 by Allison Cowan, MD; Racheal Johnson, DO; and Henrik Close, MD
by Allison Cowan, MD; Racheal Johnson, DO; and Henrik Close, MD
Dr. Cowan is with the Department of Psychiatry at the Boonshoft School of Medicine at Wright State University in Dayton, Ohio. Drs. Close and Johnson are with the Department of Psychiatry at the Boonshoft School of Medicine at Wright State University in Dayton, Ohio and are Captains in the United States Air Force.
FUNDING: No funding was provided.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Psychiatry is one of the first medical specialties to move to the practice of telehealth. Social distancing in the time of COVID-19 has prompted many face-to-face practices, including psychotherapy, to transition to virtual formats. Patients and physicians may have reservations about the change in approach and may have concerns about privacy and the security of protected health information. By utilizing telepsychiatry, patients and psychiatrists can have increased access to one another, bringing a host of benefits and challenges along with it. Addressing these concerns is an important part of telepsychiatry in psychotherapy practice. Here, we discuss practical solutions to challenges clinicians might encounter when moving a psychotherapy practice to telehealth, such as privacy issues, health information security, and developing/maintain a therapeutic bond.
Keywords: Coronavirus psychotherapy, telehealth, telepsychiatry for psychotherapy
Department editor. Julie P. Gentile, MD, is a professor with and chair of the Department of Psychiatry at Wright State University in Dayton, Ohio.
Editor’s Note. The patient cases presented in Psychotherapy Rounds are composite cases written to illustrate certain diagnostic characteristics and to instruct on treatment techniques. The composite cases are not real patients in treatment. Any resemblance to a real patient is purely coincidental.
Innov Clin Neurosci. 2020;17(4–6):23–26
Telehealth has been in use for decades. In 1959, the University of Nebraska Medical Center used two-way television to transmit demonstrations involving patients with neurological disorders to student doctors, and in 1961, group psychotherapy was conducted via two-way television.1 In the 1960s, the United States (US) Department of Veterans Affairs (VA) worked to expand mental health care through the use of videoconferencing and were able to demonstrate efficacy in decreasing admissions by an average of 24.4 percent with a 26.6-percent decrease of days of hospitalization as well.2 Telepsychiatry has been proven effective in increasing adherence3 and utilization has significantly increased since 2010.4 In addition to increasing access in rural areas,4 telepsychiatry use has also increased in US emergency departments, filling a critical need.5 The American Psychiatric Association (APA) suggests there are several patient populations, including those with severe anxiety disorders and geriatric patients with physical limitations, where telepsychiatry might be preferable to face-to-face treatment.6 This is likely also applicable to individuals with compromised immune systems and risk factors for a more severe course of disease during COVID 19. Morland et al7 demonstrated a similar reduction in problematic symptoms in a randomized, noninferiority trial of telemedicine compared with traditional in-person services delivery. A 2016 review of 452 studies of telepsychiatry outcomes reported that while both providers and patients are generally satisfied with telepsychiatry services, providers tend to be more concerned about the potential adverse effects of distance communication on therapeutic alliance.8 However, patients were less likely to endorse these concerns about their provider.8 Additionally, the review reported that when noninferiority designs were appropriately used, telepsychiatry performed as well as (if not better) than face-to-face services and was more cost-effective.8
Privacy Concerns
The COVID-19 pandemic has presented a host of new challenges to all healthcare providers, both in terms of physical measures taken to facilitate interactions safely and new methodological approaches. Fortunately, for psychiatrists in this crisis, psychotherapy does not necessitate physical interaction in the way traditional office medicine does and would ideally lend itself well to teletransition. Despite this apparent benefit, therapists transitioning away from traditional face-to-face practice to a telehealth interface still struggle with a multitude of concerns. Not only is the concept of introducing a technology intermediary into an otherwise sacred and highly personal relationship seemingly heresy, but the more practical concern regarding the Health Insurance Portability and Accountability Act of 1996 (HIPAA) adherence also arises.
Vignette 1. Dr. A is has been working with Mr. B, a 45-year-old engineer, for stress and anxiety at work. Dr. A is discussing the necessary move to telepsychiatry and his anxiety about the change. Dr. A anticipates that Mr. B will have significant reservations about this and has a handout ready for Mr. B from the US Department of Health and Human Services explaining temporary changes to HIPAA.9
Dr. A—Given the current safety risks, it looks like it would be best for us to move to telepsychiatry for the time being.
Mr. B—Yeah, sounds reasonable, but I’m worried about privacy. What if someone hacks us? Are you going to broadcast us? What options do I have?
Dr. A—Yes, I think it is reasonable to be concerned about this. I have this Health and Human Services information to give you. Tell me more about your worries.
Mr. B—OK, so we get just switch to online? Alright, but what if someone hears me or knows I’m in a session?
Dr. A—Those are good questions. When we first log in together, I’ll point my camera around my office so that you can see my door is closed. My job is to make sure your appointment is confidential on my end, and your job is to make sure it’s confidential on your end. Choose a location where you feel comfortable talking to me. Find a quiet room with a door that closes. Some people like to put on headphones. We will use a platform that meets healthcare privacy requirements, but the government has relaxed these during the time of COVID-19 so that people can still obtain medical care rather than go without.
Mr. B—I guess it’s not that different than when we meet in person. My wife knows when I have an appointment anyway. If we meet virtually it reduces my worries about exposing my family to coronavirus, and it also reduces your exposure. I want to make sure I’m not accidentally exposing you to coronavirus, too.
Dr. A—It’s also important to me to make sure I’m not getting my patients sick. And thank you for thinking of me.
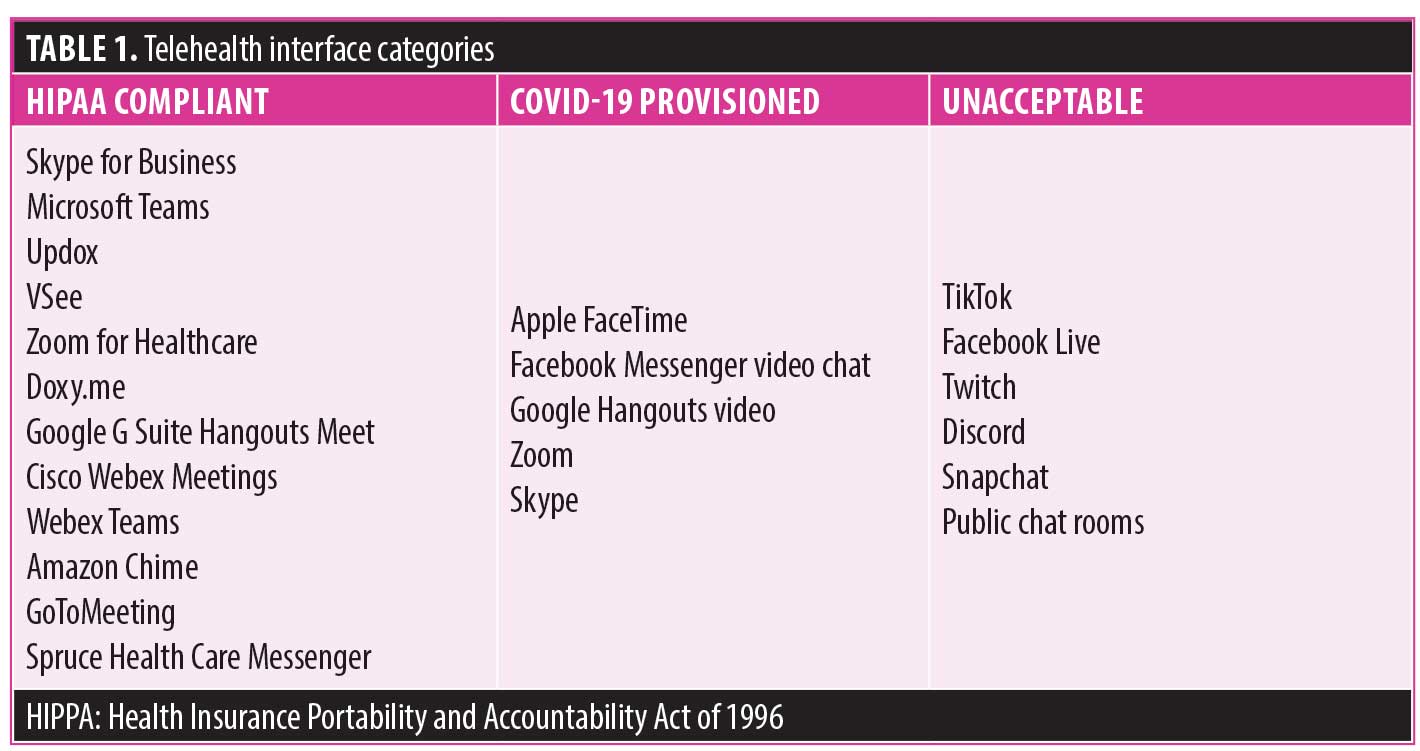
Dr. A discussed Mr. B’s real and reasonable privacy concerns. General guidance dictates that popular video applications that are “nonpublic facing” can be used for telehealth without concern for nonadherence with HIPAA during the COVID-19 pandemic. These are defined as nonpublic facing because they use end-to-end data encryption, thereby only allowing two individuals to share transmission. This is a distinct contrast with public-facing products that are designed to allow open, wide, and indiscriminate access to communications.10 Table 1 will clarify these interfaces.
Independent of choice of platform, more practical pointers should also be observed to protect patient privacy when using telehealth. These measures are particularly important in psychotherapy where many barriers already exist for a patient’s comfort and ability to be open and vulnerable. Telepsychiatry sessions should be conducted in private settings—generally office or clinic environments are best. Encourage your patient to be in a setting where he or she will not be overheard and will feel comfortable discussing therapy topics. Additionally, using lowered voices and discouraging use of speakerphone in addition to observing reasonable distance from others during appointments will further guard patient privacy. In general, informing the patient of the shared responsibility in the security of his or her appointment not only empowers the patient but also clarifies the importance of privacy in treatment.
Therapeutic Alliance in Telehealth
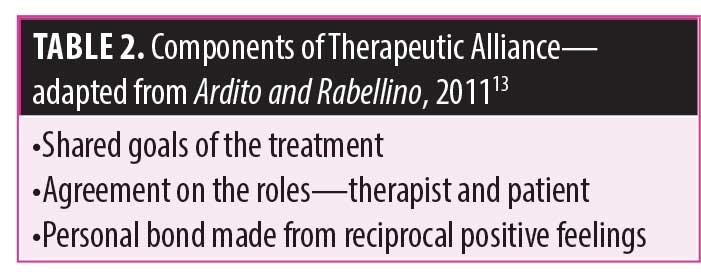
One of the concerns shared by patients and psychiatrists alike is how virtual appointments will affect the therapeutic alliance—the working relationship between the therapist and patient. Gabbard11 writes that “the alliance is present when the patient feels that the therapist is collaborating in pursuit of common therapeutic goals.” The therapeutic alliance is one of the proposed tools in psychotherapy that allows for change.12 The strength of the therapeutic alliance in telepsychiatry has been found to be equivalent to that of face-to-face visits.13 Discussing the relationship between the doctor and patient is encouraged and should be addressed when making the transition to telepsychiatry sessions (Table 2).
Vignette 2. Ms. C is a 32-year-old woman with a diagnosis of social anxiety disorder and has been seen for weekly psychodynamic psychotherapy with the goal of reducing her overall anxiety. She has been exploring how her fear of being judged has hindered her ability to form relationships. Due to COVID 19, her appointment has been transitioned to a telehealth appointment. This is the first virtual appointment.
Dr. A—It’s good to see you. This is different than what we are used to.
Ms. C—I know! I really wanted to see you because my anxiety has been really high since the quarantine.
Dr. A—Having increased anxiety during this time is completely understandable. Why don’t you tell me more about how you have been feeling?
Ms. C—I was worried that I would not be able to see you, that our appointment would be canceled. Just when I felt I was getting better, this had to happen, and now I can’t go out even if I wanted to. I feel like my progress has just been wiped away.
Dr. A—It is frustrating when we have worked so long toward getting out in the world to now be told you have to stay away from people.
Ms. C—It is frustrating. I mean, what is the point of continuing seeing each other? It just isn’t the same.
Dr. A—You’re right. This is not how we are used to seeing each other. Tell me more about your concerns.
Ms. C—What if I can’t log in? What if the camera doesn’t work? What if I get bored or distracted? You know I can shut down when I get nervous. What if that happens during our appointment?
Dr. A—OK, it seems like you have given this a lot of thought. Our work together is very important. If we have technical difficulties with the video equipment, we can always contact the information technology (IT) team or try to figure it out ourselves. Now that we are having our first session using the telepsychiatry platform, is it as difficult as you imagined?
Ms. C—No, it was actually pretty easy to log in. And our internet connection is OK.
Dr. A—Speaking of connection, how does it feel to interact in this way? Do you feel like something is missing?
Ms. C—Well, it is nice to see you. I feel better just after seeing you on my screen.
Dr. A—Most people using web-based services tend to forget about the camera and video after a little bit into the session.
Ms. C—You know, now that you mention it, I’d forgotten about it until we started talking about it.
Clinical pearls for enhancing therapeutic alliance in telepsychiatry.14
- Be more deliberate and overt in nonverbal responses such a purposefully exaggerating voice inflections and changes in tone as well as gestures and mannerisms
- Ask more questions to clarify
the meaning attached to patients’
facial expressions and body language
Dr. A opened the session by acknowledging the change of the setting. This modeled that it was OK to talk about the change in treatment modality. When Ms. C expressed frustration with the change, Dr. A validated her feelings. Rather than being defensive about the labor involved in implementing a telehealth platform, Dr. A was able to normalize having reservations and encouraged Ms. C to expand on her concerns. By taking a nonjudgmental approach and addressing concerns as they arose, the therapeutic alliance was preserved. Dr. A also empowered Ms. C to bring up any future concerns, strengthening the working relationship.
Other concerns often brought up regarding telehealth include how the home environment will alter the therapeutic relationship. For instance, a patient might worry how the psychiatrist would perceive their messy home. A doctor could worry that the patient will find them less credible if their background is not professional enough. A person’s home is often their inner sanctum, and much could be learned from what they choose to share via telehealth. The next vignette describes how the greater access to a person’s home environment via telehealth could be utilized to strengthen the therapeutic relationship.
Vignette 3. Mr. D is a 22-year-old man with a psychiatric diagnosis of major depressive disorder who has been seen monthly for combination medication management and supportive psychotherapy. There is a shortage of psychiatrists in his rural community and telehealth appointments have been key to his recovery. This is his seventh telepsychiatry appointment.
Mr. D—Hi, Dr. A. I am doing really well. I have more energy, and my appetite is back.
Dr. A—I am glad to hear you are feeling more like yourself. I know we increased your dosage of fluoxetine last appointment. Are you having any side effects to your medications?
Mr. D—Not that I know of. Haha, I may be eating too much now.
Dr. A—Let’s talk about that. What do you think is going on?
Mr. D—I think I am just feeling better overall. I am not eating too much, and I’ve started cooking for myself again. I’m excited about it, and I’m also so glad for these telehealth appointments. It has changed my life.
Dr. A—I am impressed with the hard work and effort you have put into feeling better. I see your dog, Shaggy, is there with you. Shaggy is getting bigger! Shaggy was a puppy when you rescued him. I remember how happy you were to get him for your birthday. And, oh my gosh, is that a tiny couch he is sitting on?
Mr. D—I knew you would notice that! Yes, I got Shaggy a tiny couch. I am thinking about making matching T-shirts for Shaggy and me. One with my face on it for him, and one with his face on it for me. Cool, huh?
Dr. A—That sounds pretty cool. Are you still taking daily walks with Shaggy to the park?
Mr. D—Yes. It has been good exercise for the two of us. I enjoy the sunshine and fresh air. Shaggy likes to run, so we get a good work out!
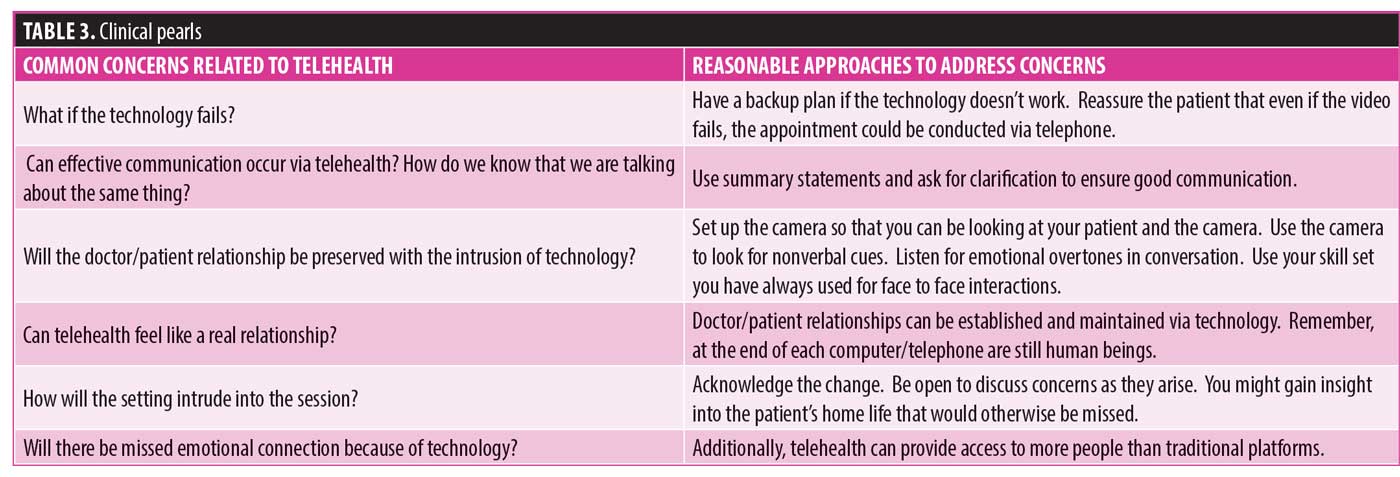
In this vignette, telehealth has provided access to treatment where limited resources and long travel times are otherwise prohibitive. Dr. A utilizes the home setting observed via telehealth to further strengthen the therapeutic alliance by acknowledging the changes in environment (i.e., Shaggy’s couch). She exaggerates some of her responses so that the affect carries over the telehealth connection more effectively. The ensuing conversation solidifies the therapeutic relationship further as Dr. A remembers important details surrounding the patient’s birthday, pet, and daily activities, thus demonstrating she hears and understands the patient. Dr. A encourages continued positive coping skills such as daily exercise to encourage continued improvement in Mr. D’s mental health. Telehealth can provide further insight into a patient’s private world and further strengthen the therapeutic relationship (Table 3).
Transference in Telepsychiatry and Psychotherapy
First described by Sigmund Freud, transference is widely understood to be the feelings, conscious, and unconscious, that a patient has toward their psychotherapist.15 Much like traditional face-to-face psychotherapy, there might be intrusions into the therapeutic space. Unlike construction noise in the building or parking lot angst, interruptions in teletherapy might take the shape of poor connections, a less desirable platform as another one the patient has used, or frustration about not being able to be together in person. These might also be seen as allusions to the transference, the idea that to broach a difficult topic such as irritation at the therapist, the patient might need to convey irritation in a more roundabout manner.
Mr. E is a 50-year-old man who initially presented for problems in his close relationships. He is seen by telepsychiatry.
Dr. A—Hi, Mr. E. How have you been since last appointment?
Mr. E—You know, of course this computer has to decide to install these updates now. It is just such a hassle to do things this way. I don’t even know if it’s worth it.
Dr. A—Oh, wow. It sounds like you’re pretty frustrated with it.
Mr. E—Of course I’m frustrated. I’m too old to be video chatting like a teenager. And I feel like you don’t want to actually have to see me.
Dr. A—Can you tell me more about that feeling—your words are saying you’re mad, but it looks like your face is saying that you are feeling sad.
Mr. E—What is it with you? Fine, I guess. I just feel like if you really wanted to see me, I could still come to the office.
Dr. A—It feels like I don’t care as much this way?
Mr. E—No, it’s not about the computer. It’s more that I wish you’d make an exception for me.
Dr. A—But I’m not making exceptions for anyone. Feeling that you’re being treated the same as everyone else can sometimes feel like getting less that what you’re due.
Mr. E—Yes, that’s it. I need to be the most important person. Ugh, even saying that out loud is a little embarrassing, but that’s how I feel. I know it’s not possible, but when you don’t do things special for me, it makes me feel like I’m not special at all.
Dr. A—I could see how that could get in the way here in our relationship, but also in your other relationships.
Dr. A focuses on the feelings behind the frustration with the technology. Of course, the technology might be the entirety of the issue but often there can be underlying feelings about the psychiatrist or the treatment. When Mr. E shares that he is embarrassed in talking by video but is able to share that he does not feel that he is valued, Dr. A can work through those feelings with him. This vignette demonstrates that while telehealth is a newer model of psychotherapy, there remain many similarities.
Conclusion
Telehealth has expanded exponentially in recent years and has increased even further with COVID-19. Telepsychiatry is a cost-effective and efficacious method in which to provide mental health services where distance and safety are barriers to traditional face-to-face care. While psychotherapy might appear different, there are many similarities, including worries about privacy and protected health information and transference processes. There are technological challenges, but the increased access into a patient’s space can be used to strengthen the therapeutic alliance. Telepsychiatry has a history longer than most would expect and is uniquely suited to bring psychiatric services to people in difficult times and austere locations.
References
- Wittson CL, Benschoter R. Two-way television: helping the medical center reach out. Am J Psychiatry. 1972;129(5):624–7.
- Godleski L, Darkins A, Peters J. Outcomes of 98,609 US Department of Veterans Affairs patients enrolled in telemental health services, 2006–2010. Psychiatr Serv. 2012;63(4):383–385.
- Shulman M, John M, Kane JM. Home-based outpatient telepsychiatry to improve adherence with treatment appointments: a pilot study. Psychiatr Serv. 2017;68(7):743–746.
- Spivak S, Spivak A, Cullen B, et al. Telepsychiatry use in US mental health facilities, 2010–2017. Psychiatr Serv. 2020;71(2):121–127.
- Freeman RE, Boggs KM, Zachrison KS, et al. National study of telepsychiatry use in US emergency departments. Psychiatr Serv. 2020 Feb:appi-ps.
- Hilty D. Evidence base in telepsychiatry. 2020. American Psychiatric Association site. https://www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/evidence-base. Accessed May 14, 2020.
- Morland LA, Greene CJ, Rosen CS, et al. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial. J Clin Psychiatry. 2010;71(7):855–863.
- Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016 Jun;6(2):269.
- USHHS Office of Civil Rights. 30 March 2020. Notification of enforcement discretion for telehealth remote communications during the COVID-19 Nationwide Public Health emergency. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. Accessed April 19, 2020.
- USHHS Office of Civil Rights site. FAQs on telehealth and HIPAA during the COVID-19 Nationwide Public Health emergency. 16 Apr 2020. https://www.hhs.gov/sites/default/files/telehealth-faqs-508.pdf. Accessed April 19, 2020.
- Gabbard GO. Long-term psychodynamic psychotherapy: a basic text. American Psychiatric Pub; 2017 Feb.
- Cabaniss DL. Psychodynamic Psychotherapy: a clinical manual. John Wiley & Sons; 2016:84.
- Ardito RB, Rabellino D. Therapeutic alliance and outcome of psychotherapy: historical excursus, measurements, and prospects for research. Front Psychol. 2011;2:270.
- Simpson SG, Reid CL. Therapeutic alliance in videoconferencing psychotherapy: A review. Aust J Rural Health. 2014;22(6):280–299.
- Freud S. Introductory lectures on psychoanalysis. WW Norton & Company; 1977.





