by Randy A. Sansone, MD, and Lori A. Sansone, MD
by Randy A. Sansone, MD, and Lori A. Sansone, MD
R. Sansone is a professor in the Departments of Psychiatry and Internal Medicine at Wright State University School of Medicine in Dayton, OH, and Director of Psychiatry Education at Kettering Medical Center in Kettering, OH. L. Sansone is a civilian family medicine physician and Medical Director of the Family Health Clinic at Wright-Patterson Air Force Base Medical Center in WPAFB, OH. The views and opinions expressed in this article are those of the authors and do not reflect the official policy or position of the United States Air Force, Department of Defense, or United States Government.
Innov Clin Neurosci. 2013;10(11–12):23–27
This ongoing column is dedicated to the challenging clinical interface between psychiatry and primary care—two fields that are inexorably linked.
Funding: There was no funding for the development and writing of this article.
Financial Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: In medico-economic studies, wound care has been shown to be expensive but is seemingly unavoidable given an aging population and the high community rates of diabetes and obesity. Astonishingly, however, some impaired wound resolution is intentional or purposeful. According to our review of seven clinical samples, the prevalence of preventing wounds from healing varies from 0.8 percent in a cardiac-stress-testing sample to 13.3 percent in a psychiatric inpatient sample. These variations in prevalence suggest that the more psychiatric loading in a given population, the higher the potential rate of preventing wounds from healing. In addition, statistical analyses indicate that preventing wounds from healing is consistently associated with borderline personality disorder. This link is most likely explained through the psychodynamics of self-harm behavior. Self-harm behavior is an inherent feature of borderline personality disorder, and preventing wounds from healing may be a self-injury equivalent among some patients with this particular personality dysfunction. Among participants with this Axis II disorder, women tend to report higher rates of preventing wounds from healing than men. Overall findings suggest that clinicians need to be alert to unexpected delays with wound healing, particularly in patients with psychiatric histories, and consider that such behavior is likely to be associated with borderline personality disorder.
Key words: Borderline personality, healing, preventing wounds from healing, Self-Harm Inventory, wounds
Introduction
According to Sen et al,[1] approximately 6.5 million persons in the United States are affected by chronic wounds. As a result of this sizeable minority, an estimated 25 billion dollars is spent annually on the treatment of chronic wounds.[1] These expenditures are echoed in data projections from the United Kingdom, where Harding[2] estimates that the National Health Service will spend 2-3 billion pounds annually in direct costs for wound care. Likewise, Drew et al[3] estimate that the wound-care costs for a local British population of 500,000 for the years 2005–2006 would be between 15 and 18 million pounds. In a recent article on the topic of wound-care cost, Hjort et al[4] broached the uncomfortable finding that wound care will pose a major economic challenge for Denmark in the coming years.[4] These preceding findings indicate that chronic wound care is prevalent and expensive.
Perhaps some of these data are reasonably palatable based upon the medical origin and types of wound care typically referred to—e.g., pressure ulcers, venous stasis ulcers, neuropathic ulcers. As such, future increases in wound-care costs are understandably linked to the unfolding population dynamics of a disproportionately older population and the high prevalence rates of diabetes and obesity. However, what if some delays in wound healing were not due to medical causes? What if some lingering wounds were self-induced or intentional, and attributable to psychiatric illness?
In this edition of The Interface, we explore this intriguing possibility. We present data from a number of different clinical populations, all from our own studies, on the prevalence of purposefully preventing wounds from healing. We also review data statistically linking such behavior to borderline personality disorder. Among the various psychiatric disorders, one might wonder—why borderline personality disorder? This particular Axis II disorder is diagnostically characterized by self-harm behavior, and preventing wounds from healing may be an alternative form of such behavior. As a caveat, there may be other psychiatric disorders associated with preventing wounds from healing (e.g., psychotic disorders, obsessive-compulsive spectrum disorders), but we elected to focus on borderline personality disorder due to its relatively high prevalence in community populations (6%)[5] and in internal medicine outpatient settings (6.4%).[6]
The Prevalence of Preventing Wounds from Healing in Various Clinical Samples
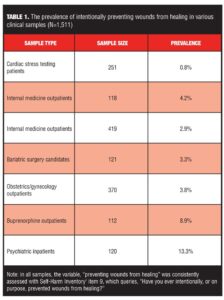
We have explored the prevalence of intentionally preventing wounds from healing in a number of different clinical samples. In the following review, we present these self-reported data beginning with medical samples and ending with psychiatric samples (Table 1). Each study in this review used the Self-Harm Inventory (SHI),[7] a 22-item self-report measure, for the assessment of preventing wounds from healing. Explicitly, item 9 of the SHI queries, “Have you ever intentionally, or on purpose, prevented wounds from healing?”
Cardiac stress testing patients. We examined the prevalence of preventing wounds from healing using the SHI in a consecutive sample of 251 patients undergoing cardiac stress testing in a suburban community-hospital setting.[8] In this sample of 118 men and 133 women, the average age was 58.0 years. Regarding ethnicity and education, 93.2 percent were White and only 7.6 percent of the sample did not finish high school. In this clinical population, the prevalence of preventing wounds from healing was 0.8 percent.
Internal medicine outpatients. We initially examined the prevalence of preventing wounds from healing using the SHI in a convenience sample of 118 internal medicine patients being seen for nonemergent medical care in a suburban outpatient clinic.[9] In this sample of 33 men and 85 women, we did not report the age demographics. Regarding ethnicity and education, 91.5 percent were White and 84.7 percent had attained at least a high school diploma. In this clinical population, 4.2 percent reported preventing wounds from healing.
In a second internal medicine outpatient sample of 419 consecutive patients, we examined the prevalence of preventing wounds from healing using the SHI.[10] In this sample of 130 men and 287 women, the average age was 49.5 years. Regarding ethnicity and education, 84.5 percent were White and 92.1 percent had at least graduated from high school. In this clinical population, 2.9 percent reported preventing wounds from healing.
Bariatric surgery candidates. We examined the prevalence of preventing wounds from healing using the SHI in a convenience sample of 121 bariatric surgery candidates at a suburban site.[11] In this sample of 104 women and 17 men, the average age was 44.6 years. Regarding ethnicity and education, 82.6 percent were White and 78 percent reported a high-school diploma as their highest degree of completed education. In this clinical population, the prevalence of preventing wounds from healing was 3.3 percent.
Obstetrics/gynecology outpatients. We examined the prevalence of preventing wounds from healing using the SHI in a consecutive sample of 370 women from an urban obstetrics/gynecology clinic.[12] In this sample, the average age of participants was 26.3 years. Regarding ethnicity and education, 54.3 percent were White and 39.4 percent were African-American; 88 percent reported high school as their highest level of educational attainment. On a side note, approximately 80 percent of the sample reported government insurance and 15.3 percent were self-pay or reported no-insurance. In this clinical population, the prevalence of preventing wounds from healing was 3.8 percent.
Buprenorphine patients. We examined the prevalence of preventing wounds from healing using the SHI in a convenience sample of 112 patients being treated at a subacute detoxification unit for opioid dependence.[13] In this setting, buprenorphine is the standardized treatment. In this sample of 60 men and 52 women, the average age was 32.9 years. Regarding ethnicity and education, most patients were White (92.0%) and 85.7 percent reported high school as their highest level of educational attainment. The prevalence of preventing wounds from healing in this clinical population was 8.9 percent.
Psychiatric inpatients. Finally, we examined the prevalence of preventing wounds from healing using the SHI in a convenience sample of 120 psychiatric inpatients in an urban hospital setting.[14] In this sample of 47 men and 73 women, the average age was 38.7 years. Regarding ethnicity, 81.5 percent of the participants were White and 15.1 percent were African-American. About two-thirds of the participants had completed high school and about one-third had completed some college coursework but not attained a degree. In this clinical population, the prevalence of preventing wounds from healing was 13.3 percent.
Summary. According to findings, preventing wounds from healing is least prevalent in medical specialty settings, prevalent at about 3 to 4 percent in various types of primary care populations, and most prevalent in psychiatric settings. We relate the buprenorphine sample to psychiatric samples due to the high rates of psychopathology encountered in those with substance abuse.
Caveats with these prevalence data. An important potential limitation in the preceding studies is the self-report format for the variable, “preventing wounds from healing.” It is likely that a number of participants in these various studies under-reported this specific behavior due to denial, suppression, repression, embarrassment, or misinterpretation (e.g., “it wasn’t really that”). Therefore, the reported prevalence rates in these studies may represent the proverbial “tip of the iceberg.”
Preventing Wounds from Healing: Relationships with Borderline Personality
In addition to examining the prevalence rates of preventing wounds from healing in various clinical samples, we have also previously examined relationships between preventing wounds from healing and borderline personality disorder. In all of the following studies, the assessment of borderline personality symptoms was accomplished using various self-report measures for this disorder, including the borderline personality scale of the Personality Diagnostic Questionnaire-R (PDQ-R),[15] the borderline personality scale of the Personality Diagnostic Questionnaire-4 (PDQ-4),[16] the SHI,[7][ and the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD).[17] As a caveat, personality disorder assessment with these types of self-report measures tends to be over-inclusive (i.e., generate false positives). Because of this, we will refer to our Axis II findings in this section in terms of borderline personality symptomatology (BPS) rather than disorder.
Internal medicine outpatients. In the more recent study of internal medicine outpatients that we previously presented, we also examined relationships between preventing wounds from healing and two self-report measures for BPS, the PDQ-4 and the SHI.[10] Given a prevalence rate of 2.9 percent, we compared respondents who admitted versus denied having prevented wounds from healing. Admitters had statistically significantly higher scores on both the PDQ-4 and the SHI, compared with deniers. In addition, compared with deniers, admitters were more likely to exceed the cut-off scores for BPS on both the PDQ-4 and SHI.
Obstetrics/gynecology outpatients. In the study of obstetrics/gynecology outpatients that we previously presented, we also examined the relationship between preventing wounds from healing and BPS using the PDQ-4.[12] In this study, the correlation between these variables was r=0.30. In addition, using a different statistical approach (chi square analysis), we found that preventing wounds from healing was statistically significantly higher among participants with BPS compared to those without this type of psychopathology.
Psychiatric inpatients and internal medicine outpatients. In a meta-analytic study, we examined 441 patients from one inpatient psychiatric site (4 different study samples) and 332 patients from one internal medicine outpatient site (6 different study samples) with regard to preventing wounds from healing.[18] In subsequent analyses, compared to psychiatric participants who did not exceed the cut-off score on the PDQ (i.e., either the PDQ-R or the PDQ-4), those with BPS were significantly more likely to endorse preventing wounds from healing. Likewise, compared to internal medicine participants who did not exceed the cut-off score on the PDQ, those with BPS were also significantly more likely to endorse preventing wounds from healing.
Gender patterns. In one study, in which we analyzed data from our previously cited internal medicine sample,[10] we examined gender patterns for preventing wounds from healing.[19] In this sample of 419 participants, reported rates for preventing wounds from healing among men and women were 5.6 percent and 12.2 percent, respectively. Although the rate among women was twice the rate encountered in men, this difference was not statistically significant.
Conclusion
Wound care is an expensive undertaking. Given that the majority of resistant wounds are legitimately secondary to medical causes, it is important to appreciate that some atypical or resistant wounds may be due to psychiatric dysfunction. According to the available data comprising 1,511 patients, the prevalence of preventing wounds from healing in seven clinical samples varied from 0.8 to 13.3 percent. In considering sampling characteristics, these data suggest that as the psychiatric loading of a given population increases, so do rates of preventing wounds from healing. According to three studies, one of which consisted of a meta-analysis, preventing wounds from healing is consistently related to BPS, regardless of the Axis-II measure for borderline personality or the statistical approach applied. The likely explanation for this association is that preventing wounds from healing is functioning as a self-injury equivalent—i.e., it is a behavioral variation of the characteristic self-harm behavior that one regularly encounters in individuals with BPS. Because of the preceding findings, clinicians need to be alert to unexpected delays in wound healing. The cause may not be so elusive and exotic, but rather well-known and familiar—borderline personality dynamics.
References
1. Sen CK, Gordillo GM, Roy S, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2009;17:763–771.
2. Harding K. Chronic wounds and their management and prevention is a significant public health issue. Int Wound J. 2010;7:125–126.
3. Drew P, Posnett J, Rusling L, et al. The cost of wound care for a local population in England. Int Wound J. 2007;4:149–155.
4. Hjort A, Gottrup F. Cost of wound treatment to increase significantly in Denmark over the next decade. J Wound Care. 2010;19:173–174, 176, 178, 180, 182, 184.
5. Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69:533–545.
6. Gross R, Olfson M, Gameroff M, et al. Borderline personality disorder in primary care. Arch Intern Med. 2002;162:53–60.
7. Sansone RA, Wiederman MW, Sansone LA. The Self-Harm Inventory (SHI): development of a scale for identifying self-destructive behaviors and borderline personality disorder. J Clin Psychol. 1998;54:973–983.
8. Sansone RA, Dittoe N, Hahn HS, Wiederman MW. The prevalence of self-harm behaviors in a consecutive sample of cardiac stress test patients. Int J Psychiatry Med. 2011;41:123–126.
9. Sansone RA, Wiederman MW, Sansone LA. Medically self-harming behavior and its relationship to borderline personality symptoms and somatic preoccupation among internal medicine patients. J Nerv Ment Dis. 2000;188:45–47.
10. Sansone RA, Lam C, Wiederman MW. Preventing wounds from healing: a relationship with borderline personality? Int J Psychiatry Med. 2010;40:469–471.
11. Sansone RA, Wiederman MW, Schumacher DF, Routsong-Weichers L. The prevalence of self-harm behaviors among a sample of gastric surgery candidates. J Psychosom Res. 2008;65:441–444.
12. Sansone RA, Chang J, Jewell B. Preventing wounds from healing and borderline personality symptomatology in an obstetrics/gynecology sample. Prim Care Companion. 2012;14(4). pii: PCC.11|01294. doi 10.4088/PCC.11|01294
13. Sansone RA, Whitecar P, Wiederman MW. Self-harm behaviors among buprenorphine-treated patients. Prim Care Companion. 2010;12:e1.
14. Sansone RA, McLean JS, Wiederman MW. The relationship between medically self-sabotaging behaviors and borderline personality disorder among psychiatric inpatients. Prim Care Companion. 2008;10:448–452.
15. Hyler SE, Skodol AE, Kellman HD, Oldham JM, Rosnick L. Validity of the Personality Diagnostic Questionnaire-Revised: comparison with two structured interviews. Am J Psychiatry. 1990;147:1043–1048.
16. Hyler SE. Personality Diagnostic Questionniare-4. New York: Author; 1994.
17. Zanarini MC, Vujanovic AA, Parachini EA, et al. A screening measure for BPD: the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD). J Pers Disord. 2003;17:568–ƒ573.
18. Sansone RA, Wiederman MW. Interference with wound healing: borderline patients in psychiatric versus medical settings. Prim Care Companion. 2009;11:271–272.
19. Sansone RA, Lam C, Wiederman MW. Self-harm behaviors in borderline personality. an analysis by gender. J Nerv Ment Dis. 2010;198:914–915.