by Emily E. Leppien, PharmD, BCPS; Tammie Lee Demler, BS, PharmD, MBA, BCGP, BCPP; and Eileen Trigoboff, RN, PMHCNS-BC, DNS, DABFN
Dr. Leppien is with the Binghamton University School of Pharmacy and Pharmaceutical Sciences and Lourdes Hospital Center for Pain and Wellness in Binghamton, New York. Drs. Demler and Trigoboff are with the Buffalo Psychiatric Center, New York State Office of Mental Health, the University at Buffalo School of Pharmacy and Pharmaceutical Sciences (Department of Pharmacy Practice) and the University at Buffalo School of Medicine (Department of Psychiatry) in Buffalo, New York.
Funding: No funding was provided for this study.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Background: Antimicrobial resistance threatens the effective prevention and treatment of many types of infections. Infection occurs more frequently in patients diagnosed with psychiatric illness due to a number of risk factors. Urinary tract infections (UTI) are among the most common infections in this patient population. Currently, there is little information available offering guidance on how to treat infections commonly reported in patients with psychiatric illnesses, nor are there specific recommendations on how to provide efficient and effective educational interventions to prescribers who typically are not infectious disease specialists yet are responsible for treating infections within a psychiatric hospital. This study aims to determine 1) whether psychiatric inpatients were appropriately treated for a urinary tract infection (UTI) prior to educational interventions, and 2) whether there is a relationship between different modes of educational interventions and increased knowledge attainment and retention among healthcare clinicians regarding UTI treatment. This study also sought to determine if 3) health-team teaching used as an enablement method improves antibiotic prescribing and if 4) the number of appropriate UTI treatment regimens increased following educational intervention compared to baseline (prior to educational intervention). Methods: A 10-question pre-test survey focusing on UTIs was administered to clinicians in various healthcare disciplines who were later randomly assigned to receive UTI educational interventions either as a live lecture or independent study with identical content. The same 10-question survey was administered as a post-test, 6 to 7 weeks following the educational intervention. Antibiotic prescribing prior to and following educational interventions was assessed to note prescribing trends. Results: Analysis showed that healthcare providers who received live education scored higher on the post-test survey versus those who received directions for self-directed review of educational material presented at the live educational intervention (p<0.001). Following educational interventions, the number of urine samples collected for suspected UTI decreased, resulting in a decrease of unnecessary antibiotic treatment. The number of appropriately prescribed antibiotic treatment regimens increased following educational efforts. Conclusion: These enablement educational intervention strategies resulted in significantly improved antibiotic prescribing, indicating that andragogical teaching methods, reinforced through printed material and verbal communication of prescribing deficits, promotes knowledge retention and improved care for patients hospitalized with psychiatric illness.
Keywords: Psychiatric inpatients, antimicrobial stewardship, provider education, educational strategies, antibiotic prescribing, prescribing practices
Innov Clin Neurosci. 2019;16(5–6):22–29
The World Health Organization (WHO) estimates that healthcare-acquired infections affect 3.5 to 12 percent of all hospitalized patients.1 The United States (US) Centers for Disease Control and Prevention (CDC) reported that up to 50 percent of antibiotics prescribed for the treatment of healthcare-acquired infections within acute care hospitals in the US were either inappropriate or unnecessary.2 Patients unnecessarily exposed to antibiotics are placed at an increased risk of serious adverse events with no clinical benefit. Misuse of antibiotics has contributed to the growing problem of antibiotic resistance, which has threatened the effective prevention and treatment of infections.2
The CDC identified antimicrobial agents as one of the most commonly prescribed medications within nursing homes, with 70 percent of long-term care facility (LTCF) patients receiving at least one antibiotic prescription annually.3 The increased use of antibiotics, inappropriate treatment of infections, and increasing antimicrobial resistance indicates a need for more appropriate antimicrobial use within healthcare facilities. In response, the US Joint Commission announced a new medication management standard (MM.09.01.01) that requires all hospitals and LTCFs to implement an antimicrobial stewardship committee effective January 1, 2017.4 There has been debate over how the new Joint Commission standard applies to psychiatric hospitals. Compared to patients admitted to an acute care general medical hospital, patients with serious mental illness (SMI) tend to have significantly increased lengths of stay, making psychiatric hospitals more comparable to LTCFs than traditional acute care hospitals.
Urinary tract infections (UTIs) are one of the most common infections seen in patients with psychiatric illness, which suggests there might be increased antibiotic use in these settings.5–7 Acutely relapsed patients living with schizophrenia were 29 times more likely to have a UTI than stable outpatients.8 Psychiatric relapse can result in delusions and symptoms that hinder good hygiene and adequate hydration, which is thought to increase the risk of UTIs.8 Studies also show that patients experiencing psychiatric exacerbations have increased serum concentrations of interleukin (IL)-beta, IL-6, and c-reactive protein (CRP) compared to those free of psychiatric symptoms. It is unclear if this increased inflammation reduces the patient’s ability to fight the infection or is the result of an infection.9 Lastly, antipsychotics (APs) used to treat psychiatric illness can cause bladder and urinary complications, which might further contribute to the increased risk of UTIs among this patient population.10–12
Antimicrobial stewardship committees that assess prevention and treatment of infections within psychiatric hospitals and LCTFs are crucial. Establishing a consensus of appropriate UTI treatment in a psychiatric setting is challenging given that psychiatric inpatients residing in these facilities are more vulnerable to healthcare-associated infections due to environment and functional impairment. Within these facilities, prescribers responsible for treating infections commonly reported in psychiatric patients often are not infectious disease specialists. Knowledge gaps exist among clinicians despite the availability of evidence-based recommendations.13 Data from a prescriber survey revealed that while healthcare clinicians recognize the value of guideline adherence, a lack of familiarity with current treatment guidelines might contribute to dated prescribing practices.14
Kobayashi et al15 advocates that dated prescribing practices continue to exist for treatment of UTIs. For example, despite the recommendation from the Infectious Disease Society of America (IDSA), that fluoroquinolone only be used as a second-line treatment for UTI, use of this antibiotic as a first-line agent has not been curtailed. Data derived from National Ambulatory Medical Care surveys was analyzed to establish antibiotic prescribing trends for treatment of UTIs in the US. Treatment regimens for women 18 years of age or older with the diagnosis of uncomplicated UTI were included in the analysis. Fluoroquinolone was found to be the most frequently prescribed agent (49% of all antibiotic prescriptions). First-line agents trimethoprim/sulfamethoxazole (Bactrim) and nitrofurantoin (Macrobid) represented 27 and 19 percent of antibiotic prescriptions respectively. The study also revealed that patients 70 years of age or older (adjusted odds ratio [AOR]=2.5; 95 percent confidence interval [CI], 1.6–3.8) and patients treated by internists (AOR=2.0; 95% CI, 1.1–3.3) were more likely to be prescribed a fluoroquinolone for treatment of UTI.15 These findings demonstrate that prescribing practices of clinicians might deviate from current guideline recommendations with respect to treatment of UTIs. Educating prescribers on these discrepancies through educational interventions might prove useful in aligning clinical practice with evidence-based recommendations.
Stewardship standards outline the need to educate practitioners and direct patient-care staff on optimal prescribing to assist providers in adherence to guidelines.4 There is little data available that offer guidance on how to provide efficient and effective education to prescribers who are not infectious disease specialists but are responsible for treating infections within a psychiatric hospital. Continuing medical education (CME) programs are essential for closing knowledge gaps to improve prescribing practices by providing updates on treatment recommendations. The format of these learning programs, the platforms used for information delivery, and the type of assessment tools implemented to evaluate achievement of learning objectives can impact the effectiveness of CME programs. There is some evidence to suggest that the effectiveness of CME is greater when educational interventions use a mix of passive and active strategies, compared to traditional, didactic CME modalities.16 It is necessary to identify the characteristics that are most beneficial in conveying clinical messages to healthcare professionals and in promoting tangible changes to prescribing trends.
Objectives
This study aimed to determine 1) whether psychiatric inpatients were appropriately treated for UTIs prior to clinician educational interventions and 2) whether there was a relationship between different modes of educational interventions and increased knowledge attainment and retention among healthcare clinicians regarding UTI treatment. This study also sought to determine if 3) health-team teaching used as an enablement method improved antibiotic prescribing and if 4) the number of appropriate UTI treatment regimens increased following educational intervention compared to baseline (prior to educational intervention).
Methods
This study examined medication use evaluation (MUE) and subsequent performance improvement (PI) reports conducted by the Pharmacy and Therapeutics (P&T) Committee at a state psychiatric inpatient hospital, which was approved by the Institutional Review Board for the facility (New York State Psychiatric Institute). A chart review was conducted for patients hospitalized at the state psychiatric hospital anytime between January 1, 2017, and September 1, 2017, with at least one suspected UTI. Patient charts were evaluated for age, sex, UTI diagnosis, urinary tract symptoms, urinalysis results, urine culture and sensitivity results, and antibiotic treatment regimen, if any. This information was used to determine whether each patient was correctly diagnosed with a UTI or asymptomatic bacteriuria and whether antibiotic treatment was warranted. If an antibiotic treatment regimen was prescribed for UTI, the regimen was evaluated for appropriateness. An appropriate UTI regimen was defined as one where the organism was sensitive to the antibiotic prescribed, antibiotic dose was optimized (adjusted based on renal function and drug–drug interactions, if applicable), and total treatment duration was adequate per guideline recommendations.17 To determine whether the prescribed treatment regimen was effective, the need for subsequent antibiotic therapy following the initial UTI treatment course was assessed.
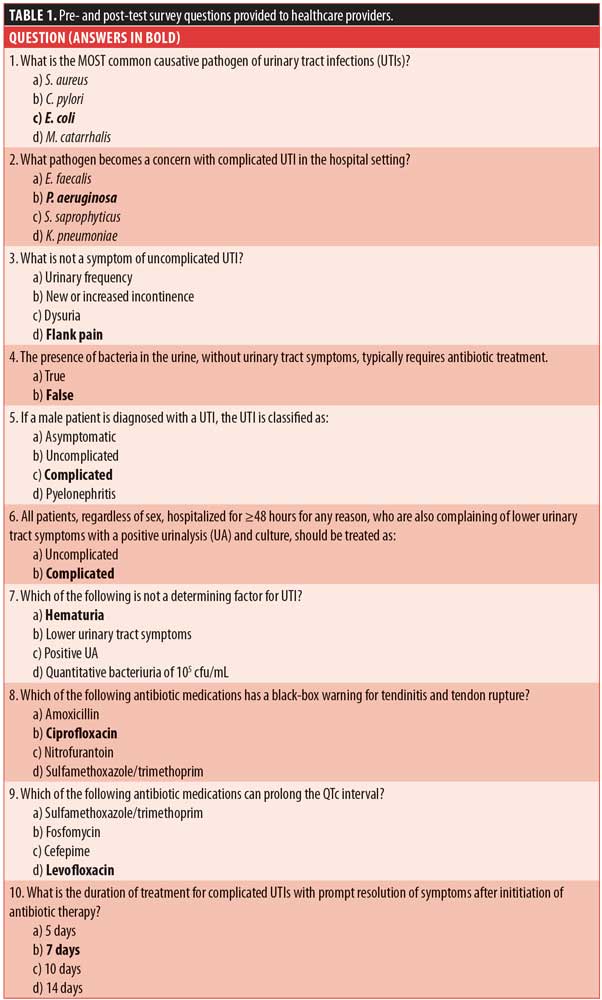
To determine the additional endpoints, an anonymous, identical 10-question multiple choice pre-test survey regarding symptoms, classification, diagnostic strategies, and treatment of UTIs was given to multidisciplinary healthcare clinicians (providers, pharmacists, and nurses) who were involved in the prescribing, dispensing, or administering of antibiotics to patients between June 1, 2017, and December 31, 2017. The survey questions are outlined in Table 1 (correct answers are bolded for purposes of this publication, but were not bolded when administered to healthcare clinicians).
After completion of the pre-test, healthcare clinicians were randomly assigned to receive UTI education either as a live lecture provided by a trained clinician or as independent study with identical content, highlighting key messages of UTI treatment as defined by the P&T committee based on current literature and guideline recommendations.17–22 The same 10-question survey was given as a post-test appropriately six weeks following educational interventions. Post-test results were evaluated using a two-tailed T-test to assess which educational intervention strategy, live or independent study, was more effective at increasing knowledge retention among healthcare clinicians overall and within different disciplines. T-test statistical analyses were conducted use the Statistical Package for Social Sciences version 23 (SPSS v23). The level for statistical significance was selected at p<0.05 to minimize the risk of Type I error.
Following education intervention strategies, a subsequent patient chart review was conducted for patients hospitalized between January 1, 2018, and June 30, 2018. Patient charts were again evaluated to determine whether each patient was correctly diagnosed with a UTI, whether antibiotic treatment was warranted, and if the treatment regimen prescribed was appropriate and effective, using the same criteria previously defined.
As part of a pharmacy PI report, pharmacists completed a screening evaluation of all antibiotic regimens prescribed from January 1, 2018, to June 30, 2018. The initial screening evaluation identified whether the antibiotic regimen indication was for UTI. All orders with an indication for UTI had an additional layer of review. Antibiotic drug, dose, and treatment duration were reviewed to ensure alignment with the key messages defined by the P&T committee. Pharmacists were directed to identify and communicate regimens not in alignment with these key messages to the P&T medical specialist for further review.
Inclusion criteria for Study Group 1.
- Male and female adult patients aged more than 18 years
- Inpatients at the state psychiatric hospital between either January 1, 2017, to September 1, 2017, or January 1, 2018 to June 30, 2018
- Charts containing documentation regarding UTI symptoms, urinalysis and/or culture and sensitivity results, if any, and an antibiotic prescription for the treatment of UTI from January 1, 2017, to September 1, 2017, and again from January 1, 2018, to June 30, 2018
Exclusion criteria for Study Group 1.
- Individuals with a criminal procedure law (CPL) designation
- Patients receiving antibiotic therapy for UTI prophylaxis
Inclusion criteria for Study Group 2.
- Any healthcare professional employed by the state psychiatric hospital between June 1, 2017, and December 31, 2017, and involved in the prescribing, dispensing, or administering of antibiotics to psychiatric inpatients
Exclusion criteria for Study Group 2.
- Nonhealthcare professionals
- Healthcare professionals not affiliated with the state psychiatric hospital
Results
UTI prescribing trends (from June 1, 2017, to September 1, 2017). There were 48 suspected cases of UTI among 37 patients between June 1, 2017, and September 1, 2017, as evidenced by obtainment of a urinalysis. Of the 48 suspected UTI cases, 15 (31%) cases were confirmed to have a UTI. These 15 cases occurred in 15 different patients. All 15 patients were candidates for antibiotic therapy. Of the 15 who were candidates for treatment, 13 (87%) received a course of antibiotics. Ten of the 13 (77%) patients who were treated with antibiotics received an appropriate treatment regimen (Figure 1). The remaining three (23%) patients did not receive an appropriate treatment regimen, in that it was too short of a treatment duration. One of the three (33%) patients who received an inappropriate treatment regimen required subsequent antibiotic therapy to eradicate the infection.
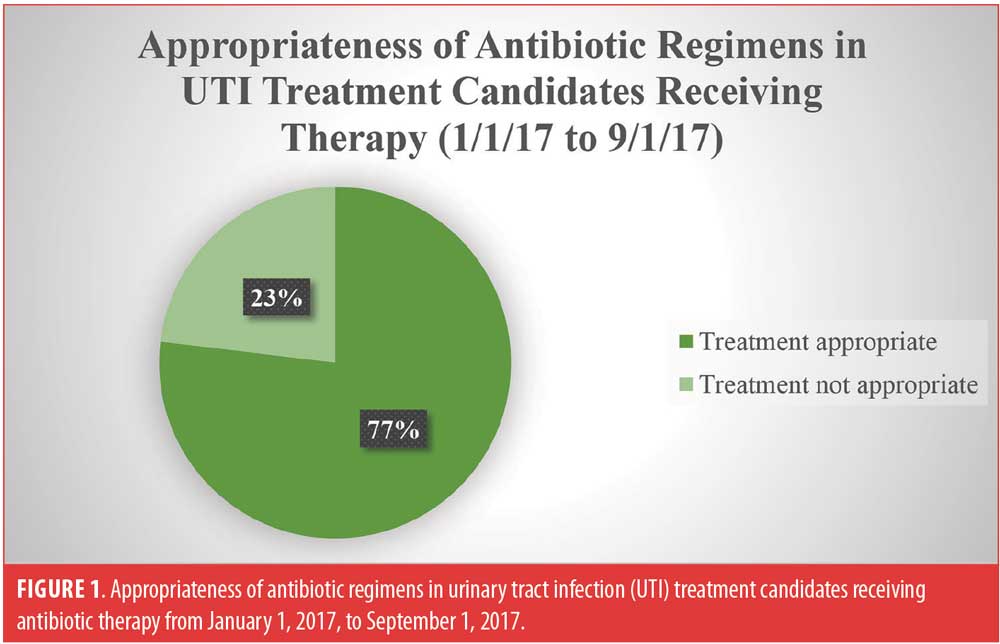
Of the 48 suspected UTI cases, 33 (69%) cases did not meet the criteria for UTI diagnosis. These 33 cases occurred among 22 different patients. Three (9%) patients received antibiotic therapy, which was deemed inappropriate per key messages defined by the P&T committee. These three patients were asymptomatic, indicating that antibiotic therapy should not have been prescribed, as asymptomatic bacteriuria in this patient population does not warrant antibiotic therapy.
Pre- and post-test survey. Table 2 summarizes the pre- and post-test survey administration dates and education intervention timeline. Survey questions and answer choices are listed in Table 1.

T-tests comparing the two educational intervention strategies were conducted on the entire training group and within each discipline. All resulted in a statistically significant difference between live andragogical interventions and independent review of educational materials, with the live training yielding a statistically significant higher level of learning as a result of training, compared to self-directed, independent review. The smallest difference, yet still significant, was noted with the prescriber group.
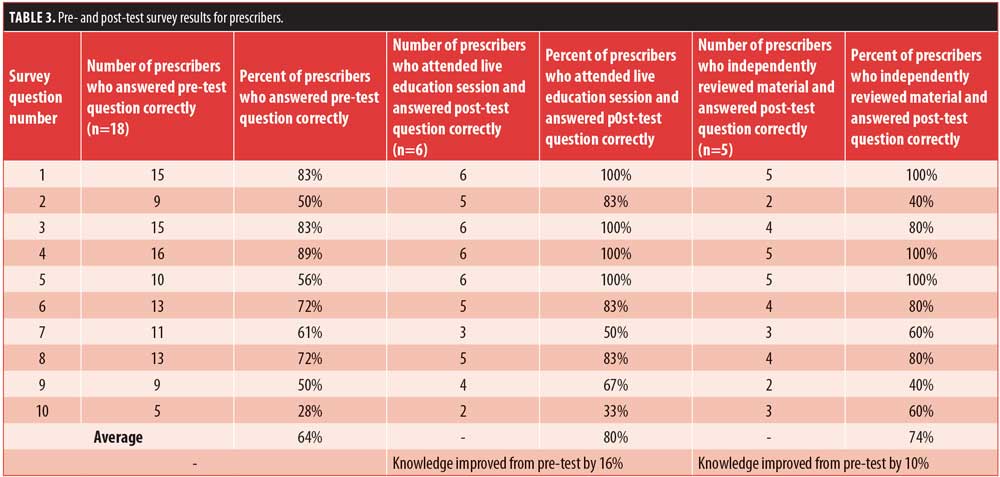
Eighteen prescribers were pre-tested. Nine prescribers were not pre-tested due to absence from the monthly medical staff organization (MSO) meeting or declination to participate in the survey. However, education was delivered to all prescribers. Fourteen prescribers attended the live education session and 13 received educational materials to independently review. Six of the 14 prescribers who received live education were post-tested, while 5 of the 13 prescribers who received educational materials to independently review were post-tested. Post-test scores for prescribers who received live educational training (t=10.854) were significantly higher (p=0.012) than those who independently reviewed educational materials (t=10.091). Table 3 displays survey results for prescribers.
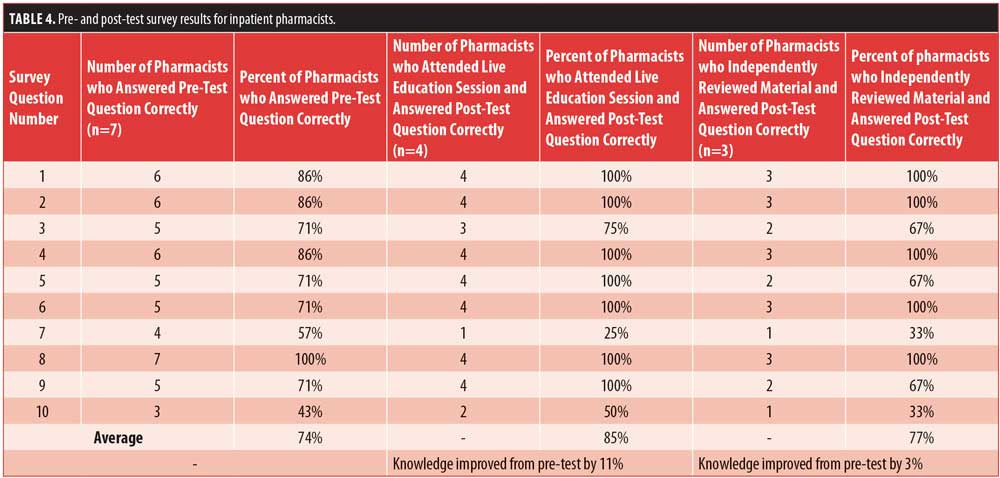
Seven pharmacists were pre-tested. Four pharmacists received live education and three received educational materials to independently review. All seven pharmacists were post-tested. Post-test scores for pharmacists who received live educational interventions (t=10.002) were significantly higher (p<0.001) than those who independently reviewed educational materials (t=8.835). Table 4 displays survey results for pharmacists.
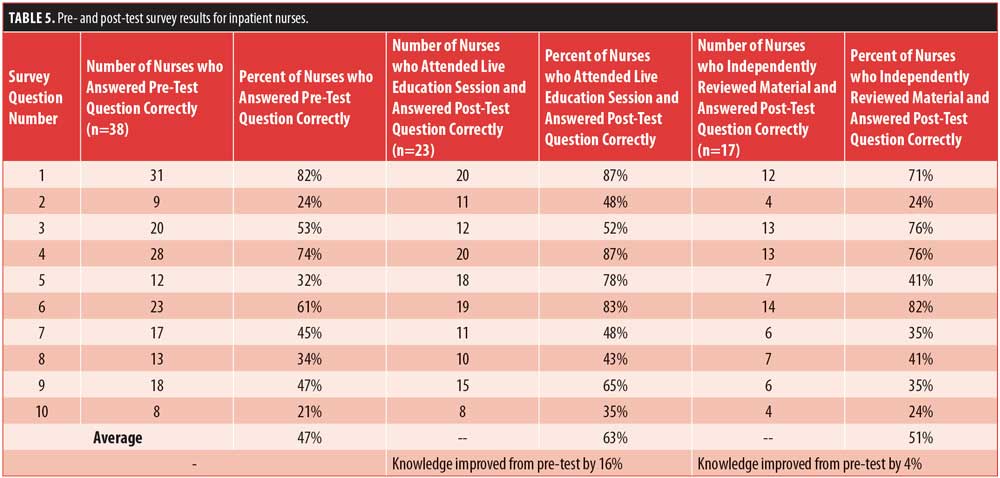
Thirty-eight inpatient nurses were pre-tested. Twenty-six inpatient nurses attended a live education session and 18 received educational materials to independently review. Twenty-three of the 26 nurses who received live education completed the post-test. However, 8 of the 18 nurses who were assigned to receive educational materials to independently review did not receive materials prior to the post-test, due to being inadvertently omitted from the email list-serve. Thus, their post-test results were excluded. Educational material was distributed to these eight nurses, and subsequent post-tests were rescheduled and analyzed separately. A total of 17 nurses who independently reviewed educational material during the first-wave of training were post-tested and included in the analysis. Post-test scores among inpatient nurses who received live educational interventions (t=10.006) were significantly higher (p<0.001) than those who independently reviewed educational materials (t=6.886). Table 5 displays survey results for inpatient nurses.
A total of 63 healthcare professionals were pre-tested and 58 professionals were post-tested, all of whom were included in the overall analysis. The post-test survey scores for all healthcare professionals improved from the baseline pre-test. Of the 58 post-tested professionals included in the analysis, 33 received live educational interventions, while 25 received educational materials to independently review. Post-test scores among all healthcare professionals who received live educational training (t=11.294) were significantly higher (p<0.001) than the post-test scores for those who independently reviewed educational materials (t=8.788).
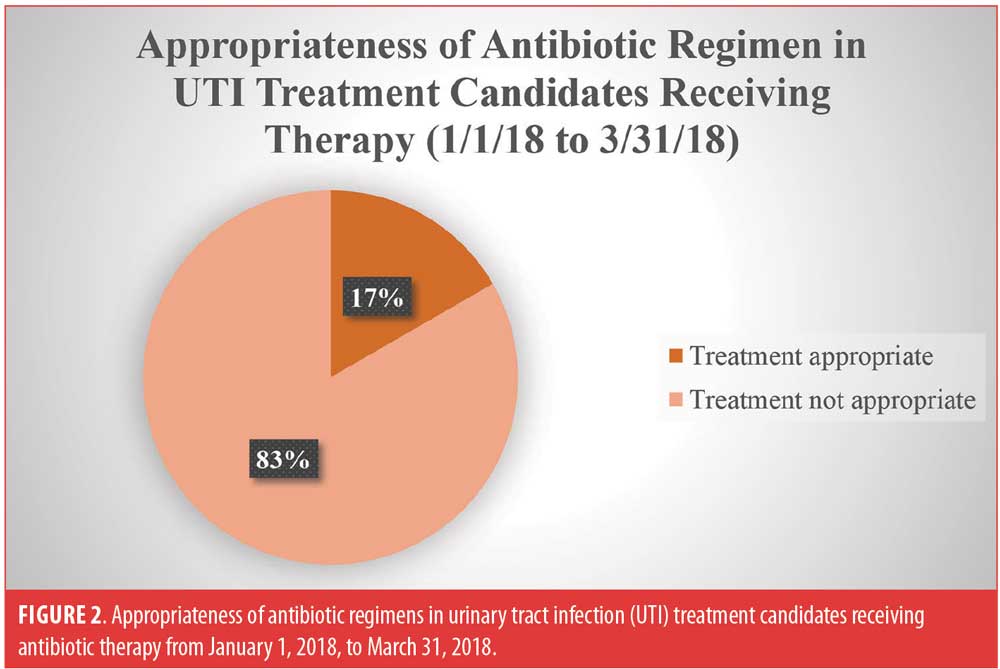
UTI prescribing trends (from January 1, 2018, to March 31, 2018). There were six suspected cases of UTI identified between January 1, 2018, and March 31, 2018, as evidenced by obtainment of urinalysis. These six cases occurred in six different patients. All six patients were candidates for antibiotic therapy and received a course of antibiotics. One (17%) of the 6 patients received an appropriate initial antibiotic regimen (Figure 2). One (17%) of the 6 patients was prescribed a contraindicated drug due to renal impairment, which was correctly identified by the pharmacist and changed to an appropriate regimen. The remaining four (30%) patients did not receive an appropriate antibiotic treatment regimen due to too short of treatment duration. Five (83%) patients did not receive an appropriate initial antibiotic regimen (Figure 2). Of the five patients who did not receive appropriate antibiotic therapy, one (20%) required a subsequent antibiotic treatment regimen to eradicate the infection.
UTI prescribing trends (from April 1, 2018, to June 30, 2018). There were five suspected cases of UTI identified between April 1, 2018, and June 30, 2018, as evidenced by obtainment of urinalysis. These five cases occurred in five different patients. All five patients were candidates for antibiotic therapy. All five (100%) patients received an appropriate initial antibiotic regimen (Figure 3).
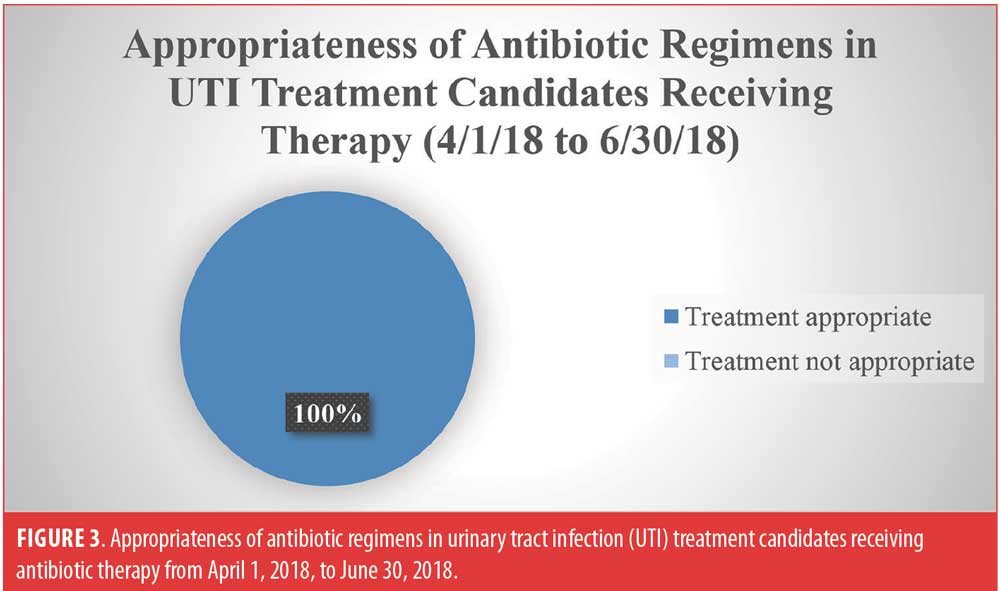
Performance improvement(from January 1, 2018, to June 30, 2018). Thirty-six total antibiotic regimens were prescribed during the first quarter from January 1, 2018, to March 31, 2018, with seven (19%) being prescribed for UTI. Forty-seven antibiotic regimens were prescribed during the second quarter from April 1, 2018, to June 30, 2018, with five (11%) being prescribed for UTI. Fewer antibiotic regimens for UTI were prescribed during the second quarter compared to the first quarter. During the first quarter, 1 of the 7 (14%) antibiotic regimens prescribed for treatment of UTI was deemed appropriate. Of these seven regimens, only two (29%) were correctly identified as not in alignment with key messages by the evaluating pharmacist. During the second quarter, all five (100%) antibiotic regimens prescribed for treatment of UTI were deemed appropriate. Of these five regimens, three (60%) were correctly identified as being in alignment with key messages by the evaluating pharmacist. Both prescribing and pharmacist assessment improved from the first to second quarter.
Discussion
Live education, compared to self-directed, independent review of the same educational material, is more effective at educating healthcare clinicians, as evidenced by post-test survey results. At face value, post-test scores improved from the baseline pre-test survey for all healthcare disciplines. Prescribers, pharmacists, and inpatient nurses who received live education retained more knowledge than those who independently reviewed educational material, which was the anticipated outcome. The eight inpatient nurses who did not initially receive educational material performed marginally better on the post-test survey compared to the 17 who received educational materials during the first wave of educational intervention, but this difference was not statistically significant. Confounding the results is that the eight nurses had seen the survey questions twice prior to reading educational material and taking subsequent post-test survey. All healthcare professionals overall and within each discipline had increased knowledge retention with live andragogical education training strategies compared to those who independently reviewed the same educational materials, and this improvement difference was found to be statistically significant.
Self-directed, independent review of educational materials might not have the same impact as live educational interventions presented by trained clinicians. This might be multifactorial, including limited time for healthcare professionals to read material, staffing constraints, and distractions during training. Andragogical educational methods are more applicable and preferred when educating adult professionals compared to pedagogical methods. Andragogical strategies allow healthcare professionals to discuss prior positive and negative experiences with other individuals within the healthcare field, increasing knowledge retention. Live educational interventions can be costly, which is why some institutions might elect not to implement andragogical teaching methods. However, the increased expense of live education would offset expenditure associated with increased medications, hospitalizations, and additional care.
It was suspected that educational interventions and survey questions would prompt healthcare providers to reevaluate the appropriateness of antibiotic treatment. Prescribers have been active in the recent clinical best practice of antimicrobial stewardship. This process in our facility engaged prescribers in examining treatment and outcomes for the most common infective process of UTIs. Therefore, their practice of keeping abreast of developments and clinical outcomes contributes to there being a still statistically significant difference between training modes, although it is less so given their routine patient care. Prescribers who independently reviewed educational material performed better on the post-test survey question regarding treatment duration (survey question 10) compared to those who received live education. A larger percentage of prescribers, regardless of educational intervention group, had a less robust improvement on this question (survey question 10) compared to other survey questions (survey questions 1–9). Analysis of UTI regimen appropriateness following educational intervention showed that this knowledge was not sustained as UTI regimen duration continued to be identified as the biggest prescribing deficit. Thus, we report that antibiotic stewardship and UTI treatment key messages presented through live andragogical educational methods was the most effective intervention in our state psychiatric hospital. We further recommend that live education be reinforced through printed material to promote knowledge retention.
There are no specific guidelines addressing treatment of UTI and other common infections within a psychiatric inpatient population. Due to the challenges associated with mental illness, psychiatric inpatients often have greater difficult communicating symptoms of urinary tract infections. When a psychiatric inpatient decompensates, or there is a change in mental status, healthcare clinicians are inclined to collect a urine sample for urinalysis and culture to rule out medical causes of psychiatric exacerbations. However, the increased collection of urine samples might result in unnecessary treatment of suspected UTI due to confusion over findings, as the presence of bacteria alone should not prompt treatment in all circumstances. Studies and case reports focused on psychiatric inpatients have found a trend of worsening psychosis with certain infections and with the medications used to treat these infections.23–28 Following educational interventions, the number of urine samples collected for suspected UTI decreased from 48 (January 1, 2017, to September 1, 2017) to 11 (June 1, 2018, to June 30, 2018). This reduced specimen collection coincided with a decreased rate of inappropriate antibiotic treatment from nine to zero percent.
There is also some debate on how psychiatric patients hospitalized at a long-term state psychiatric facility should be treated for confirmed UTI, which might have affected survey scores and UTI prescribing trends. It is unclear whether patients should be treated similarly to those in the community, LTCFs, or hospitals. However, recent literature is now classifying UTIs as healthcare-associated versus hospital-acquired because UTIs can be acquired in any healthcare setting (not just hospitals).18 Subsequently, the CDC published an article recommending that if a patient has been admitted to the LTCF for at least two days, the infection is to be classified as facility-associated.19 Society for Healthcare Epidemiology of America (SHEA) guidelines for treatment of UTI in LTCFs state that a seven-day course of treatment is recommended for all individuals who have symptoms of lower UTI and 10 to 14 days for those with upper UTI infections or fever.20,21 It is recommended that all men with UTI be treated with antibiotic therapy for 10 to 14 days.
A more recent article supports current literature defining complicated UTI as the following: pregnant women, urinary obstruction, comorbid conditions (i.e. uncontrolled diabetes), immunosuppression, renal failure, urinary retention from neurologic disease, or healthcare associated.22 Individuals meeting these criteria, which would include psychiatric inpatients residing in the state psychiatric facility, should be treated for 5 to 14 days. Current guidelines for complicated UTI recommend a seven-day antibiotic regimen for patients with symptoms of lower UTI and 10 to 14 days for patients with more severe symptoms, including fever.17 Again, men should always be treated for at least seven days. Given this evidence, the patients evaluated in this analysis with confirmed UTI should be treated according to complicated UTI guidelines, with at least five days of treatment for female patients and seven days of treatment for male patients.
Limitations of this study include small patient sample size from one facility and review of prescribing trends for only one specific infection (UTI). More studies are needed to review the overall impact team-based enablement interventions have on antibiotic prescribing trends within a psychiatric hospital.
Conclusion
All three disciplines included in this study work within a psychiatric specialty. This study would be useful in any specialty area or a general patient care setting for determining learning modes most effective for healthcare professionals. Our team-based enablement educational methods not only included targeted multidisciplinary education, but also involved PI initiatives that fostered continued commitment to focus on key messages and guideline adherence. Trained healthcare clinicians presenting educational content, and advocating for each team member to communicate survey key messages, resulted in decreased tendency to treat asymptomatic bacteriuria and increased appropriateness of prescribed UTI antibiotic treatment regimens. There is significant complexity of antibiotic use within psychiatric populations. UTI prescribing trends prior to educational interventions revealed that duration of treatment required the most attention. While the administered survey did not focus on appropriate drug selection, educational interventions did. Pharmacists evaluated drug selection as part of the PI and enablement methods; however, duration continued to be the biggest deficit. These enablement educational intervention strategies resulted in significantly improved prescriber antibiotic prescribing and pharmacist screening. We attribute this improvement to andragogical teaching methods, reinforced through printed material, and verbal communication of prescribing deficits, promoting knowledge retention for prescribers and improved care for those hospitalized with a psychiatric illness.
References
- WHO. Antimicrobial Resistance. (Updated: Apr 2015). https://www.who.int/gpsc/country_work/gpsc_ccisc_fact_sheet_en.pdf. Accessed October 27, 2017.
- United States Centers for Disease Control and Prevention. Core Elements of Hospital Antibiotic Stewardship Programs. (Updated: Feb 2017). https://www.cdc.gov/antibiotic-use/healthcare/implementation/core-elements.html. Accessed October 27, 2017.
- United States Centers for Disease Control and Prevention. Antibiotic Use in Nursing Homes. November 5, 2013. http://www.cdc.gov/getsmart/healthcare/learn-from-others/factsheets/nursing-homes.html. Accessed October 27, 2017.
- The United States Joint Commission. New Antimicrobial Stewardship Standard [Internet]. Joint Commission Perspectives. 2016;36(7):1–8.
- Demler TL, Mulcahy KB. Implications of infection and trends of antibiotic prescribing in hospitalized patients diagnosed with serious mental illness. Int Clin Psychopharmacol. 2018;33(1):49–55.
- Graham KL, Carson CM, Ezeoke A, et al. Urinary tract infections in acute psychosis. J Clin Psychiatry. 2014;75(4):379–385.
- Nicolle LE, Bentley D, Garibaldi R, et al. Antimicrobial use in long-term-care facilities. Infect Control Hosp Epidemiol. 2000;21(8):537–545.
- Miller BJ, Graham KL, Bodenheimer CM, et al. A prevalence study of urinary tract infections in acute relapse of schizophrenia. J Clin Psychiatry. 2013;74(3):271–277.
- Kirkpatrick B, Miller BJ. Inflammation and schizophrenia. Schizophr Bull. 2013;39(6):1174–1179.
- Hanes A, Demler T, Lee C, Campos A. Pseudoephedrine for the treatment of clozapine-induced incontinence. Innov Clin Neurosci. 2013;10(4):33–35.
- Warner JP, Harvey CA, Barnes TR. Clozapine and urinary incontinence. Int Clin Psychopharmacol. 1994;9(3):207–209.
- Thor KB, Donatucci C. Central nervous system control of the lower urinary tract: new pharmacological approaches to stress urinary incontinence in women. J Urol. 2004;172(1):27–33.
- Grindrod KA, Patel P, Martin JE. What interventions should pharmacists employ to impact health practitioners’ prescribing practices? Ann Pharmacother. 2006;40(9):1546–1557.
- Leppien E, Demler T. Examining prescriber perceptions of statin therapy and the potential implications these perceptions may have on guideline adherence. Int Clin Psychopharmacol. 2018;33(5):290–296.
- Kobayashi M, Shapiro DJ, Hersh AL, et al. Outpatient antibiotic prescribing practices for uncomplicated urinary tract infection in women in the United States, 2002–2011. Open forum infectious diseases. 2016 (Vol. 3, No. 3, p. ofw159). Oxford University Press.
- Mansouri M, Lockyer J. A meta-analysis of continuing medical education effectiveness. J Contin Educ Health Prof. 2007;27:6–15.
- Nicolle LE, AMMI Canada Guidelines Committee. Complicated urinary tract infection in adults. Can J Infect Dis Med Microbiol. 2005;16(6):349–360.
- Iacovelli V, Gaziev G, Topazio L, et al. Nosocomial urinary tract infections: a review. Urologia. 2014;81(4):222–227.
- United States Centers for Disease Control and Prevention. Urinary Tract Infection (UTI) Event for Long-term Care Facilities. (Updated Jan. 2018). https://www.cdc.gov/nhsn/PDFs/LTC/LTCF-UTI-protocol-current.pdf. Accessed April 2, 2018.
- Nicolle LE, SHEA Long-term-care-committee. Urinary tract infections in long-term-care facilities. Infect Control Hosp Epidemiol. 2001;22(3):167–175.
- Genao L, Buhr GT. Urinary tract infections in older adults residing in long-term care facilities. Ann Longterm Care. 2012;20(4):33–38.
- Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5):e103–120.
- Tosyali PM, Patel S, Varas DB, et al. Ceftriaxone and infection in first episode adolescent psychosis. J Child Adolesc Psychopharmacol. 2013;23(10):693–696.
- Seminog OO, Goldacre MJ. Risk of pneumonia and pneumococcal disease in people with severe mental illness: English record linkage studies. Thorax. 2013;68(2):171–176.
- Graham KL, Carson CM, Ezeoke A, et al. Urinary tract infections in acute psychosis. J Clin Psychiatry. 2014;75(4):379–385.
- Abouesh A, Stone C, Hobbs WR, et al. Antimicrobial-induced mania (antibiomania): a review of spontaneous reports. J Clin Psychopharmacol. 2002;22(1):71–81.
- Mostafa S, Miller BJ, et al. Antibiotic-associated psychosis during treatment of urinary tract infections: a systematic review. J Clin Psychopharmacol. 2014;34(4):483–490.
- Lurie I, Yang YX, Haynes K, et al. Antibiotic exposure and the risk for depression, anxiety, or psychosis: a nested case-control study. J Clin Psychiatry. 2015;76(11):1522–1528.





