 by Takahiko Nagamine, MD, PhD
by Takahiko Nagamine, MD, PhD
Department of Psychiatric Internal Medicine, Sunlight Brain Research Center, Yamaguchi, Japan.
Innov Clin Neurosci. 2016;13(11–12):28–31.
Funding: No funding was received for the preparation of this article.
Financial disclosures: The author has no conflicts of interest relevant to the content of this article.
Key words: Cardiac arrest, hypothermia, risperidone, J-wave
Abstract: Hypothermia is a rare adverse effect of risperidone and is associated with ventricular arrhythmias, which may lead to intensive care unit admission and sometimes death. We describe a patient with schizophrenia who was taking risperidone and who, after falling into a hypothermic state, suffered cardiac arrest. Observations of the case and a brief literature review are provided.
Introduction
Hypothermia has high mortality and is associated with ventricular arrhythmias.[1] Antipsychotic drugs can influence thermoregulation.[2] We report the case of a 75-year-old patient with schizophrenia who suffered cardiac arrest due to severe hypothermia that we believe was induced by risperidone.
Case Presentation
A 75-year-old woman was found comatose in her house by her daughter. An ambulance service was called, and she was transferred to our emergency room (ER). She had been diagnosed with schizophrenia in her late teens. The corroborative history from her family members revealed that her treatment adherence was generally poor, resulting in relapses. However, in between the relapse episodes she functioned relatively well. Her medication history revealed that she had been well stabilized with risperidone. Three weeks before she presented to the ER, she had recommenced 6mg daily of risperidone for agitated behavior. She did not have any significant medical or psychoactive substance use history.
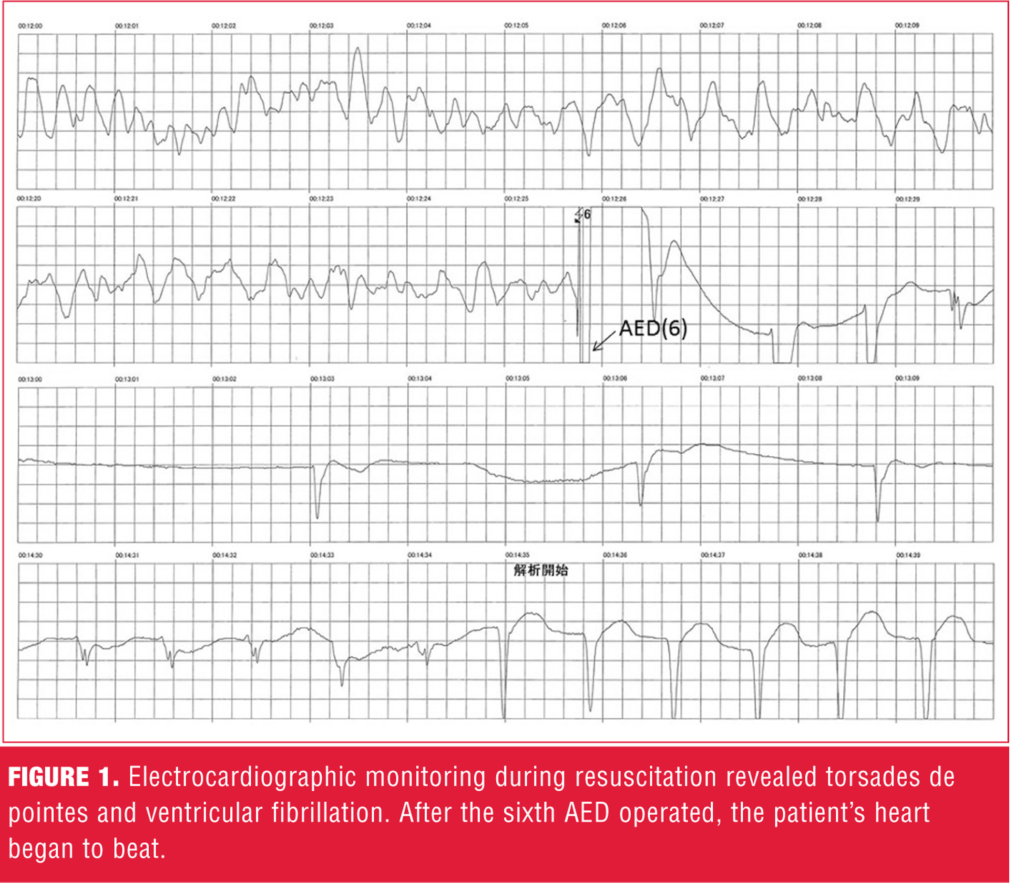
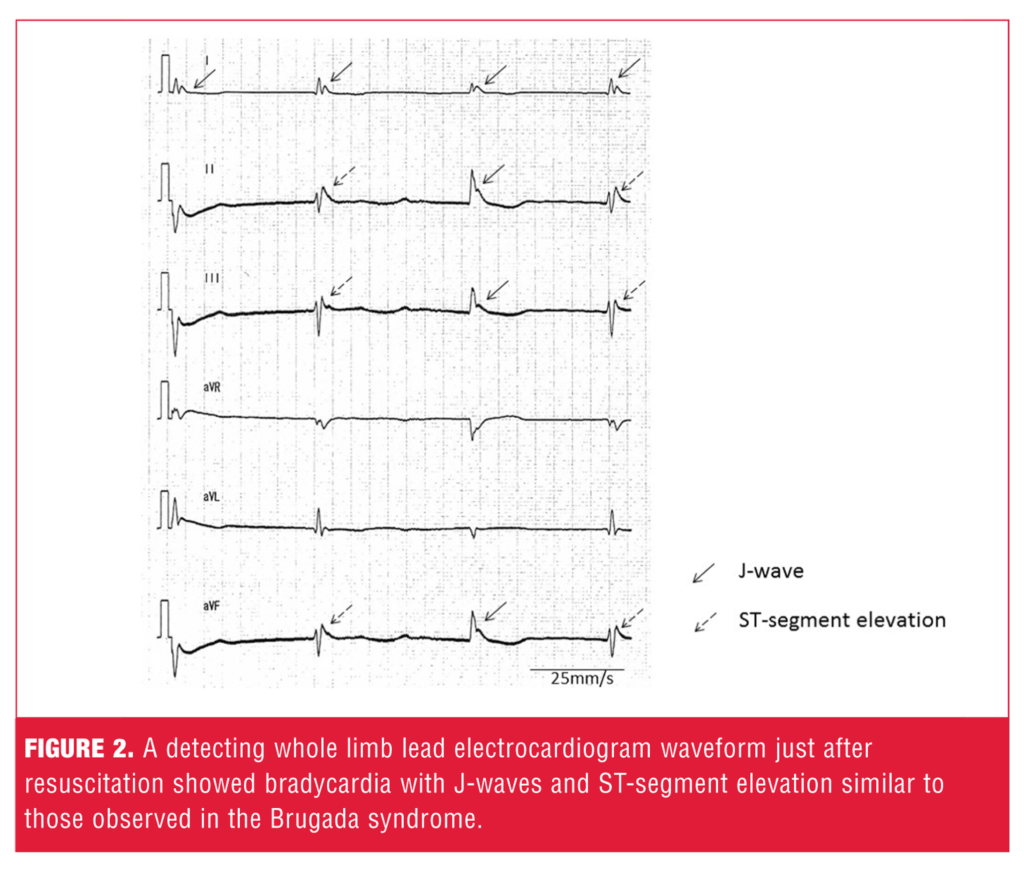
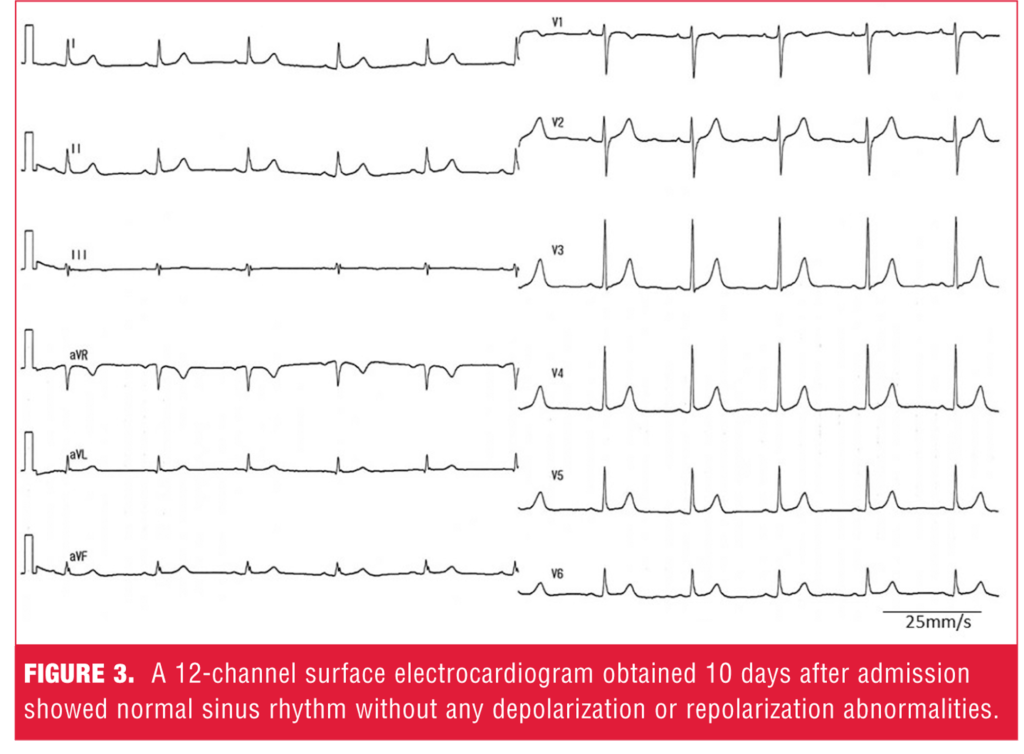
On arrival to the ER, she was not breathing and became pulseless; cardiopulmonary life support was started immediately. Emergency endotracheal intubation was performed, and chest compressions were provided at a rate of 100 compressions per minute to a depth of 4- to 5cm with full chest recoil between compressions. Along with conventional administration of adrenaline (total dose 2mg), an automated external defibrillator (AED) was performed. After the sixth AED operated, the patient’s heart began to beat (Figure 1). Return of spontaneous circulation and breathing occurred about 30 minutes after the patient’s arrival to the ER. The electrocardiogram (ECG) waveform performed just after resuscitation showed bradycardia with J-waves and ST-segment elevation similar to those observed in Brugada syndrome (Figure 2). These changes are characteristic of hypothermia.[3] Her core body temperature was measured at 32.2°C (89.96°F). She was closely monitored and warmed with blankets. Her hypothermia improved, and her temperature rose to 35.5°C (95.9°F). After warming to a normal body temperature, the patient recovered without any major complications. Her psychotic symptoms were successfully treated with aripiprazole 9mg daily without hypothermia. A 12-channel ECG obtained 10 days after admission showed normal sinus rhythm without any depolarization or repolarization abnormalities (Figure 3).
Discussion
Use of antipsychotic drugs is associated with an increased risk of ventricular fibrillation, cardiac arrest, QT-interval prolongation (a presumed marker of cardiac risk), and torsade de pointes.[4–8] In a case-crossover study in Taiwan, antipsychotic drug use was associated with a 1.53-fold higher risk of ventricular arrhythmia.4 According to a meta-analysis,[5] antipsychotics differ substantially in side effects, and small but robust differences are seen in efficacy. The risk of QT-interval prolongation was found to be significantly higher in ziprasidone, olanzapine, and risperidone than placebo and aripiprazole.[5] Risperidone, a widely used second-generation antipsychotic drug, in particular raises the risk of serious ventricular tachyarrhythmias, ventricular fibrillation, and sudden cardiac death.[6] A dose-dependent increase in risk of sudden cardiac death from risperidone has also been reported.[6] Blockade of the human cardiac potassium channel known as human ether-a-go-go-related gene (HERG) often underlies such clinical findings.[7] Antipsychotics with a high potency of the HERG blockade, such as risperidone and its active metabolite paliperidone, increase the risk of ventricular fibrillation.[4,8]
A rather rare and less documented adverse effect of risperidone is hypothermia, which is traditionally defined as a drop in core body temperature below 35.0°C (95.0?F).[2] Although the exact mechanisms of risperidone-induced hypothermia are unknown, several possible causes are speculated. Antipsychotic drugs with strong serotonin (5-HT2A) antagonism seem to be more frequently associated with hypothermia due to the association of the 5-HT2A receptor with thermoregulation.[9] Risperidone has a stronger affinity for the 5-HT2A receptor than for the dopamine D2 receptor, thus increasing the risk for hypothermia. In addition, risperidone blocks alpha2-adrenergic receptors, also involved in thermoregulation, by inducing peripheral responses to cooling (e.g., vasoconstriction, shivering), further increasing the risk for hypothermia.
Severe hypothermia has been well described as being associated with bradycardia, prolongation of the PQ and QT intervals, progressive widening of the QRS complex with J-wave, and increased incidence of ventricular fibrillation.[3] Brugada-like ECG changes have been described in patients with severe hypothermia.[10] The appearance of the Brugada-like ECG pattern during hypothermia may provide evidence for a common underlying cellular arrhythmogenic mechanism, such as an increase of the transmural voltage gradient. We observed J-waves in the ECG of our patient at the time of successful resuscitation, which led us to speculate that our patient suffered cardiac arrest due to severe hypothermia.
In clinical practice, certain medical conditions, such as diabetes, thyroid conditions, some medications, severe trauma, and substance abuse can increase the risk of hypothermia.[11] However, the most common cause of hypothermia is prolonged exposure to cold temperatures.[1] Our patient had no such medical history and was living in a house with an appropriate temperature, according to her daughter who cared for her. Thus we deduced that the hypothermia was caused by risperidone.
Though not directly related to the main point of this case report, we feel it is important to note that continuous chest compressions were vital to the successful and uncomplicated resuscitation of our patient. Uninterrupted chest compressions to patients in cardiac arrest provide perfusion and oxygenation to the tissues, including brain. Though psychiatrists and other mental health professionals are not likely to treat patients in cardiac arrest, nonetheless (should the need ever arise), it is a worthy reminder to them that interruptions in chest compressions during resuscitation, including pulse determinations, cardiac rhythm analysis, airway management, and vascular access, can negatively impact outcomes in cardiac arrest.[12] An innovative resuscitation protocol called cardiocerebral resuscitation emphasizes uninterrupted chest compressions.[13] Cardiac activity in our patient was successfully recovered by an emergency endotracheal intubation, repeated defibrillations by AED, and continuous chest compressions.
Conclusion
Our patient presented to the ER in a state of cardiac arrest. We were able to successfully resuscitate her without complication. Based on her very low body temperature and the presence of J-waves on her ECG, we speculated that hypothermia was the cause of the cardiac arrest. The patient did not have any medical conditions known to cause hypothermia nor had she been subjected to unusually cold temperatures; however, she was taking risperidone, an antipsychotic known to cause hypothermia. Thus, we deduced that our patient’s hypothermia was caused by risperidone. After being stabilized, our patient was switched to aripiprazole without further cardiac incidents.
Hypothermia is a rare but potentially life-threatening adverse effect of risperidone. Because risperidone is widely used in psychiatric settings, clinicians should be mindful of this side effect. Furthermore, when any antipsychotic is prescribed, clinicians should monitor their patients regularly with ECG to avoid adverse cardiac effects.
References
1. Brown DJ, Brugger H, Boyd J, Paal P. Accidental hypothermia. N Engl J Med. 2012; 360(20): 1930–1938.
2. van Marum RJ, Wegewijs MA, Loonen AJ, Beers E. Hypothermia following antipsychotic drug use. Eur J Clin Pharmacol. 2007;63(6):627–631.
3. Kowalczyk E, Kasprzak JD, Lipiec P. Giant J-wave and Brugada-like pattern in a patient with severe hypothermia. Acta Cardiol. 2014;69(1):66–67.
4. Wu CS, Tsai YT, Tsai HJ. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Assoc. 2015;4(2).
5. Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951–962.
6. Ray WA, Chung CP, Murray KT, et al. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360(3):225–235.
7. Drolet B, Yang T, Daleau P, et al. Risperidone prolongs cardiac repolarization by blocking the rapid component of the delayed rectifier potassium current. J Cardiovasc Pharmacol. 2003;41(6):934–937.
8. Vigneault P, Kaddar N, Bourgault S, et al. Prolongation of cardiac ventricular repolarization under paliperidone: how and how much? J Cardiovasc Pharmacol. 2011;57(6):690–695.
9. Kreuzer P, Landgrebe M, Wittmann M, et al. Hypothermia associated with antipsychotic drug use: a clinical case series and review of current literature. J Clin Pharmacol. 2012;52(7):1090–1097.
10. Bonnemeier H, Mäuser W, Schunkert H. Images in cardiovascular medicine. Brugada-like ECG pattern in severe hypothermia. Circulation. 2008;118(9):977–978.
11. McCullough L, Arora S. Diagnosis and treatment of hypothermia. Am Fam Physician. 2004;70(12):2325–2332.
12. Cunningham LM, Mattu A, O’Connor RE, Brady WJ. Cardiopulmonary resuscitation for cardiac arrest: the importance of uninterrupted chest compressions in cardiac arrest resuscitation. Am J Emerg Med. 2012;30(8):1630–1638.
13. Bradley SM. Update in cardiopulmonary resuscitation. Minerva Cardioangiol. 2011;59(3):239–253.





