
by Adrian R. Johnson, LCSW; Taryn R. Hagerman, LCSW; and Samuel L. Preston, DO
Mr. Johnson is Deputy, Installation Director of Psychological Health, Department of Behavioral Health, Desmond T. Doss Health Clinic in Schofield Barracks, Hawaii. Ms. Hagerman is a Behavioral Health Officer (BHO), Carl R. Darnall Army Medical Center in Fort Hood, Texas. Dr. Preston is an Associate Faculty of Psychiatry, Uniformed Services University of Health Sciences in Bethesda, Maryland, and Psychiatry Consultant, Office of the Army Surgeon General in Falls Church, Virginia.
Funding: No funding was provided for this article.
Disclosures: The authors report no conflicts of interest relevant to the content of this article.
Innov Clin Neurosci. 2022;19(1–3):39–45.
ABSTRACT: The authors explore the impact of cumulative stress on United States (US) military service members (SM), including soldiers and medical personnel, deployed to serve in New York City (NYC) communities. Their mission was to assist in establishing emergency field hospitals during the COVID-19 pandemic. Causative biopsychosocial factors are presented, as well as the impact of wellness checks, which were utilized to monitor the mood and morale of frontline healthcare providers, military personnel, and infected patients in a 2,500-bed emergency field hospital and a 1,000-bed Naval hospital ship operating in the metropolitan NYC area. The authors introduce a self-care and wellness tool, which assesses five core domains (physical, mental, emotional, social, and spiritual) for the purpose of assessing and improving individual overall well-being during periods of heightened stress. This instrument could aid attending medical personnel in identifying patients at risk of suicide. Likewise, the utility of this self-care tool is applicable to both military SM and civilians, and includes soldiers and medical personnel.
Keywords: Self-care, wellness checks, army, soldiers, COVID-19 Response Mission, pandemic, Javits Convention Center (JCC), New York, isolation, quarantine, coping strategies, wellness, military operational stress, physical domain, mental domain, emotional domain, social domain, spiritual domain, self-check tool, 44th Medical Brigade, clinician care, healthcare providers, Joint Base McGuire-Dix-Lakehurst (JBMDL), New Jersey, joint-service operation, humanitarian mission, service members, Title 10 Soldiers, Title 32 Soldiers
As COVID-19-related mortality rates increased, communities began to comprehend the devastating impact of COVID-19. Hospitals were struggling with a lack of manpower to meet the demands of their communities, with consistently increasing mortality rates. In March 2020, as hospital beds in the New York City (NYC) area rapidly filled, hospital staff faced severe challenges as additional personal protective equipment (PPE), ventilators, and other important life-saving equipment were scarce. The COVID-19 Response Mission was established, with military (active and reserve) teams created to augment civilian health care throughout the United States (US).
In NYC, the Javits Convention Center (JCC) was transformed into a 2,500-bed emergency field hospital. The USS Comfort (naval hospital ship) sailed into the harbor and provided an additional capacity of 1,000 hospital beds. The 44th Medical Brigade (MED BDE), from Fort Bragg, North Carolina, was tasked with providing assistance to medical providers and staff, both civilian and military, at the JCC. The 44th MED BDE was fully operational by late March 2020. Integration was paramount amid rising COVID-19 casualties, which were at an estimated 13,000+ laboratory-confirmed and greater than 5,000 probable COVID-19 deaths of NYC residents between March and May 2020, per Weinberger, Chen, and Cohen (2020).1
The 44th MED BDE possessed behavioral health (BH) capabilities, including care from psychiatrists, clinical psychologists (CP), psychiatric mental health nurse practitioners (PMHNP), licensed clinical social workers (LCSW), and behavioral health technicians (BHT). Additional resources provided by the 44th MED BDE included a chaplaincy network, consisting of chaplains and religious affairs specialists (RAS) who provided spiritual and moral support for patients and medical staff. With these capabilities, a multidisciplinary BH clinic was established in the basement of the JCC. BH providers engaged in the provision of healthcare support with the primary objective of easing the psychological distress of patients and healthcare staff. Healthcare support included visiting patients in the wards (in full PPE) and providing additional support to the medical teams. Responsibilities of BH providers increased as the psychological impact of COVID-19 became more apparent.
Psychological Impact of COVID-19
Patient concerns. Presentation and severity of mental health issues varied at the JCC. Stress associated with immediate medical concerns increased as fear of the unknown, isolation, and grief over lost loved ones surged, making previously high-functioning individuals vulnerable to stress-related reactions and those with previously existing biological, psychological, or emotional conditions even more susceptible situational depression and/or anxiety. Requests for psychotropic medication evaluations and BH services increased to help process complex psychosocial stressors, as well as grief and loss issues. To help reframe the significant impact of COVID-19, BH providers conducted mental health safety checks for patients who endorsed suicidal ideation.
Clinician concerns. Increases in patient care directly affected the emotional wellness and physical resiliency of physicians, nurses, and technicians. Exhaustion factored into physiological and psychological strain on healthcare service members. Long shifts without time to decompress possibly impacted access to care and healthcare service delivery due to fatigue and waning concentration. The JCC became a community resource for patients who had severe symptoms, were homeless, and/or were uninsured. Many providers were not assigned to NYC, and discharge planning was a major challenge for patients who were homeless. BH teams experienced burn out and became vulnerable to psychological distress due to unrealistic expectations. The significant impact of COVID-19, along with its causal loss of life, separation from loved ones, and extended operating hours, with few, if any, opportunities for self-care, decreased healthcare service delivery to the community. Providers who contracted COVID-19 or were exposed without full PPE were perceived to be at a higher level of vulnerability to increased stress because of the nature of COVID-19. Common BH symptoms, such as mood alterations, increased anxiety, and difficulty sleeping, subsequently increased due to team members being removed from the team and having to be isolated and/or quarantined.
Family member concerns. Numerous civilian patients cared for in the intensive care unit/intensive care ward (ICU/ICW) of the JCC and other hospital locations throughout NYC and the United States (US) lost family members to COVID-19 while they themselves were inpatients being treated for COVID-19. Additionally, military service member (SMs) lost loved ones to COVID-19. The detrimental impact of the inability to support dying family members and develop some level of closure is significant, and the impact this may have on their future mental well-being is not fully understood. Service members working in civilian hospitals witnessed gruesome scenes of body bags stacked with human remains, coupled with civilian family members unable to see or say goodbye to loved ones who died from COVID-19, and felt an array of emotions, from disassociated apathy to grief and bereavement. Self-care would be vital in this setting as these invisible wounds of tragedy are formidable and diminished attention and quality of medical services could occur.
Military operational stressors. During this period of increased stress, some of the military SMs and civilian staff members developed COVID-19 symptoms. Exposure to a COVID-positive patient resulted in SM placement into isolation or quarantine, even if the SM was asymptomatic. This meant that the SM was restricted to their hotel room for a period of 10 to 14 days. Depending upon exposure, SM status was determined through assessment and contact tracing. SM was then placed into quarantine status to minimize the spread of COVID-19. If the SM developed symptoms of COVID-19 (fever, persistent cough, sneezing, nausea, vomiting, and/or diarrhea), they were placed into isolation status. Periodically, SMs were tested for COVID-19, and upon testing positive, were placed into isolation status for a period not to exceed (NTE) 10 days following the day of the positive test result. Safety was of the utmost importance, and if a SM was exposed and tested positive, even if they were asymptomatic, the SM would remain in quarantine status for a period NTE 14 days.
Addressing Psychological Needs of Patients, Clinicians, Family Members, and Military Personnel
A team of military BH professionals and technicians was deployed to conduct daily wellness checks of military SMs who were isolated or quarantined. The goals of the wellness checks in NYC were simple, yet critical. A BH wellness team would ensure each SM had their basic needs met (food, water, clean laundry, medications, access to support, etc.), provide behavioral health support or resources as requested, and facilitate the coordination of additional care as needed. Communication with military leadership was coordinated as well to identify all concerns.
This team of BH professionals working at the JCC created a resource packet, which was distributed to isolated and quarantined SMs. This was done daily either by request or in person. Wellness packets included information on sleep hygiene, managing anxiety, and tips for developing/practicing resilience during the COVID-19 pandemic. Some of the resilience tips included activities such as sudoku, word searches, and crossword puzzles, and contact numbers for local chaplains, medical sick call, and BH services.
The continuing COVID-19 situation, related deaths, and difficulty managing hectic work schedules was a contributing factor to increased anxiety, depression, and adjustment difficulties. BH services increased as psychosocial stressors became more prevalent within this COVID-19 environment. SMs in the NYC area began to inquire about BH services. BH professionals were able to address the needs of the civilian patients in the ICU/ICW immediately following setup; however, care to SMs did not occur until the second to third week of the COVID-19 Response Mission. It became evident that a mechanism for self-care was necessary. This was in direct correlation to addressing the needs of medical staff (doctors, nurses, respiratory therapists, pharmacy personnel, and administrators) to enhance and optimize their performance over the remainder of the deployment. Overall, 150 to 200 medical staff members received the self-care tool on two separate occurrences, which included passing out a self-care resource.
The redeployment phase at Joint Base McGuire-Dix-Lakehurst (JBMDL), New Jersey, required additional wellness support that was tailored to the needs of SMs (medical professionals) during this phase. Most SMs at JBMDL did not have symptoms or recent known contact with anyone infected with COVID-19, and therefore, the restrictions were slightly different. They were queried about what coping tools would work best for them in a contained environment. Packages of materials based upon the comments from quarantined and isolated SMs were constructed with the hopes of facilitating mood enhancement during the quarantine/isolation period. These SMs were returning from NYC and other northeastern US locales, working in challenging environments with high operational tempo (OPTEMPO) and facing potentially traumatizing experiences. Upon arrival to JBMDL, they were thrust into isolation, and therefore put at risk for additional stressors. The existing wellness packets were then updated to include local contact numbers for medical, BH, and chaplain support; more resiliency-gaining support activities; and information and techniques for practicing gratitude.
Self-care was also administered during this retrograde operations phase of the COVID-19 Response Mission. Self-care and wellness were taught to SMs and leaders in the deployed environment, as well as to soldiers and command teams of military units following the deployment. The materials were presented to SMs and civilians at the local installation and military treatment facility (MTF) upon redeployment from the COVID-19 Response Mission.
Throughout routine aspects of life, stress can and will be experienced. It can be experienced as eustress, distress, or somewhere in between. Eustress is expressed as confident stress brought on by circumstances, such as positive childbirth or energy derived from exercise or physical fitness. Distress is categorized as damaging or catastrophic stress imbued by events such as divorce, job or peer relational difficulties, or bankruptcy. Different stressors encountered in the everyday life of military SMs, who are impacted by the rigors of combat and various military missions, have signaled the need for resilience. After experiencing significantly stressful events, resilient activities can contribute to the attainment of improved health and fitness.
Introduced in the following text is a description of resilience, along with two resilience modalities for possible use. Britt, Sinclair, and McFadden (2013)2 stipulate that resilience is obtained when the procurement of positive adjustment to stressors occurs amid experiencing significant adversity to life events. Within the military resilience construct, research trends which denote recognition of personality characteristics connected to resilience are examined. The way that positive emotions and coping mechanisms interface with increasing resilience is also explored. Positive change occurs when an individual learns how to negotiate external and/or internal stimuli (any controversial source that introduces stress into a person’s livelihood), which subsequently becomes a modality for positive transformation. Upon experiencing the external and/or internal stimuli, resilience can be fortified through the application of a protocol used in a continuous manner to advance health and strength.
For the sake of brevity, two such resilience modes are shared. Troy and Mauss (2011)3 present information on two resilience modalities, Attention Control (AC) and Cognitive Reappraisal (CR), that, if applied regularly in the face of stress, could contribute to robustness of life.
AC3 centers on choosing the path in which one’s attention is focused. It extends itself away from stressful internal or external processes to alter their emotional influence. By purposefully selecting what one absorbs as a focal point and choosing a more optimistic stimulus, the individual can alter the amount of stress they undertake.
CR3 speaks to restructuring an event to amend its emotional outcome from something adverse to something more constructive. Upon recognition of the negative stimulus, this would entail altering one’s assessment to something more affirmative. Both AC and CR are not mutually exclusive.
Enhancing one’s vitality through simple procedures can create resilience. Self-care promotes resilience when applied as a positive change agent during or following a tension-filled or anxiety-provoking circumstance. Additionally, incorporating a recovery/maintenance plan can facilitate a smoother inclination towards resilience. Methods, such as developing two or three different relaxation techniques for use in the physical domain following a stressful workday, can help one to build and maintain resilience. The social domain could contain a maintenance model of communication and listening techniques as part of relationship-sustenance for a spouse or significant other. Meditation can be a form of recovery for the spiritual domain. Attending to personal care can help to decrease the deleterious effects of the biopsychosocial stressors SMs and civilians contend with in everyday life.
Discussion
Civilian patients suffering physical and psychological pain at the JCC was correlated to the adverse impact of the COVID-19 pandemic across the US. Stress associated with combating the pandemic dealt a significant toll on military and civilian healthcare workers. The extraordinary circumstances of the COVID-19 Response Mission illuminated a need for self-care training for medical staff beyond standard army resilience training. According to Baldor (2020),4 BH-related stressors and the effects of the COVID-19 environment contributed to a 20- to 30-percent increase in suicides among US army SMs in 2020. At one installation in mideastern US, 10 soldiers took their own lives, a greater than 50-percent increase from the previous five years combined, speaking to the significance of the moment.6 According to the Department of Defense Suicide Event Reports (DoDSERs) associated with the 10 deaths, biopsychosocial factors that were contributory to the suicides included primary relationship distress, work-related stressors, legal stressors, and financial stressors. Because of these stressors, questions arose, such as “What coping strategies must an individual employ to reduce stress encountered from these stressors as a result of COVID-19 related events?” Additionally, “How does a SM render theirself mission capable amid the numerous stressors confronted throughout this pandemic?” SM resiliency was explored as an alternative to counteract the effects of stress on their lives during combat and other military operations.
The aforementioned stressors are the most notable precursors or risk factors following suicide attempts and completions. While self-care alone is not the solution, the RAND Corporation (2011)6 reported raising awareness and promoting self-care as one of six necessary practices for a comprehensive suicide-prevention program. After reviewing literature, interviewing experts, and evaluating suicide prevention programs in each branch of the military, RAND findings revealed that every branch, including the army, has awareness campaigns and training, but there are very few initiatives directed at promoting self-care, which includes the ability to self-refer for assistance.6 Among the 14 recommendations in this study, researchers advise training to include skill-building in the realms of actions that promote self-care and well-being and building the insight for soldiers to self-refer to services that can assist them when they are feeling overwhelmed.6 Human contact is essential for helping a person choose life over suicide, but individuals must be willing to ask for help from friends, family, or professionals. During COVID-19 Response Missions, BH professionals started sharing self-care resources and tools among both known and suspected at-risk populations as a way of increasing resiliency and the ability to ask for help amidst a fairly isolated population. These efforts alone are never meant to be the solution to suicide; however, teaching and encouraging self-care is the basis for helping individuals learn when they are not feeling well and when they need to ask for additional support.
Another important recommendation was for commanders to receive formal guidance regarding how to respond to a suicide or suicide attempt.6 The army continues to utilize brigade BH officers (BHO) as subject matter experts and advisors to the commanders in BH and wellness matters. Command consultation is regular practice in many brigades across the army, intending to educate, assist, and advise commanders in matters that involve risk and the mental well-being of soldiers in their units. This serves as yet another access point in which a self-care tool could be inserted and applied, not only teaching soldiers important skills in resiliency, but teaching command teams and advocating for soldiers’ environments to match the desired state of wellness as well.
Since its introduction at one army installation, the “Five Essential Components of Self-Care” modality (Appendix 1), comprises five core domains of self-care (physical, mental, emotionall, social, and spiritual), that, if used properly, demonstrates promise for enhancement of an individual’s biopsychosocial functioning and could possibly mitigate risks of suicide. Each domain has five subcomponents. Aspects from each domain of self-care can enhance one’s vitality and should be personalized to fit individual regimens.
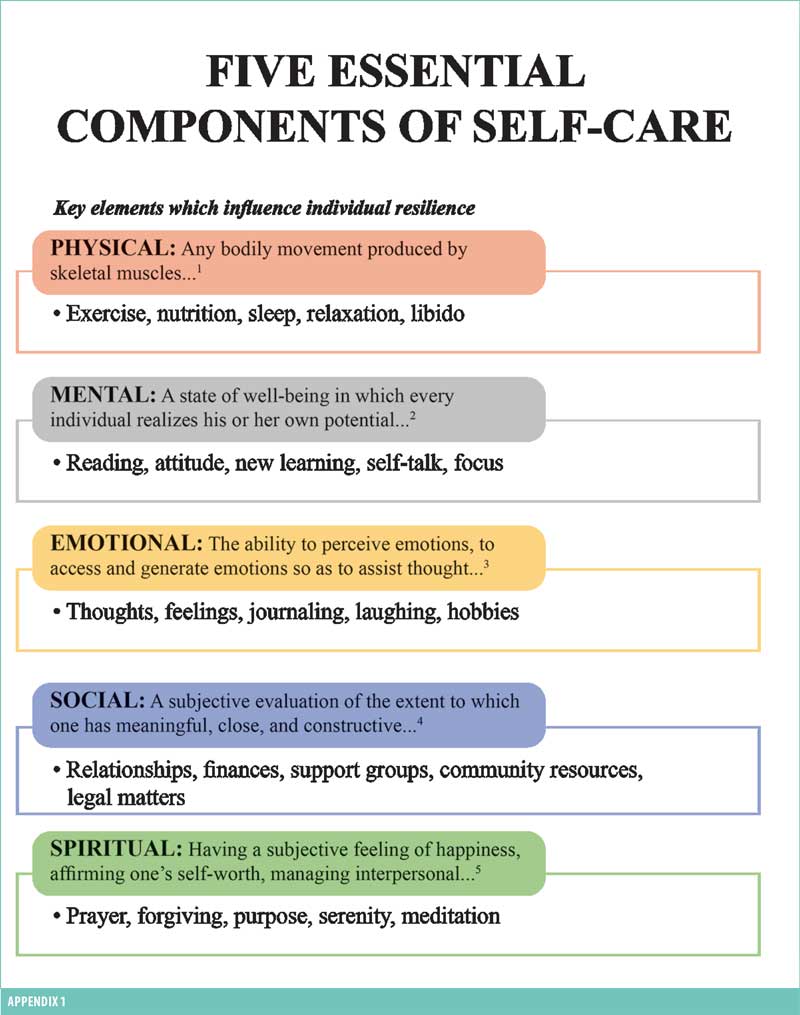
The physical domain is described as “any bodily movement produced by skeletal muscles resulting in energy expenditure,” as indicated by Casperson, Sinclair, and Christenson,7 and comprises subcomponents of exercise, sleep, nutrition, relaxation, and libido. One individual might choose to work on relaxation, whereas another might find that complying with a 10- to 15-minute exercise regimen three days per week improves their physical functioning.
The mental (agility) domain, as defined by the World Health Organization (WHO), according to Manwell et al (2015),8 is described as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.” Cognitive processing from a negative to positive mindset could involve building self-confidence by reciting a mantra, such as “Calm is the key.”
The emotional (intelligence) domain, as per Brannick et al (2009),9 posits “the ability to perceive emotions, to access and generate emotions so as to assist thought, to understand emotions and emotional knowledge, and to reflectively regulate emotions so as to promote emotional and intellectual growth.” Its subcomponents are thoughts, feelings, journaling, laughing, and hobbies. Opportunity to take on a hobby, such as playing a musical instrument, artwork/woodwork, or crossword puzzles, could arouse one’s expressive aspirations.
O’Rourke and Sidani (2017)10 stipulate that the social (connectedness) domain pertains to “a subjective evaluation of the extent to which one has meaningful, close, and constructive relationships with others, including individuals, groups, and society.” Subcomponents of this domain entail relationships, finances, support groups, community resources, and legal issues. Exploration of financial matters as a social construct summons community resources and could build upon one’s social capital. Processes that facilitate connection of the subcomponents of the social domain can become streamlined.
Lastly, the spiritual domain, per Yang et al (2010),11 is defined as “having a subjective feeling of happiness, affirming one’s self-worth, managing interpersonal relationships with an open and accepting attitude, and possessing an internal energy.” Forgiveness, inclusive of the five subcomponents (prayer, forgiveness, purpose, serenity, and meditation) is an agent geared to produce constructive change. Making a choice to forgive oneself and others for past indiscretions affirms self-worth and encourages an internal cleansing or healing process.
The self-care tool is a behavioral health prevention and self-assessment strategic modality utilized to assess individual wellness by analyzing one’s ability to cope with life stressors from five specific domains. Sharing the utility of this tool was met with verbal affirmation from military leaders. Due to the absence of a tool that would provide internal validity to SM and civilian staff member resilience, it is immensely difficult to ascertain tangible results. According to studies conducted by Hoyt and Holtz (2020),12 army-wide protocols used to mitigate suicide have been largely ineffective, despite the lack of specific studies which assess the effect of prevention efforts. Some of the army’s current initiatives aimed at preventing suicide and/or increasing resiliency include Master Resiliency Training (MRT); Applied Suicide Intervention Skills Training (ASIST); and Ask, Care, Escort (ACE).12 Secondarily, pre- and post-surveys have not been administered for a randomized clinical trial (RCT) in order to begin to assess for internal validity. Rapid mission change and time constraints of the COVID-19 Response Mission did not allow for measurement of the effects or results of the self-care protocol’s administration. Lastly, the efficacy of this self-care tool can be realized through its use in routine therapy sessions, which measure wellness and guide clinical practice.
Part II of the self-care tool administration will involve conducting a RCT featuring soldiers at 2 to 3 different US army installations. Experimental and control groups comprising approximately 30 soldiers each will be requested for the testing. Prior to administration of the self-care tool to the experimental group, personnel in both groups will be administered a pre-survey of 20 questions. The personnel in both groups with then be administered the self-care tool; however, the personnel in the experimental group will be taught the rational emotive behavioral therapy protocol as a measure to facilitate greater understanding and awareness of the self-care tool’s utility. The control group will only be administered the self-care tool. Ninety days after the pre-test, a post-survey test of the same 20 questions will be administered to both groups, with the results noted to see if there were improvements in the biopsychosocial functioning of the personnel in either group based upon the post-survey scores.
This work is the initial effort involving self-care with a view towards utilization as an assessment tool to guide which types of modality a clinician can use in practice. It will require additional research to validate its efficacy. Further research will be conducted to determine efficacy and whether or not it will be useful to continue in clinical practice settings.
Conclusion
The significant impact of the COVID-19 Response Mission, along with other military endeavors and life events, have called for examination of protocols to teach resilience and to augment individual care, for the purpose of sustaining life in the US Armed Forces. Conducting self-care is one mechanism that can facilitate SM understanding of some of the biopsychosocial stressors SMs face in their daily lives. Having a grasp of this knowledge can create an opportunity to engage in personal care to optimize one’s functionality. Self-care is a useful protocol and is vital to the improvement of SM biopsychosocial sustenance. Following the COVID-19 Response Mission, as military operations and other endeavors continue, self-care training and BH wellness checks could be essential utilization techniques to facilitate the optimization of soldier and civilian health and fitness and overall functioning. When asked how he would spend two additional hours added to his day, Robert Boland, MD, Chief of Staff, Menninger Institute, Houston, TX, responded, “I think we could all benefit from more time for self-care, self-reflection, reading for pleasure, enjoying nature and spending time with family and friends.”13
Although adding the self-care tool and advocacy to soldiers’ daily practice to enhance coping and continued command consultation alone cannot eradicate suicide, these self-care domains are viewed as essential components to an effective suicide prevention program. As such, efforts should increase to reach as many soldiers and leaders as possible.6 Prevention remains as the traditional focus for absolving suicide. The concept of self-care is in direct support of this but approaches it from a crucially different angle. Self-care provides wellness, peace, and meaning. Therefore, instead of solely keeping patients alive, self-care helps soldiers find meaning in life and, ultimately, a desire to live. The Department of Defense’s Strategy for Suicide Prevention validates the development of a tool focused on facilitating the practice of self-care.14
Disclaimer
The views expressed in this material are solely those of the authors and do not necessarily represent those of the US Army, Department of Defense, or its affiliates. Additionally, other self-care tools exist; however, the other resources do not contain the exact specifications of the self-care tool provided with this article.
References
- Weinberger DM, Chen J, Cohen T, et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern. 2020;180(10):1336–1344.
- Britt TW, Sinclair RR, McFadden AC. Introduction: the meaning and importance of military resilience. In: Sinclair RR, Britt TW, eds. Building psychological resilience in military personnel: theory and practice. American Psychological Association; 2013:3–17.
- Troy AS, Mauss IB. Chapter 2: Resilience in the face of stress: emotion regulation as a protective factor. In: Southwick SM, Litz BT, Charney D, Friedman MJ, eds. Resilience and mental health: challenges across the lifespan. Cambridge University Press; 2011:30–44.
- Baldor L. Military suicides up as much as 20% in COVID era. The Associated Press. 27 Sept 2020. https://apnews.com/article/virus-outbreak-air-force-stress-archive-army-be5e2d741c1798fad3f79ca2f2c14dd. Accessed 9 Apr 2021.
- Pruitt LD, et al. Department of Defense Suicide Event Report (DoDSER): calendar year 2020 annual report, no. 0-A2345. Washington, DC: Defense Health Agency; 2020:iv.
- Ramchand R, Acosta J, Burns R, Jaycox L, and Pernin C. The war within: Preventing suicide in the US military. RAND Corporation; 2011.
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131.
- Manwell LA, Barbic SP, Roberts K, et al. What is mental health? evidence towards a new definition from a mixed methods multidisciplinary international survey. BMJ Open. 2015;5(6):e007079.
- Brannick MT, Wahi MM, Arce M, et al. Comparison of trait and ability measures of emotional intelligence in medical students. Med Educ. 2009;43:1062–1068.
- O’Rourke HM, Sidani S. Definition, determinants, and outcomes of social connectedness for older adults: a scoping review. J Gerontol Nurs. 2017;43(7):43–52.
- Yang CT, Yen SY, Chen JO. [Spiritual well-being: a concept analysis]. Hu Li Za Zhi. 2010;57(3):99–104.
- Hoyt T, Holtz PM. Challenging prevailing models of US army suicide. The US Army War Quarterly Parameters. 2020;50(4):7–19.
- Meet the next chief of staff. Connections Newsletter. 2020;12(9):1.
- Department of Defense. Strategy for suicide prevention. 2015. https://www.dspo.mil/Portals/113/Documents/TAB%20B%20-%20dssp_final%20USD%20PR%20signed.pdf. Accessed 26 Jan 2022.





