by Andrew B. Correll, MD; Terry L. Correll, DO; and Matthew C. Correll, BS Candidate
by Andrew B. Correll, MD; Terry L. Correll, DO; and Matthew C. Correll, BS Candidate
Mr. A. Correll is with Wright State University Boonshoft School of Medicine in Dayton, Ohio. Dr. T. Correll is Clinical Professor, Department of Psychiatry, Wright State University Boonshoft School of Medicine in Dayton, Ohio. Mr. M. Correll is a student at Wright State University Raj Soin School of Business in Dayton, Ohio.
Funding: No funding was provided for this study.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Innov Clin Neurosci. 2024;21(7–9):15–21.
Department Editor
Julie P. Gentile, MD, is Professor and Chair of the Department of Psychiatry at Wright State University in Dayton, Ohio.
Editor’s Note
The patient cases presented in Psychotherapy Rounds are composite cases written to illustrate certain diagnostic characteristics and to instruct on treatment techniques. The composite cases are not real patients in treatment. Any resemblance to a real patient is purely coincidental.
Abstract
Bibliotherapy, a relatively underutilized lifestyle intervention in psychotherapy, is a unique cost-effective avenue of treatment that empowers patients by integrating therapeutic reading into their treatment plan. This approach strategically uses empirically validated cognitive-behavioral and self-help literature to facilitate the application of therapeutic topics outside of psychotherapy sessions. Bibliotherapy’s range of administration styles highlights its potential as an adjunct to medication, psychotherapy, and/or healthy lifestyle interventions in a comprehensive treatment plan. Most meta-analyses conducted so far regarding bibliotherapy in a clinical setting consist of studies that use minimal patient interaction via short phone calls or emails. Despite this, meta-analyses show medium-to-large effect sizes that are comparable to traditional psychotherapy modalities for common disorders, most notably depression. This article explores the practical implementation of bibliotherapy research via an example psychotherapy session with a patient who has a diagnosis of major depressive disorder (MDD). An evidence-based reading list is proposed alongside a decision tree and actionable clinical insights for the effective implementation of bibliotherapy.
Keywords: Bibliotherapy, psychotherapy
An optimal psychotherapy patient would be one who is deeply engaged in the therapeutic process, extending the impact of what is discussed beyond the confines of the office. This individual might take ideas home, mull them over with curiosity, and dedicate time for such processing. An ideal psychotherapy patient would likely proactively seek out additional information about their condition so they can understand for themselves how to best proceed in the healing journey. They would maintain an openness to multiple viewpoints about what could be occurring and would likely bring unique perspectives on their situation to the psychotherapy session derived from thoughtful reflections at home. How can a psychotherapist foster an environment where patients are so empowered? One potential solution would be to handpick some of the clearest thinkers in the psychiatric community and have patients read the most impactful material relevant to their situation. This can be achieved with the relatively underutilized healthy lifestyle intervention known as bibliotherapy.
Bibliotherapy has been defined as an “interaction between the reader and certain literature which is useful in aiding personal adjustment.”1 There is no standard set of reading material that is universally studied, though excellent lists have been created.2 In fact, given findings of how patients who are more actively involved in their treatment plan have better diabetes control,3 it is likely more beneficial for the patient in psychotherapy to actively research material and then come to the clinician with reading options that can be discussed together.
Various administration methods have been explored in trials of bibliotherapy. One style is almost an entire replacement for a normal course of psychotherapy utilizing reading assignments along with short (around 5-minute) follow-up telephone calls.4 Other styles include bibliotherapy as an adjunct to medication-based treatment, as an adjunct to psychotherapy, or as a talking point in a more traditional course of psychotherapy. Through continuous engagement with therapeutic content outside the office, bibliotherapy could help stimulate new insights in our patients. Having high-impact reading material can also serve as a springboard for deeper discussions than previously enabled in a patient’s course of psychotherapy. Such empowerment can help patients become better aware of others’ struggles and troubleshoot after psychotherapy termination5 through rereading the material.6 For example, psychotherapy might initially outperform bibliotherapy in treating depression, but one study showed that bibliotherapy participants continued improving, leading to no significant differences between groups after a three-month follow-up.7 This article aims to provide an overview and guide for the practical application of bibliotherapy, an exciting tool psychotherapists can utilize to provide optimal care.
There is a shortage of psychiatric care in the United States (US), as a recent sampling found that only 18.5 percent of psychiatrists were taking new patients, with a median wait time of 67 days.8 The potential for bibliotherapy is significant since it might allow psychotherapists to see more patients in less time while also placing the selection and “dosage” of the reading material in the patient’s control.
Integrating readings with psychotherapeutic goals can bolster and reinforce material discussed in previous sessions. Many psychotherapists (68%) reported using bibliotherapy in one study, with a positive correlation between overall counseling experience and use of bibliotherapy.9 Another survey found a 60.3-percent prescription rate of self-help books in psychotherapy, but notably, eight percent of psychologists had been informed by patients of harm from self-help readings.10 Patients can be expected to follow through with the assigned readings, as in one trial lasting four weeks, the average percentage of the lengthy and comprehensive Feeling Good book that was actually read was 83 percent.11 Tailoring reading level to the patient will make it more likely the patient will not only read the material but also enhance their understanding, as 15 percent of the US population and 34 percent of non-US-born adults in the US have low English literacy.12 Dropout rates for prescribed bibliotherapy might be higher in those with lower education.11 Tailoring language to a patient’s understanding might improve general medical outcomes in other settings,13 but making sure there is clear communication is important because patients often actively conceal illiteracy because of social stigma.14 Bibliotherapy can also put complex psychiatric jargon into more understandable terms.5,15
Most studied forms of bibliotherapy involve a personal meeting at the beginning and subsequent weekly telephone calls for 5 to 15 minutes in which the psychotherapist gives support.16 This style seems to be quite effective,16 and with different protocols, psychotherapist time is only weakly positively correlated with outcome measures.17 A lending library within the physician’s office or collaboration with a local librarian who has a particular interest in the therapeutic value of reading can increase accessibility for patients.2 Book clubs or even the discussion of a particular book in group psychotherapy could be a great way to obtain healthy socialization. Bibliotherapy might thereby help patients obtain treatment who otherwise might not because of the stigma and/or the mental healthcare shortage in the US. Greater efficiency could help with providing psychotherapy in light of decreased insurance reimbursement for psychiatrists to provide such modalities, as there is a national trend toward the use of psychopharmacology as the only treatment for mental health outpatients. Between 1998 and 2007, the number of individuals treated solely with psychotropic medication increased from 44 percent to 57 percent. In contrast, during the same period, the use of psychotherapy alone as a treatment decreased from 15.9 percent to 10.5 percent.18
Clinical Case Vignette 1
A 68-year-old male individual, Mr. Z, presented for initial psychiatric evaluation reporting that, “Everything seems like its colored black and gray; where colors once danced, now I feel like it is all so monochrome.” The patient denied any history of color blindness, visual disturbances, or taking medications known to impact color vision (digoxin/ethambutol).
Dialogue 1
Psychiatrist: Thanks for the beautiful description. Could you tell me more about what you meant by seeing everything as “monochrome?”
Mr. Z: It’s like the joy and excitement that colored my world is gone, leaving everything dull and less enjoyable.
Psychiatrist: What do you think is contributing to this?
Mr. Z: A lot of things just aren’t as they used to be. Over the last few years, I have been less able to get out and move around because of bad knees, and all my friends are passing away, so it feels like my world has gotten a lot smaller. I find myself dreaming at night about the “good old days.”
Psychiatrist: It sounds like numerous losses and disappointments for you.
Mr. Z: I can’t sleep very well either and only get about four hours a night. I feel tired all the time and have a reduced appetite, and I feel guilty for missing many social obligations, too, because of all this.
Psychiatrist: Does feeling tired affect your ability to think clearly?
Mr. Z: It seems I am not as sharp as I was even six months ago. It is mainly with minor decisions. I can still make chess moves with my buddies even though it is not as much fun anymore, but just calling here to schedule an appointment was a struggle. I contemplated so long what I should wear to come here, too. Even at the grocery, the poor lad behind me probably thought I was trying to decipher the Da Vinci Code in front of the spice display.
Psychiatrist: Well, it sounds like you can orchestrate a checkmate, but when it comes to the spice rack, it is more of a stalemate! When did you start to notice the sleep and interest problems?
Mr. Z: About four months ago, now that I think about it.
Practice Point 1
It is important that with bibliotherapy, a professional is still involved so that the patient is not working with therapeutic techniques without the correct diagnosis.16 For Mr. Z, his symptoms seemed to be causing clinically significant distress despite how older patients tend to spend more time in lighter stages of sleep (N1 and N2) as they age,19 which can make clinical assessment more challenging. Fatigue is not a universal symptom in the elderly, though mild fatigue can be present in more than half of elderly adults,20 so “feeling tired all the time” is a red flag and suggests his sleep is less than optimal.
Using humor in therapy can be delicate, but since the patient amusingly compared indecision to the Da Vinci Code, it was appropriate for the psychiatrist to be light-hearted as well. If empathy, genuineness, and positive regard are embodied by the psychotherapist, humor is more likely to be successful.21 The patient’s indecision about the spice rack was indicative of concentration concerns, a diagnostic criterion for major depressive disorder (MDD).22 Those with severe depression might be at a disadvantage in using bibliotherapy because of concentration difficulties, which should be considered by the psychiatrist in Mr. Z’s case.16
Four months might seem like a long time for Mr. Z to feel depressed, but one study indicated that the median duration of depressive episodes is three months.23 This patient meets the minimum of five of nine criteria for a diagnosis of MDD.22 A consensus can now be reached on formulating an optimal treatment strategy for his MDD, grounded in a robust “three-pronged stool” approach to potentially include healthy lifestyle interventions, psychotherapy, and/or psychiatric medication.
Clinical Case Vignette 1, Continued
After more exploration during the intake appointment, the psychiatrist was ready to make a treatment recommendation.
Dialogue 2
Psychiatrist: I think you have MDD, and here are the criteria that apply to you…(goes through the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision [DSM-5-TR] with the patient). What are your thoughts about that?
Mr. Z: I think what you have described is accurate.
Psychiatrist: There are three treatments we might consider. Some people prefer medication. Others prefer psychotherapy. A third option is healthy lifestyle interventions by themselves or along with psychotherapy, medication, or both. One healthy lifestyle intervention that I believe could be very beneficial for you would be bibliotherapy, which involves therapeutic reading. Do you have any preferences among the treatment options that I have offered to you?
Mr. Z: Hmm, I like the idea of therapy and reading, since I enjoy reading the newspaper so much already.
Psychiatrist: Great! We can set you up for weekly psychotherapy and weave in talking about a book. So, during the next week, I would like you to do some research on a book about depression that you would like to read. I promise, most books on the topic are not actually depressing, despite the subject matter! One really good book is Feeling Great by David Burns, which has helped others a great deal, if you need a starting place.
Mr. Z: Okay, sounds good. I will look around and let you know next week what I find. Could I listen to a book instead? Might make it more fun to mow the grass.
Psychiatrist: Sounds like a plan!
Practice Point 2
The psychiatrist in this example went through the DSM-5-TR criteria for MDD with Mr. Z. One survey found that 50 percent of psychiatrists “sometimes” or “often/always” review the DSM criteria with the patient and/or family,24 and doing so, in the authors’ experience, is appreciated by patients and their families to enhance diagnostic clarification and trust with the clinician.
Bibliotherapy might be more helpful in those patients who find solace in drawing parallels between their experiences and metaphorical examples.25 For sensitive topics, patients might feel less defensive about using metaphors from their reading to describe difficulties in their own life because the pattern first belonged to someone else.25 One of the co-author’s former patients brought in a book with underlined symptoms of psychosis that he was afraid to mention verbally in session. For Mr. Z, he initially compared depressive-like symptoms to seeing things as “dull” around him. He displayed “all-or-nothing thinking” describing that “all [his] friends are passing away” despite later mentioning chess acquaintances he still sees. Cognitive behavioral therapy (CBT)-based reading (like the well-researched Feeling Good book, recently updated to Feeling Great) might thereby be an effective suggestion if he had no idea where to start, but the psychiatrist wisely let him lead the way. For those with limited freedom in a psychiatric or forensic setting, the ability to choose readings might be disproportionately more meaningful.
Regarding treatment for depression, there is evidence that bibliotherapy has surprising benefit. A Cohen’s d value of 0.2 is considered small, 0.5 is medium, and 0.8 is large. As a benchmark, a meta-analysis by Cuijpers et al26 published in JAMA regarding general psychotherapy for depression found an effect size of d equals 0.75. Specifically concerning how bibliotherapy might relate to Mr. Z’s clinical scenario, a meta-analysis by Gregory et al27 of 29 studies of cognitive bibliotherapy for depression found an effect size of d equals 0.77. Den Boer et al28 conducted a meta-analysis of 13 bibliotherapy studies and found an effect size of d equals 0.84, with a greater effect in more severe illness. Cuijpers et al16 found an effect size of d equals 0.82 with six trials of bibliotherapy for unipolar depression, which was comparable to individual or group psychotherapy (as a reminder, Cuijpers et al26 found general psychotherapy for depression to have an effect size of d=0.75). Another study by the same group directly compared guided self-help and face-to-face psychotherapy for depression and anxiety treatment and found no significant difference with up to one year of follow-up.29
In a younger demographic, research indicates that bibliotherapy, even without counseling, is notably effective versus control conditions at treating depression and anxiety. The effect was more pronounced in treating depression, which is applicable to Mr. Z.30 This meta-analysis examined studies using the common application method of bibliotherapy: self-help materials with time-limited weekly calls or emails. Check-ins usually involved asking about the number of pages read and the number of exercises completed.30 If Mr. Z displayed self-harming behavior with his depression, data from a small trial suggests bibliotherapy might also help with 46-percent less cost compared to usual treatment.31 Importantly, the positive effects of bibliotherapy on depression seem to last, with benefits observed up to three years postintervention.32
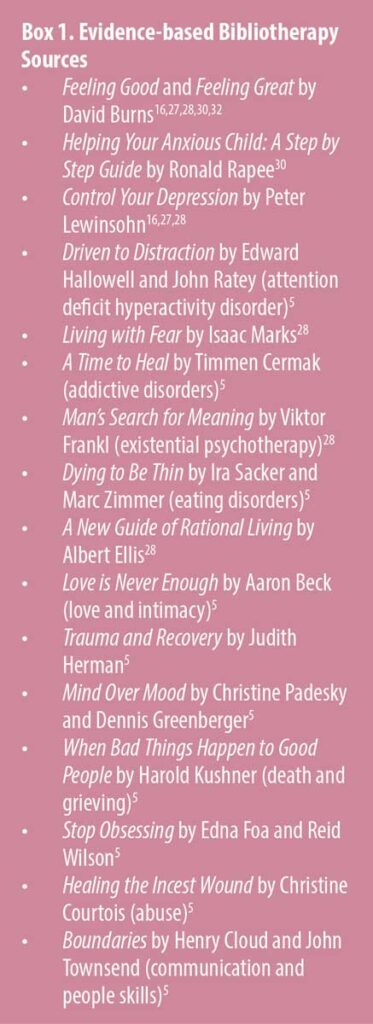
Extending beyond depression, one of the most comprehensive33 meta-analyses of bibliotherapy was conducted by Marrs et al,17 which found more prominent effects of bibliotherapy on assertion, anxiety, and sexual dysfunction, along with improvement in depression. Among 68 studies in this analysis, retention was about 84 percent, and 54 percent of the interventions required homework assignments other than reading. Reading materials from these studies were primarily grounded in CBT principles, including works such as Feeling Great by David Burns, Man’s Search for Meaning by Viktor Frankl, Living with Fear by Isaac Marks, and Control Your Depression by Peter Lewinsohn. Many other bibliotherapy studies use unpublished self-help manuals or letters with success.31,34 Box 1 contains a list of evidence-based bibliotherapy sources.
Bibliotherapy seems to be able to help reduce alcohol intake in 11 of 12 studies of a meta-analysis (d=0.65–0.80).34 Addressing any alcohol use by Mr. Z is an important role of the psychiatrist because of a heightened risk of suicide attempt with acute alcohol consumption (7-fold increased risk)35 and the depressing side effect of alcohol itself, which could overwhelm other treatment modalities. Screening Mr. Z for sexual dysfunction is important as well, as one meta-analysis found 82 and 63 percent of women and men, respectively, with MDD had sexual dysfunction.36 If this were to be present for Mr. Z, bibliotherapy might also help; a meta-analysis of nine trials concerning sexual dysfunction found bibliotherapy to be effective (d=0.68).37
Apart from the patient, bibliotherapy might help caregivers. A meta-analysis involving 1,036 caregivers of those with neurocognitive disorders found that bibliotherapy reduced depression and anxiety and improved self-efficacy.38 Uniquely, four of the studies used videos in their definition of bibliotherapy that were tailored to stress management and other relevant topics. This research is encouraging for treating this distinctive population of people (caregivers) who have more prevalent depression and anxiety than the general population.38 Furthermore, it addresses a concerning correlation where poorer caregiver mental health is associated with increased patient mortality rates.39
While not explored in the research as much as cognitively based books, fiction reading could potentially be of use with the controlled introduction of vicarious life experiences. Passages encountered through bibliotherapy might mirror situations the patient might not have navigated well in their lives.40 From a psychodynamic perspective, a patient’s interpretations of reading passages can be a projective process and give insight into internal representations of stories, characters, or themes they have experienced.25
Following Mr. Z’s suggestion to listen to a book was wise by the psychiatrist. A further step could have been to advise exercise, such as walking, along with the listening, since exercise has potentially moderate effects on depression by itself (g=0.43–0.50).41,42 In a population of cardiac rehabilitation patients, audiobooks were equal to rhythmic music in increasing positive affect associated with exercise and lowering perceived exertion.43 Such interventions might increase the amount of time exercised43 and overall satisfaction (compared to white noise), while also providing therapeutic insights outside of psychotherapy.
Clinical Pearls
- Listening to a podcast or audiobook might make exercise more enjoyable and more likely to be repeated, as well as enhance a sense of achievement.
- Audiobooks might be easier to find the time to read than a physical book, as one can reinforce and extend topics discussed in therapy by simply listening during multitasking opportunities, such as commutes.
- Audio-assisted reading might improve comprehension for patients with reading disabilities44 and those who speak English as a second language.45
- Asking the patient what topics they are interested in is wise to support autonomy and encourage “buy in.”
- Asking about key takeaways from their reading is helpful, and allowing enough time for the patient to think about an answer might promote more helpful dialogue. In peer instruction classes, it appears a longer “thinking period” after questions promotes more discussion.46
- If the patient is reading a fictional book, the psychotherapist can ask about similarities they see between any characters and their own lives to facilitate higher-order introspection and helpful discussion.
- For married individuals, having the spouse read a book as well could be a support for the patient.40
Clinical Case Vignette 1, Continued
After several sessions, Mr. Z and the psychiatrist had the following conversation:
Dialogue 3
Psychiatrist: Where would you like to begin?
Mr. Z: My week could have been better. My wife was really sick, and I had to take care of her a lot this week.
Psychiatrist: I am really sorry to hear that. I remember you telling me that she had severe heart disease. Was it related, if you don’t mind me asking?
Mr. Z: Yes, they thought she had a heart attack, but thank God she didn’t. When you are our age, nothing seems to work anymore, but at least I still have her. I thought I might lose her.
Psychiatrist: On the one hand, you were scared about losing your wife, but on the other hand, I imagine that reminded you how much you love her, right? (double-sided reflection)
Mr. Z: I agree, sometimes you have to get close to losing something to remember how much it means to you.
Psychiatrist: That is a profound way of putting it. I know we discussed the Feeling Great book you have been reading recently. Anything you learned there that applies to this situation?
Mr. Z: (takes a moment to think) I suppose I was initially “catastrophizing” that she was going to die, which was entirely overwhelming to me.
Psychiatrist: Please say more about how you were feeling at the hospital and what was going through your mind.
Mr. Z: I was a complete wreck until the doctors told me that she did not have a heart attack and would not die. Then my thoughts turned toward feeling love and appreciation that we have been together as long as we have.
Psychiatrist: It’s quite insightful of you to utilize the principles from the book you have been reading to navigate this very difficult time.
Mr. Z: The book has been very helpful. In fact, I was reading during some of the downtime while nurses came in every now and then. The few principles from the book I shared with my wife even helped calm some of her anxiety.
Psychiatrist: Even though this was a very stressful event for the two of you, it allowed you to practice some of the principles you’ve been reading about, share them with your wife, and be grateful for your long marriage together.
Mr. Z: You betcha. It was very pleasant supporting her in the hospital and recounting our many years together.
Practice Point 3
The psychiatrist started with a neutral question to empower the patient to steer the conversation toward what is most profitable to discuss and later intentionally inquired about both emotions and cognitions. Remembering that his wife had heart disease demonstrated caring and engagement. The psychiatrist also used a double-sided reflection, which is helpful in processing complicated emotions, and provided reinforcement of applying the book’s ideas to his situation. The psychiatrist repeated and reflected the patient’s feelings to reinforce some of the important lessons Mr. Z learned during his challenging week.
Clinical Pearls
- Adjust how much or how little to talk about outside readings based on feedback during the session or your psychotherapeutic goals.
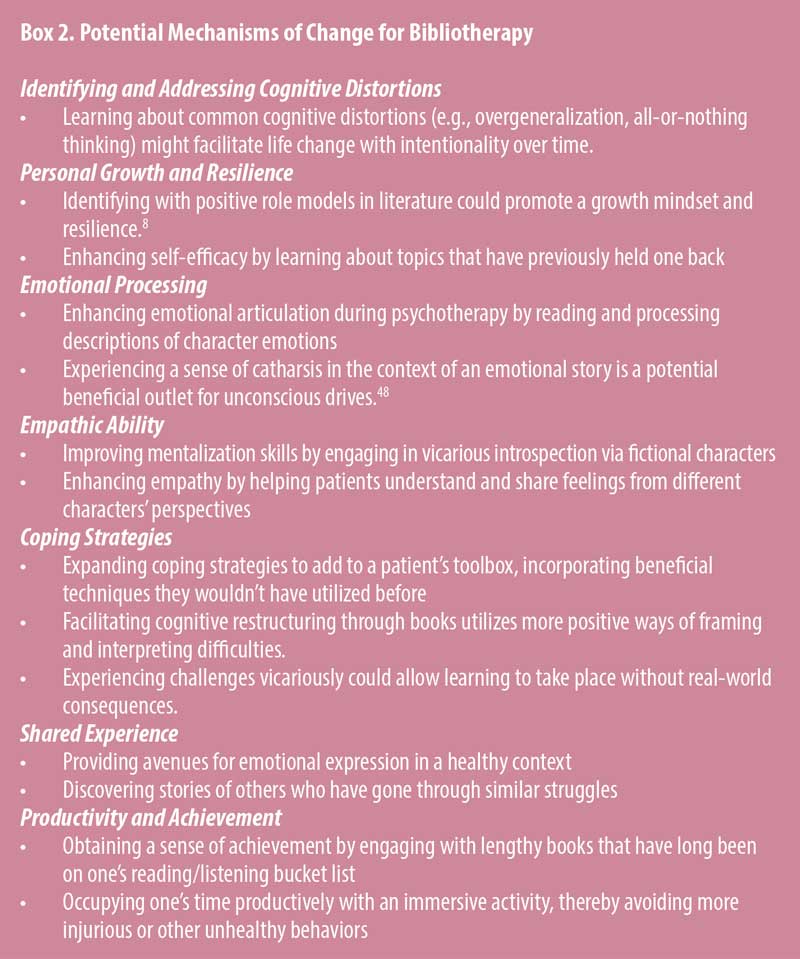
- Active reading strategies might promote recall of material more than passive reading,47 so encourage note-taking and writing down questions during reading sessions. These insights could be explored in psychotherapy (Box 2).
- Starting with shorter reading assignments could prevent discouragement. Advise that the patient stop reading sessions at defined end points, like the end of chapters. Such a bite-sized approach might help patients feel a sense of accomplishment as they progress.
- When a particularly profound insight arises, encourage application of the material they found helpful during bibliotherapy to the troubling situation in their own life. This moment of connecting their experiences with the reading has been called a “shock of recognition.”48
Conclusion
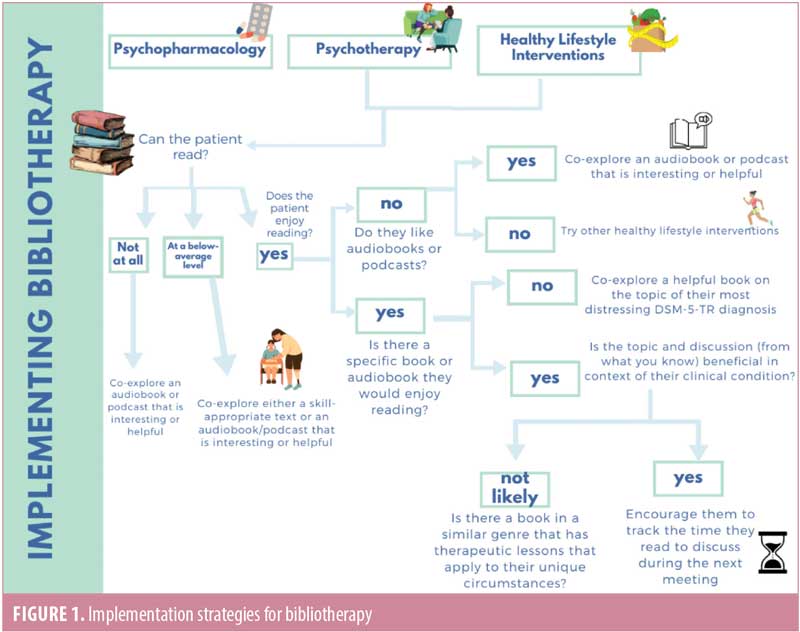
Bibliotherapy emerges as an accessible, cost-effective strategy to increase access to mental healthcare and enrich discussions in psychotherapy. Having demonstrated moderate-to-substantial efficacy in treating depression and various other disorders underscores its viability as a clinical intervention. Adapting to a patient’s unique reading level needs while incorporating their selection of topic empowers the patient (Figure 1). Implementing bibliotherapy as a healthy lifestyle intervention alongside traditional psychopharmacology and psychotherapy would likely augment the therapeutic benefits obtained. More research comparing specific reading materials would be helpful in different disorders. Additionally, comparing diverse delivery methods, such as video, audio, and traditional print, potentially broadens the scope and appeal of bibliotherapy. This exploration could lead to a more nuanced understanding of how various formats influence patient engagement and treatment efficacy.
References
- Lindeman B, Kling M. Bibliotherapy: definitions, uses and studies. J Sch Psychol. 1968;7(2):36–41.
- Anstett RE, Poole SR. Bibliotherapy: an adjunct to care of patients with problems of living. J Fam Pract. 1983;17(5):845–853.
- Coulter A, Entwistle V, Gilbert D. Sharing decisions with patients: is the information good enough? BMJ. 1999;318(7179):
318–322. - Moldovan R, Cobeanu O, David D. Cognitive bibliotherapy for mild depressive symptomatology: randomized clinical trial of efficacy and mechanisms of change. Clin Psychol Psychother. 2013;20(6):482–493.
- Campbell LF, Smith TP. Integrating self‐help books into psychotherapy. J Clin Psychol. 2003;59(2):177–186.
- Kramer K. Using Self-Help Bibliotherapy in Counselling. Lethbridge, Alta.: University of Lethbridge, Faculty of Education; 2009.
- Floyd M, Scogin F, McKendree-Smith NL, et al. Cognitive therapy for depression: a comparison of individual psychotherapy and bibliotherapy for depressed older adults. Behav Modif. 2004;28(2):297–318.
- Sun CF, Correll CU, Trestman RL, et al. Low availability, long wait times, and high geographic disparity of psychiatric outpatient care in the US. Gen Hosp Psychiatry. 2023;84:12–17.
- Adams SJ, Pitre NL. Who uses bibliotherapy and why? A survey from an underserviced area. Can J Psychiatry. 2000;45(7):645–649.
- Starker S. Do-it-yourself therapy: the prescription of self-help books by psychologists. Psychother Theory Res Pract Train. 1988;25(1):142–146.
- Jamison C, Scogin F. The outcome of cognitive bibliotherapy with depressed adults. J Consult Clin Psychol. 1995;63(4):644–650.
- National Center for Education Statistics. Data point: adult literacy in the United States. 2019. https://nces.ed.gov/pubs2019/2019179.pdf. Accessed 9 Jul 2024.
- Schapira MM, Swartz S, Ganschow PS, et al. Tailoring educational and behavioral interventions to level of health literacy: a systematic review. MDM Policy Pract. 2017;2(1):2381468317714474.
- Carstens A. Tailoring print materials to match literacy levels: a challenge for document designers and practitioners in adult literacy. Language Matters. 2004;35(2):459–484.
- Shanteau J, Harris RJ, VandenBos GR. Psychological and behavioral factors in organ donation. Psychiatr Serv. 1992;43(3):
211–219. - Cuijpers P. Bibliotherapy in unipolar depression: a meta-analysis. J Behav Ther Exp Psychiatry. 1997;28(2):139–147.
- Marrs RW. A meta-analysis of bibliotherapy studies. Am J Community Psychol. 1995;23(6):843–870.
- Olfson M, Marcus SC. National trends in outpatient psychotherapy. Am J Psychiatry. 2010;167(12):1456–1463.
- Gulia KK, Kumar VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. 2018;18(3):155–165.
- Morelli V. Fatigue and chronic fatigue in the elderly: definitions, diagnoses, and treatments. Clin Geriatr Med. 2011;27(4):673–686.
- Sultanoff SM. Integrating humor into psychotherapy: research, theory, and the necessary conditions for the presence of therapeutic humor in helping relationships. Humanist Psychol. 2013;41(4):388–399.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision. American Psychiatric Association Publishing; 2022.
- Kanai T, Takeuchi H, Furukawa TA, et al. Time to recurrence after recovery from major depressive episodes and its predictors. Psychol Med. 2003;33(5):839–845.
- First MB, Koh S, Adler D. How clinicians actually use the DSM: Psychiatric Times survey results. Psychiatric Times. 21 May 2015. Accessed 14 Aug 2024. https://www.psychiatrictimes.com/view/how-clinicians-actually-use-dsm-psychiatric-times-survey-results
- Myers JE. Bibliotherapy and DCT: co‐constructing the therapeutic metaphor. J Couns Dev. 1998;76(3):243–250.
- Cuijpers P, Karyotaki E, Eckshtain D, et al. Psychotherapy for depression across different age groups: a systematic review and meta-analysis. JAMA Psychiatry. 2020;77(7):
694–702. - Gregory RJ, Schwer Canning S, Lee TW, Wise JC. Cognitive bibliotherapy for depression: a meta-analysis. Prof Psychol Res Pract. 2004;35(3):275–280.
- Den Boer PCAM, Wiersma D, Van Den Bosch RJ. Why is self-help neglected in the treatment of emotional disorders? A meta-analysis. Psychol Med. 2004;34(6):959–971.
- Cuijpers P, Donker T, van Straten A, et al. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med. 2010;40(12):1943–1957.
- Yuan S, Zhou X, Zhang Y, et al. Comparative efficacy and acceptability of bibliotherapy for depression and anxiety disorders in children and adolescents: a meta-analysis of randomized clinical trials. Neuropsychiatr Dis Treat. 2018;14:353–365.
- Evans K, Tyrer P, Catalan J, et al. Manual-assisted cognitive-behaviour therapy (MACT): a randomized controlled trial of a brief intervention with bibliotherapy in the treatment of recurrent deliberate self-harm. Psychol Med. 1999;29(1):19–25.
- Gualano MR, Bert F, Martorana M, et al. The long-term effects of bibliotherapy in depression treatment: systematic review of randomized clinical trials. Clin Psychol Rev. 2017;58:49–58.
- Fanner D, Urquhart C. Bibliotherapy for mental health service users Part 1: a systematic review. Health Inf Libr J. 2008;25(4):237–252.
- Apodaca TR, Miller WR. A meta‐analysis of the effectiveness of bibliotherapy for alcohol problems. J Clin Psychol. 2003;59(3):289–304.
- Borges G, Bagge CL, Cherpitel CJ, et al. A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychol Med. 2017;47(5):949–957.
- Gonçalves WS, Gherman BR, Abdo CHN, et al. Prevalence of sexual dysfunction in depressive and persistent depressive disorders: a systematic review and meta-analysis. Int J Impot Res. 2023;35(4):340–349.
- van Lankveld JJDM. Bibliotherapy in the treatment of sexual dysfunctions: a meta-analysis. J Consult Clin Psychol. 1998;66(4):702–708.
- Lou Q, Liu S, Huo YR, et al. Comprehensive analysis of patient and caregiver predictors for caregiver burden, anxiety and depression in Alzheimer’s disease. J Clin Nurs. 2015;24(17–18):2668–2678.
- Lwi SJ, Ford BQ, Casey JJ, et al. Poor caregiver mental health predicts mortality of patients with neurodegenerative disease. Proc Natl Acad Sci U S A. 2017;114(28):7319–7324.
- Gottschalk LA. Bibliotherapy as an adjuvant in psychotherapy. Am J Psychiatry. 1948;104(10):632–637.
- Kvam S, Kleppe CL, Nordhus IH, Hovland A. Exercise as a treatment for depression: a meta-analysis. J Affect Disord. 2016;202:
67–86. - Josefsson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: meta-analysis and systematic review. Scand J Med Sci Sports. 2014;24(2):259–272.
- Nwebube C, Faulkner GE, Thaut MH, et al. Rhythmic auditory music stimulation increases task-distraction during exercise among cardiac rehabilitation patients: a secondary analysis of a randomized controlled trial. Psychol Sport Exerc. 2021;53:101868.
- Esteves KJ, Whitten E. Assisted reading with digital audiobooks for students with reading disabilities. Reading Horizons. 2011;51(1):
21–40. - Chang ACS, Millett S. Improving reading rates and comprehension through audio-assisted extensive reading for beginner learners. System. 2015;52:91–102.
- Nielsen KL, Hansen G, Stav JB. How the initial thinking period affects student argumentation during peer instruction: students’ experiences versus observations. Stud High Educ. 2016;41(1):124–138.
- Brown PC, Roediger III HL, McDaniel MA. Make It Stick: The Science of Successful Learning. Harvard University Press; 2014.
- Cornett CE, Cornett CF. Bibliotherapy: The Right Book at the Right Time. Phi Delta Kappa Educational Foundation; 1980.