyn O’Donnell, PharmD; Tammie Lee Demler, PharmD, MBA, BCGP, BCPP; and Eileen Trigoboff, RN, PMHCNS-BC, DNS, DABFN;
Drs. O’Donnell, Demler, and Trigoboff are with the State University of New York at Buffalo School of Pharmacy and Pharmaceutical Sciences, Department of Pharmacy Practice in Buffalo, New York. Drs. O’Donnell and Demler are with the New York State Office of Mental Health at Buffalo Psychiatric Center in Buffalo, New York. Drs. Demler and Trigoboff are with the State University of New York at Buffalo School of Medicine, Department of Psychiatry in Buffalo, New York.
Funding: No funding was provided for this study.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Innov Clin Neurosci. 2022;19(1–3):33–38.
ABSTRACT: Objective: The utility of selective serotonin reuptake inhibitors (SSRIs) has been overshadowed by the box warning they received when the United States (US) Food and Drug Administration (FDA) identified an increased risk of suicidality in patients 24 years of age or younger. Newer studies have identified suicidality as self-aggression and hypothesized whether this might also apply to aggression toward others. The controversy surrounding SSRIs has led to a decrease in prescriptions from healthcare clinicians and number of patients seeking the necessary treatment. The objective of this study was to determine if there is a relationship between SSRI use and aggressive behavior in an inpatient state psychiatric facility.
Design: Using a retrospective analysis, patients (N=64) admitted to an inpatient state psychiatric facility between January 1, 2013, and December 31, 2020, who were taking SSRIs were assessed to determine if they had an increased risk of aggression, whether toward themselves or others. Patients served as their own comparators and were required to have a period without an SSRI and an equivalent period taking an SSRI. Patients were assessed through markers of aggression, including psychiatric emergencies; restraints; seclusions; as needed (PRN) medication use or STAT medication use for agitation, aggression, violence, poor impulse control, or psychosis; and PRN nicotine use.
Results: There was no statistical significance in any of the analyses demonstrating that SSRI use led to an increased risk of aggression in this sample of inpatients.
Conclusion: The FDA warning of increased risk of suicidality and case reports of aggression potentially associated with the use of certain antidepressants should not prevent prescribers from treating adult patients with SSRI medications.
Keywords: Selective-serotonin reuptake inhibitors, SSRIs, antidepressants, aggression, inpatient psychiatric facility
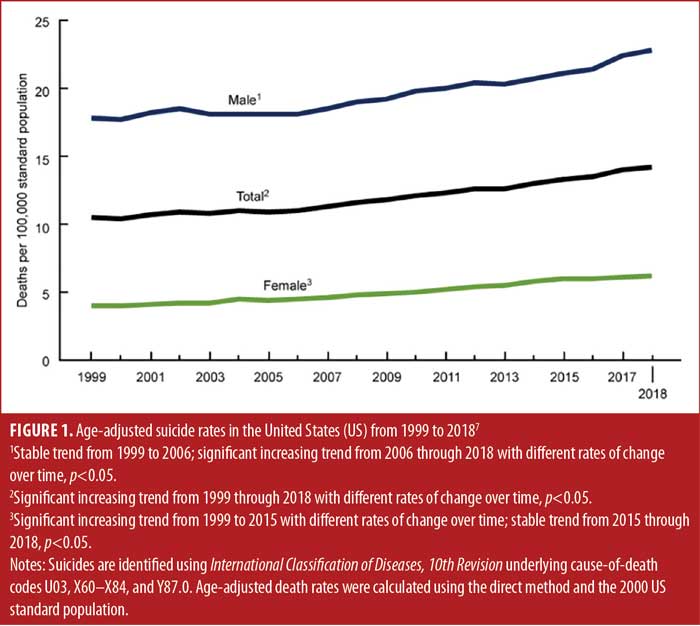
When the first selective serotonin reuptake inhibitor (SSRI) antidepressant, fluoxetine, was introduced to the market in 1987, the SSRI class became commonly prescribed due to the improved safety profile compared with older antidepressants.1,2 As their use increased, they gained multiple indications to treat various mental health disorders, including major depressive disorder, anxiety disorders, and eating disorders.1 However, as early as 1990, studies began to associate the SSRI fluoxetine with violent suicidal preoccupation.3,4 As suicide rates began to increase in the early 2000s, there was further concern that the suicide rate was related to the increased use of antidepressants. In 2003, the United States (US) Food and Drug Administration (FDA) issued a public health advisory regarding suicidality in children and adolescents taking antidepressants, which was followed by a box warning in 2004.1,5,6 The box warning was expanded in 2007 to include adults up to 24 years of age.1,6 The box warning is controversial, and in the meta-analysis that led to the box warning, efficacy of antidepressant therapy was only seen in three out of 15 trials, suggesting that patients were not receiving adequate treatment and were subject to consequences of untreated depression (e.g., suicidality). Despite the box warning, suicide rates have continued to increase throughout the years (Figure 1).7
The initial box warning was developed based on a meta-analysis involving 10,000 patients and 372 studies.8 The meta-analysis indicated that suicidality was observed in four percent of those who received an antidepressant and two percent of those who received the placebo, which was only significant in patients under 18 years of age, with no fatal suicide attempts reported in either group.8 In the studies that led to the expansion of the box warning age to up to 24 years of age, there was an increased risk of suicidality in patients between 18 to 24 years of age, although the risk was not statistically significant.1,8 There is evidence that the box warning might have caused patients to decline antidepressant therapy9 or avoid seeking treatment, and that prescribers became less likely to prescribe an antidepressant, leading to an overall gap in care.5,6,8,9 A survey by Harris1 found that, in the year following the box warning in 2004, there was an 18-percent decline in antidepressant prescriptions. Newer studies have sought to investigate the link between SSRIs and suicidality and have not seen the same correlation, resulting in pressure to reconsider the box warning, given that it has decreased antidepressant prescriptions, leaving those in need of treatment without sufficient or effective pharmacological intervention.10
A meta-analysis by Gunnell et al11 did not show evidence that SSRI use led to an increased risk of suicide, although the study concluded that it would need a much larger sample size to confidently state that there was no correlation. Stone et al12 found an odds ratio of 2.3 for suicidal behavior in patients under 25 years of age taking an antidepressant, compared with the placebo. However, the risk was neutral and possibly even protective for suicidal ideation for patients between 25 and 64 years of age. The study also concluded that, for patients aged 65 years and older, antidepressants reduced the risk of suicidal ideation and suicidal behavior.12 However, this study includes all antidepressants, and SSRIs alone had an odds ratio of 0.86 times the risk for completed suicide when compared to the placebo for all age groups.12
Coupland et al13 investigated suicide and self-harm in people between the ages of 20 and 64 years and found no significant difference when comparing SSRIs and tricyclic antidepressants, but they found an increase in suicide and self-harm with other antidepressants, including venlafaxine, trazodone, and mirtazapine. In a study of 12,692 patients prescribed either fluoxetine, fluvoxamine, or paroxetine, 82 patients had suicidal ideation, and 34 patients died by suicide, which is clinically considered to be a small number of patients and might be attributed to the diagnosis of depression.14
Aggression can be defined as harm to another person, and self-aggression can be defined as harm to self.15 The Overt Aggression Scale (OAS) defines aggression as having four categories: self-aggression, physical aggression against others, physical aggression against property, and verbal aggression.16 Self-aggression can be demonstrated by harm to oneself, including suicidal behaviors,16 which might explain why medications that potentially lead to increased suicidality might also potentially increase aggression. Although the box warning for antidepressants includes suicidality, it does not include information about aggression toward others specifically. The package inserts of SSRIs include agitation, hostility, aggression, irritability, akathisia, anxiety, impulsivity, mania, and hypomania as adverse events that patients might experience when taking these medications.17
There are several hypothesized reasons as to the correlation between suicidality, aggression, and SSRI use. One theory is that the increased serotonergic function of SSRIs2 has an activating effect6,12,18–21 on patients during the first weeks of treatment or during a dose increase,18,19 providing them with energy to act out their aggression before they experience full relief of their depression.6,12 However, Mittal et al22 identified additional studies demonstrating that the risk of suicide might be at its peak one month before patients begin antidepressant therapy, and then slowly declines from that point, suggesting the higher risk of suicide might be due to the antidepressant not providing immediate relief or confirmation bias of the belief that antidepressants lead to suicidality.
Reinblatt et al18 found that 45 percent of pediatric patients prescribed fluvoxamine had an activation event, characterized by increased energy, hyperactivity, impulsivity, and disinhibition, compared to four percent of patients prescribed the placebo. Safer and Zito19 reported that activation events increased with higher doses of SSRIs, and that the patients most vulnerable to the activation were young children, whereas adults had the lowest rate of activation. Dunlop et al23 identified personality changes associated with sertraline use, including an increase in social charm and interpersonal and physical boldness and a decrease in externalization of blame and impulsivity in these patients.
Some studies report that patients with heightened suicidality and aggression might have underlying bipolar disorder misdiagnosed as depression, which could lead to adverse reactions to anitdepressants.24,25 Barlow et al26 found that patients with depression had a statistically significant decreased risk of aggression when compared with patients with other mental health diagnoses at adult psychiatric facilities in Australia. However, the same study found that patients diagnosed with bipolar affective disorder had a 2.81 times higher risk of aggression when compared to patients with other mental health diagnoses. Látalová et al27 conducted a literature review of articles published from 1966 through 2008 and reported that one in four patients diagnosed with bipolar disorder exhibited aggressive behavior, and often this aggressive behavior was linked with manic episodes. Since unopposed antidepressant use has the potential to cause mania in patients with bipolar disorder,17,21,28,29 this could, in part, explain a link between SSRIs and aggression. Preda et al30 found that 8.1 percent of inpatients at the Yale-New Haven adult inpatient psychiatric hospital were admitted due to antidepressant-associated mania or psychosis over a 14-month time period.
There are additional hypotheses for a correlation between SSRIs and aggression. Clarke et al31 connect violence in patients who were prescribed SSRIs with the medication’s side effect of akathisia, which can lead to aggression and suicidality.24 Additional studies identify that SSRI-induced apathy could play a role in violence and aggression.24,32 Drug interactions, polypharmacy, substance use, and genetics are additional contributing factors that might contribute to a link between SSRIs and aggression.32
The currently available studies that investigate SSRIs and aggression show conflicting results, and it is difficult to determine if a correlation exists, especially given the complexity of the patient population and lack of homogeneity between studies. A study assessing lethal violence in the Netherlands over a 15-year period found a negative association between suicide and homicide rates of the patients prescribed SSRIs.33 A study analyzing the entire population of Sweden in individuals over 15 years of age showed an increased rate of violent crime convictions among those prescribed an SSRI, when compared with a timeframe in which they were not prescribed an SSRI.34 This study also showed an increased risk of violence in those prescribed an SSRI, compared to those who were not. However, the increased risk of violent crimes in patients prescribed an SSRI in both arms of this study was only statistically significant in patients 24 years of age or younger, which is consistent with the box warning.34 Patients who were over 24 years of age did not show any correlation between SSRI use and violence.34 A systematic review reported that there was an increased risk of suicidality in adolescents under the age of 18 years, with an odds ratio of 1.92 (95% confidence interval [CI]: 1.51–2.44), but the risk of suicidality decreased for individuals over the age of 18 years, with an odds ratio of 0.57 (95% CI: 0.47–0.70), and even showed a protective effect, with an even further decreased risk of suicidality in adults older than 65 years.35 A systematic review that looked at 45 meta-analyses from 4,471 studies, along with an additional 252 studies identified once sensitivity analyses were adjusted for confounding variables, reported there was not enough evidence to suggest that antidepressant use led to an increased risk of suicide in children and adolescents.36
In contrast, another systematic review reported that antidepressant use led to a two-fold increase in behavior associated with suicide and violence in adults of all ages without any prior psychiatric diagnosis.37 A Danish study on work-related violence in 15,246 individuals saw an increased risk of violence in patients prescribed an antidepressant, with a hazard ratio of 1.38 (95% CI: 1.09–1.75) with antidepressants alone and a hazard ratio of 1.74 (95% CI: 1.13–2.70) in patients prescribed a combination of an antidepressant and anti-anxiety medication, although this study incorporated all antidepressants, not just SSRIs.38 An analysis of data extracted from the FDA’s Adverse Event Reporting System (AERS) over 69 months contained 383 reports of violence believed to be from an adverse drug event caused by an SSRI from 2004 to 2009.39 A Finnish study investigated homicides and identified an adjusted relative risk of 1.31 for patients who were currently using antidepressants, compared with those not prescribed antidepressants.40 In this study, the relative risk for homicide was higher for patients prescribed benzodiazepines and both opioid and non-opioid analgesics than it was for antidepressants.40
Lagerberg et al41 evaluated patients between 5 and 60 years of age in Sweden between 2006 and 2013 and found a statistically significant increased risk in violent crime in patients prescribed SSRIs between 15 and 34 years of age for up to 12 weeks after treatment discontinuation, but there was no statistically significant difference in older age groups. This study also showed that the elevated risk in violent crime had a stronger association in individuals with a previous criminal history.41 A study by Hemminki et al42 investigated 59,120 children born in Finland and found that those prescribed antidepressants were more commonly convicted of violent crimes than those who were not prescribed an antidepressant, and of those prescribed an antidepressant, 76 percent were prescribed an SSRI.
Healy et al24 analyzed data from clinical trials from regulatory agencies and identified an increase in hostile events for both children and adults prescribed paroxetine. They found that the odds of a hostile event are 17 times higher in pediatric patients diagnosed with obsessive compulsive disorder (OCD) than in pediatric patients not diagnosed with OCD.SSRIs have also been identified in criminal court cases as a possible factor leading to violence.4 As early as 2002, prior to the FDA box warnings, there were already 77 cases where fluoxetine was believed to contribute to a crime that was committed.4
With all these studies showing conflicting results, there are differences in opinions of when SSRIs should be prescribed to patients. Furthermore, this evidence might lead to confusion among patients and prescribers. The objective of this study is to determine if there is a relationship between SSRI use and aggressive behavior in an inpatient state psychiatric facility.
Methods
This study was approved by the Institutional Review Board through the New York State Office of Mental Health. Adult patients at a state psychiatric facility in Western New York were included in the study if they were prescribed an SSRI during their inpatient stay between January 1, 2013, and December 31, 2020. Subjects served as their own control. Patients included in the study were required to have an equivalent inpatient time period where they were not prescribed an SSRI. There was a 12-week window between the intervention and control timeframes for each patient to eliminate any residual effects from the SSRI after treatment discontinuation.41 There was also a 12-week window between the control and when SSRIs were initiated to remove a time period where the patient might be experiencing a change in mood or behavior leading up to the prescription of the SSRI that could have led to a confounding variable. Patients were excluded from the study if they had a criminal procedure law designation.
Using a retrospective analysis, aggression was documented by psychiatric interventions, including psychiatric emergencies, restraints, and seclusions. As needed (PRN) medication use and STAT medication use was included as another predictor of aggressive behavior, and these were documented based on the number of medications given for agitation, aggression, violence, poor impulse control, or psychosis. Patients were also analyzed for self-aggression by using the Columbia-Suicide Severity Rating Scale (C-SSRS) to identify individuals with a heightened risk of suicidality, which is defined as suicidal behavior. Nicotine can act as an aid to help calm symptoms of aggression;43 therefore, nicotine cravings were analyzed as a secondary endpoint, which was determined by PRN nicotine use. Data were analyzed using a paired two-tailed t-test, and statistical significance for all endpoints was demonstrated by a p-value of less than 0.05. This study was completed as a retrospective chart review, and therefore, patient consent was not required.
Results
The power analysis was conducted a priori, and the sample size was met and exceeded for the effect size and the significance level for this study. The patient population (Table 1) was 50 percent female and 50 percent male, with the majority of patients identifying as White (78.1%) and not Hispanic or Latinx (90.6%). The average patient age was 52.2 years of age, with an age range 22 to 79 years. Of the 64 patients, 53.1 percent had a primary diagnosis of schizophrenia, and the primary indication for SSRI use was depression in 65.6 percent of patients (Table 1). There was no exclusion criteria for length of SSRI therapy, and the longest SSRI therapy lasted 1,175 days.
All the endpoints to determine patient aggression showed no statistical significance. Patients taking SSRIs had more restraints, seclusions, and psychiatric emergencies while taking an SSRI; however, these results were not statistically significant (Table 2). Additionally, PRN medication use, STAT medication use, C-SRSS score, and PRN nicotine use showed no statistical significance when comparing SSRI use to nonuse in a patient.
The data showed 650 PRNs used when patients were not taking an SSRI and 961 PRNs used when patients were taking an SSRI. The reason for the variability in PRN use was due to patient outliers. One patient used 133 PRNs during SSRI treatment and only five when the patient was without an SSRI. Another patient had 115 PRNs used while taking an SSRI and zero PRNs when they did not take an SSRI. This can also be attributed to the patient complexity. Since patients are taking multiple medications, there are multiple other variables that could potentially lead to these outliers.
Discussion
This study identified 64 patients at an inpatient state psychiatric facility who had equivalent timeframes of treatment with and without an SSRI, and, after assessing patient aggression using psychiatric emergencies, restraints, seclusions, PRN medication use, STAT medication use, and PRN nicotine use, there was no statistically significant evidence to demonstrate that SSRI use led to an increased risk of aggression. In assessing self-aggression through C-SSRS, no association between SSRI use and increase in suicidal behavior was found. Although the FDA box warning is specifically indicated for patients 24 years of age or younger and the youngest patient in this study was 22 years of age, there is still concern by prescribers that aggression, either in the form of self-aggression or aggression to others, can be an undesirable secondary treatment effect of antidepressants for patients of all ages. This study demonstrates that, in this inpatient state psychiatric facility, there was no added increase in risk of suicidality or aggression in our adult patient population.
Limitations. The study site has a limited number of patients who are prescribed SSRIs, leading to a smaller sample size. With the patients acting as a self-comparator, those who had been prescribed an SSRI during their entire inpatient stay were excluded, which had the potential to eliminate longer courses of SSRI treatment. Since the FDA box warning for suicidality applies to persons 24 years of age or younger, it would have been helpful to include pediatric patients, but this facility serves only adult patients. Given the psychiatric histories of this patient population, the patients were prescribed multiple psychopharmacotherapies along with their SSRI, which had the potential to lead to confounding variables. The patients were also similar in demographics, with most of the patients identifying as White and not Hispanic or Latinx. Patient aggression was also based on medical records, which, by the nature of psychiatric emergencies, restraints, seclusions, PRN medication use, and STAT medication use, can limit documentation of all aggressive episodes, especially if de-escalation techniques, rather than medications, were used.
The majority of patients at our facility have the diagnosis of schizophrenia, which means that while taking an antidepressant most patients might also be taking an antipsychotic. A combination of psychiatric medications could have decreased the risk of SSRI use, and the results might differ in a population using SSRIs for depression treatment alone.
An additional limitation is that part of the data was collected both before and during the COVID-19 pandemic. The pandemic limited the number of admissions to the inpatient state psychiatric facility, and admitted patients could not leave facility grounds or have visitors for a period of time during the pandemic. However, the results showed that COVID-19 did not have any statistically significant impact on psychiatric patients and aggression, even though, given the patient population, they might be more likely to have a stress or anxiety response to the pandemic. It is possible that SSRIs helped to limit these effects.
Conclusion
Based on the data collected at a state inpatient psychiatric facility in upstate New York, we saw no increase in aggression, whether directed toward self or others, among adult patients taking SSRIs. This is encouraging, as it is an additional resource demonstrating that SSRI prescriptions when indicated should not be limited in adult patients due to a fear of suicidal behavior or aggression.1,5,6,8,9 Patients who do not seek treatment or prescribers who hesitate to prescribe SSRIs cause a gap in care, and untreated depression can in turn increase the risk for suicidal behavior.5,6,8,9 Suicidal behavior and aggression are important counseling points when prescribing an SSRI, but they should not prevent patients from receiving care. However, more research is needed in patients without additional comorbid psychiatric conditions and psychotherapeutic medications to remove any confounding variables.
References
- McCain JA. Antidepressants and suicide in adolescents and adults: a public health experiment with unintended consequences? P T. 2009;34(7):355–378.
- Walsh MT, Dinan TG. Selective serotonin reuptake inhibitors and violence: a review of the available evidence. Acta Psychiatr Scand. 2001;104(2):84–91.
- Teicher MH, Glod C, Cole JO. Emergence of intense suicidal preoccupation during fluoxetine treatment. Am J Psychiatry. 1990;147(2):207–210.
- Mason SE. Prozac and crime: who is the victim? Am J Orthopsychiatry. 2002;72(3):445–455.
- Libby AM, Brent DA, Morrato EH, et al. Decline in treatment of pediatric depression after FDA advisory on risk of suicidality with SSRIs. Am J Psychiatry. 2007;164:884–891.
- Friedman RA, Leon AC. Expanding the box-depression, antidepressants, and the risk of suicide. N Engl J Med. 2007;356(23):2343–2346.
- Hedegaard H, Curtin SC, Warner M. Increase in suicide mortality in the United States, 1999–2018. NCHS Data Brief, no 362. Hyattsville, MD: National Center for Health Statistics. 2020. https://www.cdc.gov/nchs/products/databriefs/db362.htm#:~:text=Data%20from%20the%20National%20Vital,year%20from%202006%20through%202018. Accessed 8 Mar 2021.
- Friedman RA. Antidepressants’ black-box warning—10 years later. N Engl J Med. 2014;371(18):1666–1668.
- Singh T, Prakash A, Rais T, Kumari N. Decreased use of antidepressants in youth after US Food and Drug Administration box warning. Psychiatry (Edgmont). 2009;6(10):30–34.
- Gibbons RD, Mann JJ. The relationship between antidepressant initiation and suicide risk. Psychiatr Times. 2014;31(12).
- Gunnell D, Saperia J, Ashby D. Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA’s safety review [published correction appears in BMJ. 2006;333(7557):30]. BMJ. 2005;330(7488):385.
- Stone M, Laughren T, Jones ML, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;339:b2880.
- Coupland C, Hill T, Morriss R, et al. Antidepressant use and risk of suicide and attempted suicide or self harm in people aged 20 to 64: cohort study using a primary care database. BMJ. 2015;350:h517.
- Edwards JG, Inman WHW, Wilton L, Pearce GL. Drug safety monitoring of 12,692 patients treated with fluoxetine. Hum Psychopharmacol. 1997;12(2):127–137.
- Liu J, Lewis G, Evans L. Understanding aggressive behaviour across the lifespan. J Psychiatr Ment Health Nurs. 2013;20(2):156–168.
- Yudofsky SC, Silver JM, Jackson W, et al. The Overt Aggression Scale for the objective rating of verbal and physical aggression. Am J Psychiatry. 1986;143(1):35–39.
- Fluoxetine capsule [package insert]. North Whales, PA: Teva Pharmaceuticals USA, Inc. 2020.
- Reinblatt SP, DosReis S, Walkup JT, Riddle MA. Activation adverse events induced by the selective serotonin reuptake inhibitor fluvoxamine in children and adolescents. J Child Adolesc Psychopharmacol. 2009;19(2):119–126.
- Safer DJ, Zito JM. Treatment-emergent adverse events from selective serotonin reuptake inhibitors by age group: children versus adolescents. J Child Adolesc Psychopharmacol. 2006;16(1–2):159–169.
- Luft MJ, Lamy M, DelBello MP, et al. Antidepressant-induced activation in children and adolescents: risk, recognition and management. Curr Probl Pediatr Adolesc Health Care. 2018;48(2):50–62.
- Offidani E, Fava GA, Tomba E, Baldessarini RJ. Excessive mood elevation and behavioral activation with antidepressant treatment of juvenile depressive and anxiety disorders: a systematic review. Psychother Psychosom. 2013;82(3):132–141.
- Mittal V, Brown WA, Shorter E. Are patients with depression at heightened risk of suicide as they begin to recover?. Psychiatr Serv. 2009;60(3):384–386.
- Dunlop BW, DeFife JA, Marx L, et al. The effects of sertraline on psychopathic traits. Int Clin Psychopharmacol. 2011;26(6):329–337.
- Healy D, Herxheimer A, Menkes DB. Antidepressants and violence: problems at the interface of medicine and law. PLoS Med. 2006;3(9):e372.
- Verdolini N, Perugi G, Samalin L, et al. Aggressiveness in depression: a neglected symptom possibly associated with bipolarity and mixed features. Acta Psychiatr Scand. 2017;136(4):362–372.
- Barlow K, Grenyer B, Ilkiw-Lavalle O. Prevalence and precipitants of aggression in psychiatric inpatient units. Aust N Z J Psychiatry. 2000;34(6):967–974.
- Látalová K. Bipolar disorder and aggression. Int J Clin Pract. 2009;63(6):889–899.
- Cicero D, El-Mallakh RS, Holman J, Robertson J. Antidepressant exposure in bipolar children. Psychiatry. 2003;66(4):317–322.
- Strawn JR, Adler CM, McNamara RK, et al. Antidepressant tolerability in anxious and depressed youth at high risk for bipolar disorder: a prospective naturalistic treatment study. Bipolar Disord. 2014;16(5):523–530.
- Preda A, MacLean RW, Mazure CM, Bowers MB Jr. Antidepressant-associated mania and psychosis resulting in psychiatric admissions. J Clin Psychiatry. 2001;62(1):30–33.
- Clarke C, Evans J, Brogan K. Treatment emergent violence to self and others: a literature review of neuropsychiatric adverse reactions for antidepressant and neuroleptic psychiatric drugs and general medicines. Adv Mind Body Med. 2019;33(1):4–21.
- Healy D. Emergence of antidepressant induced suicidality. Primary Care Psychiatry. 2000;6(1):23–27.
- Bouvy PF, Liem M. Antidepressants and lethal violence in the Netherlands 1994–2008. Psychopharmacology (Berl). 2012;222(3):499–506.
- Molero Y, Lichtenstein P, Zetterqvist J, et al. Selective serotonin reuptake inhibitors and violent crime: a cohort study. PLoS Med. 2015:12(9):e1001875.
- Barbui C, Esposito E, Cipriani A. Selective serotonin reuptake inhibitors and risk of suicide: a systematic review of observational studies. CMAJ. 2009;180(3):291–297.
- Dragioti E, Solmi M, Favaro A, et al. Association of antidepressant use with adverse health outcomes: a systematic umbrella review. JAMA Psychiatry. 2019;76(12):1241–1255.
- Bielefeldt AØ, Danborg PB, Gøtzsche PC. Precursors to suicidality and violence on antidepressants: systematic review of trials in adult healthy volunteers. J R Soc Med. 2016;109(10):381–392.
- Madsen IE, Burr H, Diderichsen F, et al. Work-related violence and incident use of psychotropics. Am J Epidemiol. 2011;174(12):1354–1362.
- Moore TJ, Genmullen J, Furberg CD. Prescription drugs associated with reports of violence towards others. PLoS ONE. 2010:5(12):e15337.
- Tiihonen J, Lehti M, Aaltonen M, et al. Psychotropic drugs and homicide: a prospective cohort study from Finland. World Psychiatry. 2015;14(2):245–247.
- Lagerberg T, Fazel S, Molero Y, et al. Associations between selective serotonin reuptake inhibitors and violent crime in adolescents, young, and older adults–a Swedish register-based study. Eur Neuropsychopharmacol. 2020;36:1–9.
- Hemminki E, Merikukka M, Gissler M, et al. Antidepressant use and violent crimes among young people: a longitudinal examination of the Finnish 1987 birth cohort. J Epidemiol Community Health. 2017;71(1):12–18.
- Picciotto MR, Lewis AS, van Schalkwyk GI, Mineur YS. Mood and anxiety regulation by nicotinic acetylcholine receptors: a potential pathway to modulate aggression and related behavioral states. Neuropharmacology. 2015;96(Pt B):235–243.





