 by Darlene M. Amado, BA; Darlene A. Beamon, BSE, MA; and David V. Sheehan, MD, MBA
by Darlene M. Amado, BA; Darlene A. Beamon, BSE, MA; and David V. Sheehan, MD, MBA
Mrs. Amado is with the University of South Florida College of Public Health and the University of South Florida College of Medicine, Tampa, Florida; Mrs. Beamon is with the Springfield Public School System, Springfield, Massachusetts; and Dr. Sheehan is Distinguished University Health Professor Emeritus at the University of South Florida College of Medicine, Tampa, Florida.
Innov Clin Neurosci. 2014;11(9–10):141–163
Funding: There was no funding for the development and writing of this article.
Financial Disclosures: Mrs. Amado and Mrs. Beamon are named consultants on the Pediatric versions of the Sheehan-Suicidality Tracking Scale (S-STS); and Dr. Sheehan is the author and copyright holder of the S-STS, the Sheehan-Suicidality Tracking Scale Clinically Meaningful Change Measure Version (S-STS CMCM), the Pediatric versions of the S-STS, the Sheehan Disability Scale (SDS), and the Suicidality Modifiers Scale, is a co-author of the Suicide Plan Tracking Scale (SPTS), and owns stock in Medical Outcomes Systems, which has computerized the S-STS
Key Words: Suicide, pediatric suicide, linguistic validation in children, pediatric validation, suicidality, suicide in children, pediatric suicide scale, suicide scale, suicide risk, suicide risk in children, adolescent suicide, S-STS
Abstract: Objective: The United States Food and Drug Administration meta-analysis of registration trials of antidepressants found that emergent suicidality under the age of 25 years increases with decreasing age. This led to boxed warnings for antidepressants and the recommendation for careful assessment and monitoring of suicidality in children and adolescents. To address this need, we describe the development of a pediatric suicidality assessment and tracking scale and a novel, empirically based approach to its age-appropriate linguistic validation. Method: Starting with the adult version of the Sheehan-Suicidality Tracking Scale, we collaborated with reading specialists who use the sight word lists of Dolch and Fry and the grade level vocabulary lists of Beck, Farr, and Strickland to adapt the adult version to each age group. Results: Our approach resulted in the development and documentation of a process for linguistically validating three age-appropriate pediatric versions of the Sheehan-Suicidality Tracking Scale from the adult version of the scale: one for 6- to 8-year-olds, a second for 9- to 12-year-olds, and a third for 13- to 17-year-olds. Conclusion: Further reliability and cognitive debriefing studies are needed in diverse demographic, ethnic, and cultural groups to make the pediatric versions of the Sheehan-Suicidality Tracking Scale more reliable, more generalizable, and more useful.
Introduction
The finding that treatment-emergent suicidality increases with decreasing age under 25 years in the United States Food and Drug Administration (FDA) meta-analysis of registration trials of antidepressants[1,2] led to boxed warnings for antidepressants and the recommendation for careful assessment and monitoring of suicidality in children and adolescents. The meta-analysis also focused international attention on the urgent need for the development of a proper assessment and monitoring tool to meet this need. While the FDA provided warning about suicidality risk in children and adolescents, it did not advise that antidepressants be avoided in children and adolescents. However, media attention and, at times, overreaction to this issue and medico-legal concerns by clinicians have led to a significant reduction in the prescription of antidepressants to children and adolescents and a related increase in deaths from suicide and self poisonings over that past decade.[3] The FDA did not anticipate or expect this unfortunate outcome, but did have a duty to detect and warn about safety concerns with medications. The FDA was judicious in not advising against prescribing antidepressants in pediatric populations, and their decision to strongly urge proper assessment and monitoring of suicidality in those individuals being treated for depression with psychiatric medications was the most prudent, near-term solution to manage this issue. The problem was that a simple, reproducible, age-appropriate, and linguistically validated scale for specifically assessing and monitoring suicidality in pediatric populations was not available at the time to address this need. In this article, we describe the development of a pediatric suicidality assessment and tracking scale and a novel approach to its age-appropriate linguistic validation.
Method
The most frequent approach to the development of psychiatric scales for the pediatric population is to consult child psychiatrists, child psychologists, and pediatricians who have experience in communicating with children in healthcare settings. In our early attempts to develop a pediatric suicidality assessment and tracking scale from the adult Sheehan-Suicidality Tracking Scale (S-STS),[4] we consulted such experts. In spite of much interesting input, each expert used his or her own unique clinical approach. We found that even among experts, these approaches were often conflicting, the results somewhat haphazard, and the processes used not reproducible and consistently methodical. We searched for an approach that would be methodical, reproducible, and consistent and that might have an empirical foundation. We convened an Education Advisory Committee. Its members included faculty in academic departments of education who specialized in elementary and high school education, child and adult psychiatrists, and elementary school teachers in both the public and private sector, who provided valuable input on a range of possible challenges and solutions.
The first author of this article (D.A.) proposed the solution that was finally adopted: use the empirically based system already in place and widely adopted by school systems throughout the United States, Canada, and the United Kingdom for linguistic validation of educational texts. The specialists who are currently charged with the oversight and practical implementation of this approach in the educational system are reading specialists. The empirical foundation for this system was first suggested and begun by Edward W. Dolch in 1936[5] and subsequently developed into a more organized system in his later publications.[6] He identified 220 words (Dolch’s Sight Word List), in three tiers, that children need to be able to instantly recognize by sight, by the end of the first grade, to master their reading skills in English.
In 1972 and in subsequent publications, particularly in 1999, Edward B. Fry expanded Dolch’s sight word lists to 1,000 words (Fry’s 1000 Instant Words).[7–9] Fry’s lists are broken down differently from Dolch’s lists. Fry’s lists are divided into groups of 25 words, based on frequency of use and difficulty. Even though Dolch and Fry approached their selections using a slightly different methodology, their selections overlap substantially and are largely in agreement. Fry found that 25 words make up 33 percent, 100 words make up 50 percent, and 300 words make up 65 percent of all words found in English language publications. Almost every sentence uses several of the first 300 words in the Fry list. The first 100 words are usually mastered by first grade, the second 100 words mastered by second grade, the third 100 mastered in third grade, and the remaining 700 words are mastered in fourth and fifth grades.
Zeno et al[10] further extended this system in 1995 to 154,000 words covering a more extensive graded vocabulary used in kindergarten through 12th grade and in college throughout the United States. In the largest systematic word frequency count ever conducted, Zeno et al[10] empirically investigated and identified the usual words mastered by each grade from kindergarten through college in the educational system. They developed dictionaries that assist in identifying when students most frequently encounter these words across all grades. Other similar dictionaries and systems are widely used by reading specialists in the educational system to ensure that all reading materials can be understood by children at each grade and age.[11] Based on recent research, other authors found that after children master the sight words they usually best learn the more difficult multisyllabic words encountered in children’s novels by decoding the polysyllabic words and learning the word in the context of a phrase. Other education specialists systematically organized these “vocabulary words” or phrases into graded lists. We used the method published by Beck et al[12] for “vocabulary words” in conjunction with the “sight words” in the Dolch 220 list and the Fry 1000 list. Unlike sight words, which are recognized on sight, vocabulary words are decoded. The gradation of these words and phrases in an age-appropriate manner reflects not only word recognition and comprehension, but also conceptual understanding. The solution to developing Pediatric versions of the S-STS was to start with the adult version of the scale and collaborate with reading specialists who use these empirically derived systems and related dictionaries to adapt the adult version to each age group.
With this in mind, we put together a committee of reading specialists chaired by the second author of this article (D.B.), and in collaboration we developed three pediatric versions of the S-STS. We refer to the linguistic validation process that we used as the Dolch-Fry-Beck, Farr, Strickland (D-F-BFS) system, in deference to those who pioneered this process for the United States educational system and whose lists and texts we used in this linguistic validation.
The Committee of Reading Specialists felt that making a unique pediatric version of the S-STS for each age and grade level was unnecessarily cumbersome. Considering both language mastery and cognitive development, they felt that the task could be very efficiently accomplished by making three versions: one for 6- to 8-year-olds, a second for 9- to 12-year-olds, and a third for 13- to 17-year-olds.
Results
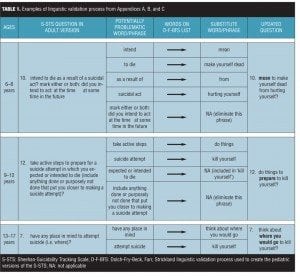
The approach described above resulted in Appendices A, B, and C (click here to access appendices), which document the alteration in each word or phrase from the adult version of the S-STS to its age appropriate substitute. Table 1 provides a few examples from these appendices to illustrate how this was done. In Table 1, the first column identifies the original wording in the adult version of the S-STS. Column 2 identifies a potentially problematic word or phrase. Column 3 notes that this word or phrase was consulted in the D-F-BFS lists for a suitable age-appropriate alternative. Column 4 identifies the substitute word for this word or phrase finally selected. Column 5 identifies the final wording of the question in age-appropriate language. The first block of rows illustrates the layout for the ages 6- to 8-year-old version, the second block of rows illustrates the layout for the ages 9- to 12-year-old version, and the third block of rows illustrates the layout for the ages 13- to 17-year-old version. The resultant three final pediatric versions of the S-STS are presented in Appendices D, E and F (click here to access appendices).
The Education Advisory Committee made a number of recommendations about the implementation of the pediatric scales:
1. The version for 6- to 8-year-olds should be clinician-rated and read orally to the child by the clinician. A parent should ideally be present during the interview, although in some circumstances at the discretion of the clinician this interview might need to be alone (e.g., when there is known child abuse by the parent or guardian or where the parent or guardian is not mentally competent to provide accurate information). Because 6- to 8-year-old children may not always be good reporters of their own behavior, it is preferable to have someone present with whom the child has a good relationship. The questions should be directed to the child. The parent or guardian should be asked at the start of the interview to avoid answering for the child unless the child provides information that appears to the parent to be erroneous. In situations when both parties give discrepant information, the clinician should discuss this with both parties and try to resolve the discrepancy in the interest of making an accurate assessment. While the child is the main focus of the questions in the interview, all relevant information from all reliable sources that can inform an accurate assessment of each suicidality item should be considered. Although this linguistic validation process is based on written language and simplifying the choice of words accordingly, we expect that most children in the 6- to 8-year-old group will understand the language and concepts even better when it is presented orally rather than in written form. In support of this statement, Beck et al state, “Young children’s listening and speaking competence is in advance of their reading and writing competence. That is, they can understand much more sophisticated content presented in oral language than they can read independently.”[13]
2. The version for 9- to 12-year-olds should be either clinician-rated or self-rated depending on the child’s reading and cognitive skills and the child’s relationship with the parent and the clinician. Usually this rating is best done with both the parent and clinician present, rather having the child self-rate alone. However, children with high IQs and at the upper end of this age range may prefer or feel more comfortable doing the self-rating. Cognitively delayed children in all age groups will obviously need more clinician assistance in completing the task. This decision is best made at the clinician’s discretion.
3. The version for 13- to 17-year-olds should be self-rated, since adolescents tend to be more self-conscious and less likely to involve parents and others in the their inner lives or in the interviews.
4. The 6- to 8-year-olds and some of the 9- to 12-year-olds may have difficulty properly understanding the spectrum of graded response options to the questions. This can complicate getting accurate information. Comprehension can be tested at the beginning of the interview. To manage this issue, it is acceptable to use a variety of adjunctive aids to visually illustrate the escalating and graded nature of the response options, like pictographs or increasing numbers of physical objects, like blocks or other manipulables as currently used in the elementary school system for this purpose. It is too early in the development stage of these pediatric versions of the S-STS to recommend any one manipulable or pictograph over another with confidence. Future research is needed to further explore the optimal choice of pictographs or manipulables to assess these graded responses. In general, most children have adequate discriminative ability and a logical capacity for cognitive operations by age 6.
Discussion
The system adopted for the development of the pediatric versions of the S-STS has been used by a small number of clinicians and other people involved with suicidal children. The feedback they provided has been useful in evolving the scale, and their experience with the pediatric S-STS scales has been positive. However, from these beginnings, a more extensive and formally structured cognitive debriefing process is needed to get feedback on the scale from children, adolescents, and those directly involved in working with the children and adolescents clinically. Cognitive debriefing is the process by which a scale is tested in a target population and target language group to determine whether the patients understand the concepts and items as the patient-reported outcome scale developers intended. Cognitive debriefing uses follow-up questions in field test interviews to better understand how patients interpret the scale questions and to collect all the concepts considered by each scale item. It is done to ensure that the validated instrument is contextually relevant and culturally acceptable to the target population. Linguistic validation into other languages and the cognitive debriefing process follows the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) recommended methodology (http://www.ispor.org/workpaper/practices_index.asp).
Sitting with and surveying parents and children within the age ranges of these clusters and discussing with them the choice and understanding of each question along the lines outlined by Wild et al[14] and by Henning and Pickett[15] will assist in adapting the current pediatric versions of the S-STS for different ethnic, cultural, and at-risk groups. Pediatric versions of the S-STS need to be tested in a broad range of demographic, socioeconomic, ethnic, and cultural settings and in those with various disabilities.
Since there is no gold standard pediatric suicidality scale that is linguistically validated, psychometric validation studies at this early stage may be premature and difficult to interpret. While there are other scales assessing different aspects of pediatric suicidality,[16] such as risk factors for suicidal ideation, psychometric validation needs to be done to compare scales that have some face equivalence and that have similar goals and focus. When linguistically validated pediatric suicidality scales with a similar focus and goals emerge, then psychometric validation studies need to be done. However, reliability studies can and should now be done to test the inter-rater reliability of clinician-rated versus clinician-rated, clinician-rated versus self-rated, and both clinician- and self-rated versions compared to a version that reconciles any differences between the two from the same interview (reconciliation version). Test-retest reliability studies can now be done on the current versions.
Much work remains to be done and will involve collaboration and feedback from a broad alliance of clinicians and researchers in many countries and cultures to continue to make the pediatric versions of S-STS more reliable, more generalizable, and more useful. Linguistic validation using the process described above with cognitive debriefing to develop pediatric suicidality scales from their psychometrically validated adult versions alone is not sufficient to address the needs of the field.
A similar linguistic validation process may not be possible in some languages where no similar linguistic validation analyses, dictionaries, and reading specialists are available. We understand that French, German, Spanish, and Japanese are among those languages where a similar process is possible based on similar existing empirical language analyses and reading specialists.
The use of empirically based, age-appropriate, linguistic validation of pediatric suicide scales is a necessary step in enhancing their accuracy and comprehension within a single language. The method discussed provides a model for such an approach. We hope this will start a process that may protect children and adolescents and reduce the tragic loss of life internationally from this silent and often preventable epidemic.
Acknowledgments
The authors wish to acknowledge the contribution of JM Giddens for editorial assistance in the preparation of the manuscript and related documents and for input into the development of all versions of the S-STS.
References
1. Stone M, Laughren T, Jones ML et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009 Aug 11;339:b2880.
2. Hammed T, Laughren T, Racoosin JA. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry. 2006;63:332–339.
3. Lu CY, Zhang F, Lakoma MD et al. Changes in antidepressant use by young people and suicidal behavior after FDA warnings and media coverage: quasi-experimental study. BMJ. 2014 Jun 18;348-g3596.
4. Sheehan DV, Giddens JM, Sheehan IS. Status Update on the Sheehan-Suicidality Tracking Scale (S-STS). Innov Clin Neurosci. 2014;11(9–10):93–140.
5. Dolch EW. A basic sight word vocabulary. Elementary School Journal. 1936;36:456–460.
6. Dolch EW. Problems in Reading. Champaign, IL: The Garrard Press; 1948.
7. Fry EB. Elementary Reading Instruction. New York. McGraw Hill; 1977.
8. Fry EB. 1000 Instant Words: The Most Common Words for Teaching Reading Writing and Spelling. Westminster, CA: Teacher Created Resources; 1999.
9. Fry EB, Kress JE. The Reading Teacher’s Book of Lists, Fifth Edition. San Francisco: Jossey-Bass; 2006.
10. Zeno SM, Ivens SH, Millard RT, et al. The Educator’s Word Frequency Guide. Brewster, NY: Touchstone Applied Science Associates; 1995.
11. Carroll JB, Davies P, Richman B. The American Heritage Word Frequency Book. New York: Houghton Mifflin; 1971.
12. Beck IL, Farr R, Strickland DS. Harcourt Trophies: A Harcourt Reading/Language Arts Program. Orlando, FL. Harcourt Inc.; 2003.
13. Beck IL, McKeown MG, Kucan L. Bringing Words to Light: Robust Vocabulary Instruction. New York: Guilford Press; 2002.
14. Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value in Health. 2005;8(2):94–104.
15. Henning D, Pickett A. A Study of Improving Sight and Functional Vocabulary Development and Comprehension. 65p. M.A. Research Project, Saint Xavier University and SkyLight Professional Development; 2000.
16. Winters NC, Myers K, Proud L. Ten-year review of rating scales. III: scales assessing suicidality, cognitive style, and self-esteem. J Am Acad Child Adolesc Psychiatry. 2002;41(10):1150–1181.