by Gabriel Edwards, MD, MPH; Teryl Nuckols, MD, MSHS; Nathalie Herrera, MD; Itai Danovitch, MD, MBA; and Waguih William IsHak, MD, FAPA
by Gabriel Edwards, MD, MPH; Teryl Nuckols, MD, MSHS; Nathalie Herrera, MD; Itai Danovitch, MD, MBA; and Waguih William IsHak, MD, FAPA
Drs. Edwards, Herrera, Danovitch, and IsHak are with the Department of Psychiatry and Behavioral Neurosciences, Cedars-Sinai Medical Center in Los Angeles, California. Dr. Nuckols is with the Division of General Internal Medicine, Cedars-Sinai Medical Center in Los Angeles, California. Dr. IsHak is with the David Geffen School of Medicine at UCLA in Los Angeles, California.
Funding: No funding was provided.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Objective: This paper sought to review the impact of depression in patients with comorbid medical problems, the importance of bridging the gap between inpatient and outpatient care for medical inpatients with depression (especially for organizations that treat patients in both settings), and the elements necessary to implement a pilot for an outpatient Collaborative Care Management program for patients with depression following medical admissions. Taken into account is the presence of new billing mechanisms and potential cost offsets. Methods: The literature referenced in this paper was identified through a search of online databases, including PubMed and Google Scholar. The data used to analyze cost were drawn from national, publicly available sources, such as the Kaiser Family Foundation, Bureau of Labor Statistics, and the Organisation for Economic Cooperation and Development. Results: Collaborative care is an evidence-based intervention for depression that can aid with successful transition of care as patients move from the inpatient to the outpatient setting. It can be considered cost-effective when treating a panel of patients that falls below the recommended caseload for a single case manager (i.e., 19–46 billed encounters, depending on the payer mix), particularly when considering the savings from a reduced length of stay associated with well-controlled depressive symptoms. Conclusion: Organizations should consider implementing collaborative care management for patients with depression to improve depression outcomes, reduce costs, and prepare themselves for a health financing environment that rewards value.
Keywords: Depression, consult psychiatry, collaborative care, care transitions, care management, value-based purchasing, health care organization and financing, telemedicine, comorbid physical, mental illness
Innov Clin Neurosci. 2019;16(11–12):19–24
Depression affects millions of Americans every year, estimated at 8.1 percent of the population in any given two-week period.1 It is now recognized that depressive symptoms are implicated in the worsening of physical functioning, bodily pain, and general health perceptions.2–4 Depressive symptoms also have substantial economic consequences, with an estimated annual cost exceeding $80 billion.5 The purpose of this paper is to lay out the case that 1) depression has impacts on the patient health and cost of care, regardless of whether that care is delivered in the inpatient or outpatient setting; 2) that health outcomes suffer with poor care coordination as a patient transfers between settings; 3) the Collaborative Care Management Model (CoCM) is an evidence-based approach to treating depression in an outpatient setting that could be incorporated in care transition planning; and, finally, 4) that recent financing mechanisms have made implementing CoCM more cost-effective, particularly when considering organizations that take responsibility for patient care in both the inpatient and outpatient settings.
Included in this article is a cost-effectiveness analysis that considers the annual cost of staffing CoCM, as well as the annual revenue that could be generated both from billing for service and from resources saved by reductions in hospital stay among patients with well-controlled depressive symptoms compared to those whose symptoms remain untreated. The objective of this analysis is to demonstrate the minimum number of patients one would need to bill for to cover the staffing costs, taking into account the payer mix. This analysis is particularly applicable for organizations that treat a patient in both the hospital and clinic because they are positioned to capture both types of revenue listed above. This differs from much of the literature that has considered CoCM in the outpatient setting exclusively.
The Impact of Depressive Symptoms and Comorbid Medical Problems
The burden of medical illness on patients suffering from depression is substantial. It is estimated that up to 60 percent of patients with chronic medical illness also suffer from depressive symptoms, with a median prevalence rate of 33 percent among medical inpatients.6 Moreover, nearly 80 percent of patients experiencing depressive symptoms struggle with a comorbid physical illness.7
Depression is an active contributor to the severity of medical illness. Patients with depression are at an increased risk for diabetes, cardiovascular disease, hypertension, coronary artery disease, myocardial infarction, heart failure, and stroke.8–14 Large World Health Organization studies have shown that comorbid depressive symptoms, along with any chronic disease (e.g., angina, arthritis, asthma, diabetes), “incrementally worsen health” compared to depression or chronic disease alone.15
Depressive disorders are associated with significantly higher healthcare utilization and costs.16 Compared to individuals who do not have depression, those with depressive symptoms tend to have higher numbers of primary care visits, specialist referrals, and total costs of care, even after controlling for age and comorbidity.17,18 One systematic review and meta-analysis found that patients with depression stay in the hospital, on average, 4.38 days longer than patients without depression.19 High rates of readmission have been observed among patients with depressive disorders.20 Moderate-to-severe depressive symptoms are specifically associated with a doubled risk of 30- and 90-day readmissions (odds ratio: 2.00) compared to patients without depression.21
Depressive symptoms are underdetected and/or undertreated. Studies showed that 33 to 50 percent of individuals with depression do not seek treatment, with the majority waiting for 12 months or more before seeking care.22 Depressive symptoms often go undetected among hospitalized patients and tend to perpetuate comorbid physical and psychiatric symptoms.23 Studies show that 78 percent of medical inpatients who screen positive for depressive symptoms have not been diagnosed previously.24 The United States Preventive Services Task Force has stated that depression screening can increase response to treatment and the rate of remission of depressive symptoms and decrease morbidity.25 Therefore, an inpatient setting represents a critical point for detection and intervention for both depressive symptoms and comorbid physical illness, especially if coupled with an effective transition-of-care model, given the magnitude of the societal and patient burden that these conditions represent.26
The Importance of Bridging the Gap from Inpatient Care to Outpatient Care in Medical Inpatients Experiencing Depressive Symptoms
Depression follows patients as they leave the discharge and can interfere with aftercare, persisting in 40 percent of patients at 30 days postdischarge.27 When individuals with chronic medical conditions and depression leave the hospital, they are less likely to take their medications and attend medical/psychiatric appointments, resulting in more frequent emergency department (ED) visits, recurrent readmissions, lengthy hospital stays, and increased cost of care.28,29 Failure of care coordination is estimated to cost primary payors up to $45 billion annually while also diminishing the quality of posthospitalization care and leading to poorer patient outcomes.30 Rehospitalization for patients with poor linkages has been estimated to be preventable in 25 to 33 percent of cases.31
Transitional care focuses on bridging the gap to ensure continuity of care between the inpatient and outpatient departments, making this transition potentially successful from the standpoint of health outcomes, as well as cost. The effectiveness of transitional care was shown in three randomized, controlled trials funded by the National Institutes of Health.32–34 These trials showed that direct engagement of patients via patient education, case management, and care-continuity support, producing significant improvements in physical function, quality of life, and satisfaction with care compared to controls.34 Care coordination programs have demonstrated improved medication adherence, health status, quality of life, and cost savings.35 They do so despite concerns that the costs of care coordination might pose a challenge to the widespread implementation.36
The medical profession is increasingly taking steps to address this issue. The American College of Physicians, Society of Hospital Medicine, Society of General Internal Medicine, American Geriatric Society, American College of Emergency Physicians, and the Society for Academic Emergency Medicine have developed consensus standards to address the gaps in the transitions between inpatient and outpatient settings. Significant issues addressed include a lack of communication between hospital and primary care physicians adversely affecting postdischarge care transitions, influencing the quality of care in approximately 25 percent of follow-up visits.37 According to a systematic review and meta-analysis, effective care transition interventions hinge on comprehensiveness, extension beyond the hospital stay, and good flexibility in responding to patient needs.38
The Collaborative Care Model
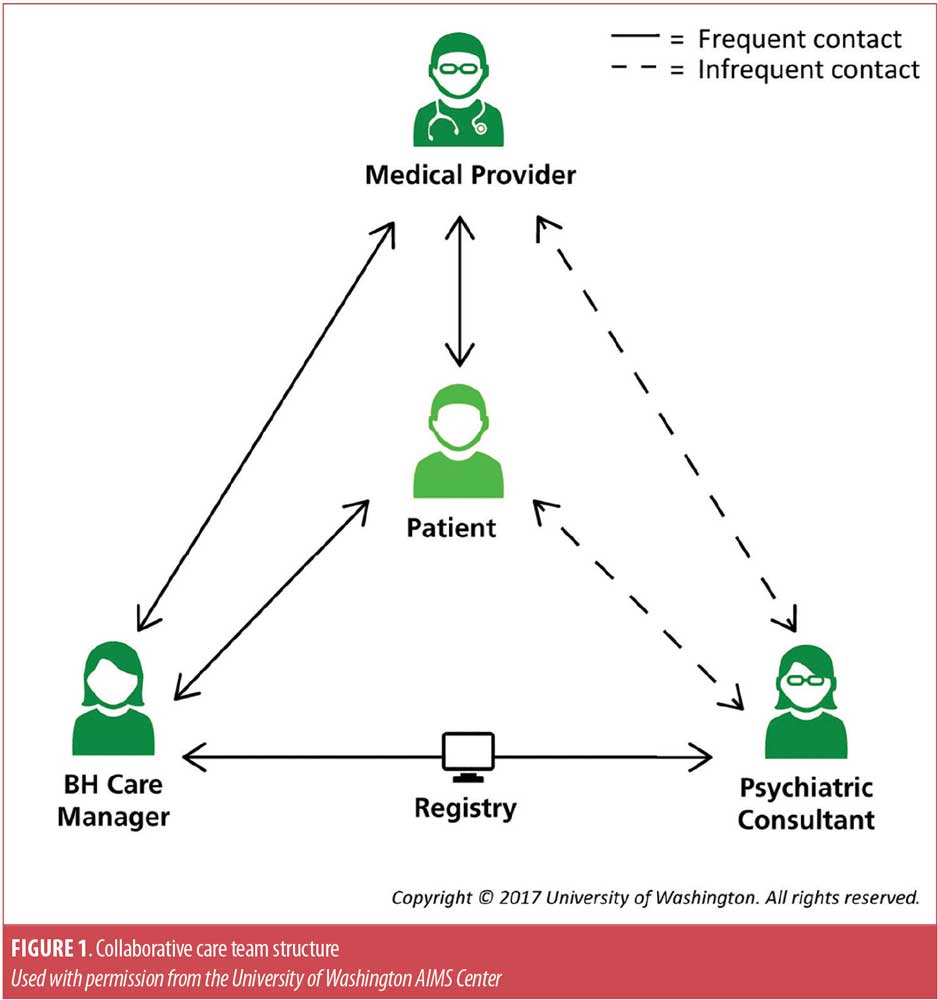
For the treatment of depression in the outpatient setting, there is a growing body of evidence that collaborative care is an effective approach. The CoCM, a specific model of care, refers to multiple health professionals working in concert with the patient to systematically identify and intervene to address mental health conditions. The model is based on the principles of chronic disease management used in managing conditions such as diabetes.39 Figure 1 diagrams the team structure and how the members relate to the patient. The care team includes the patient’s treating physician, a care manager with training in depression treatment, and a behavioral health specialist, such as a psychiatrist. A 2012 review of 79 randomized, controlled trials, comparing collaborative care with routine care for depression and anxiety, found that the patients receiving collaborative care demonstrated significantly greater improvement in depression outcomes in the short-, medium-, and long-term, with evidence of benefit in secondary outcomes, including medication use, mental health quality of life, and patient satisfaction.39 The Community Preventive Services Task Force recommends collaborative care for management of depressive disorders, based on strong evidence of effectiveness in improving depression symptoms, adherence to treatment, response to treatment, and remission and recovery from depression.40
In response to the above findings, the Center for Medicare & Medicaid Services (CMS) introduced new Current Procedural Terminology (CPT) codes that allow providers to seek reimbursement for CoCM starting January 1, 2018.41 The payments are bundled, with the patient’s primary treating clinician submitting the billing on behalf of the entire care team. The care manager and psychiatric consultant deliver components their required elements but do not bill separately; the activities of each member are aggregated together. For example the care manager is responsible for maintaining a registry of all patients they care for under this model, and the psychiatric consultant aids in determining or adjusting treatments for patients who are failing to respond or progress.
Financing Collaborative Care
The CPT codes adopted by the CMS on January 1, 2018, created a funding mechanism for this specific model of collaborative care. Following the lead of the CMS, private payers have begun to reimburse providers for these services as well.42
We approached the financing of this model as a break-even equation. For example, can the financial returns from the intervention cover or exceed the costs of hiring one full-time licensed clinical social worker, three hours per week of a psychiatric consultant, and nominal administrative support? These staffing numbers were drawn from guidelines put out by the developer of the CoCM.43 The care manager is responsible for the creation and maintenance of a registry of all patients receiving treatment, coordinating and supporting the delivery of mental health services, and coordinating team-based care.44 The psychiatric consultant provides caseload consultations to the care manager and occasional telephonic consultation to the treating physician, focusing on such issues as treatment plan changes and referrals.45
Personnel costs. The costs included the hiring of a full-time licensed clinical social worker (LCSW) to act as a care manager and paying a psychiatrist for three hours of their time weekly, on average, based on published estimated workloads for the intervention.44,45 The salary totals for each team member are taken from the national salary data.46,47 The care manager and psychiatric consultant support the primary care physician in their standard treatment of depression and, thus, the cost of staffing the latter is not considered in the analysis.
Table 1 shows the calculated personnel costs.

Billing revenue. To determine billing revenue, we calculated the revenue for services rendered by members of the collaborative care team. Second, using what we know about the effect of depression on hospital length of stays, we also factored in the savings from reduced hospital stays. The revenue from billing was generated by taking a weighted average of the relevant billing codes (99492, 99493, 99494, and 99484). Medicare data are publicly available.42 For the purposes of this analysis, we assumed private payers would compensate at twice the sum compared to Medicare. Here, 99492 is the code for the first 70 minutes spent with patients new to the intervention, 99493 is the code for the first 60 minutes in subsequent month, and 99494 is for patients whose length of service exceeds the time limits of either 99492 or 99493. Finally, 99484 is a behavioral health integration code that can be used for extra services outside the scope of CoCM, such as longer psychotherapy visits delivered by the Care Manager.41 The weights were a rough estimate for the distribution, with a 1:2:1 distribution for the 99492 to 99494 and two extra charges per month of 99484.
Possible hospital savings for reduced length of stay. Hospital savings were calculated using data on hospital utilization by age group to estimate the number of hospital visits corresponding to a set number of patients and then assuming that depression in remission reduces the hospital length of stay by 4.38 days per patient.19 National data were used to estimate the rate of hospitalization for three age groups (18–44, 45–64, and 65+ years), as well as the proportion each age group represents in an average inpatient population.48 The average length of hospital stay was set at 4.1 days.49
The average cost to a hospital of an inpatient day was taken as a national average from available data.50 The product of average inpatient stays per individual in each age bracket, the average cost of an inpatient day, and the differential length of stay between individuals with and without depression were taken to determine amount of savings expected from shortened length of stay. Table 2 shows the calculations.
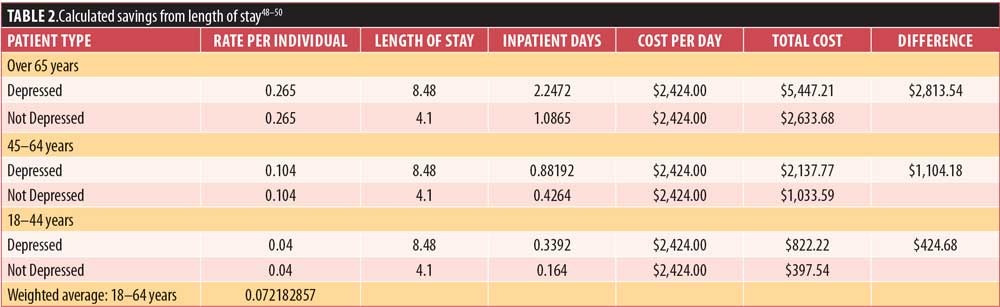
Also considered was the fact that the rates of depression remission using collaborative care are not 100 percent but, rather, closer to 30 percent using the data from the meta-analysis of collaborative care interventions.39 For this reason, the saved hospital revenue was reduced accordingly.
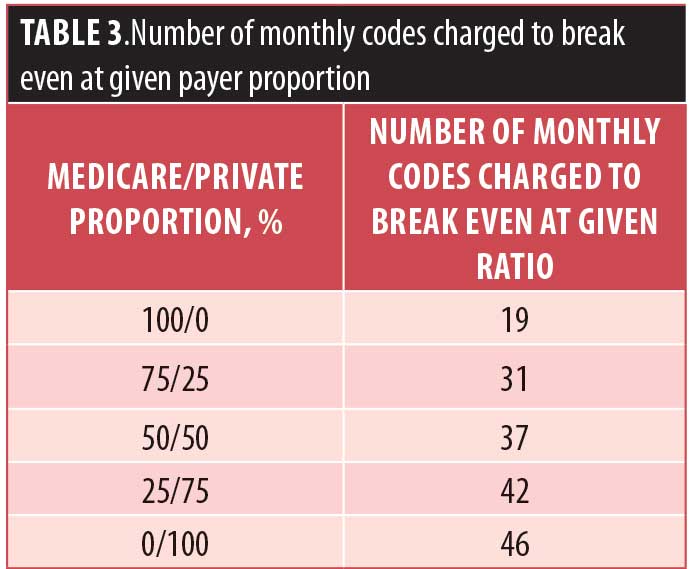
Taking the difference between overall revenue and cost, we were able to calculate how many encounters needed to be billed per month to meet or exceed the total cost from Table 1. We were also able to adjust the proportion of Medicare to private payer patients to run a sensitivity analysis. Table 3 shows a brief summary of results. Note that these are the minimums required for financial viability, not a reflection of the caseload capacity for a care manager.
In fact, a care manager can handle more than 46 patients in a given month. According to the Advancing Integrated Mental Health Solution Center, the caseload recommendations for a 1.0 full-time equivalent behavioral care manager range from 60 to 80 cases (for patients with limited social support, low income, and/or homeless status), or up to 90 to 150 cases among a patient population characterized as having adequate income and intact support networks.43
Discussion
The CoCM offers a framework for delivering evidence-based interventions, improving care coordination, and systematizing depression care for patients with comorbid medical issues in a way that is cost-effective. Our assessment suggests that, when taking into account indirect cost savings, the number of patients needing to receive services to break even is well below the estimated caseload of a single care manager.43 Despite estimating that private payers would reimburse at twice the rate as Medicare, the break-even caseload with 100 percent Medicare patients is lower due to the increased hospital care savings; the model takes into account older individuals’ higher rates of hospitalization.48 Savings from decreased hospital length of stays range from $23,757.60 for 100 percent private patients to $87,219.64 for 100 percent Medicare recipients, according to our model.
Furthermore, implementing value-based models, such as the CoCM, reflects a necessary shift in the culture of healthcare delivery for organizations that want to thrive in the future. Organizations that are accountable for the entire costs and care of a patient population are the ones who will reap the full financial benefits of the intervention outlined in our financial model, but even hospitals whose patients aren’t part of a managed care plan could benefit from the reduced length of hospital stays and utilization of services in a population with improved depression care.
For the foreseeable future, healthcare providers will face sustained pressure to demonstrate value-based outcomes. Value will play a key role in the way that healthcare will be evaluated and financed. In recent years, for example, the CMS launched its Hospital Value-based Purchasing (VBP) program for its Medicare beneficiaries, compensating hospitals on metrics such as quality, best-practice adherence, and patient experience.51 Among data elements to be measured are the utilization of screening tools including the Patient Health Questionnaire-9 and Depression Remission or Response for Adolescents and Adults.52 There is even evidence that VBP improves fidelity to key elements of CoCM, as well as depression outcomes.53
Implementing a well-defined care model might also increase the ability to measure quality within consultation-liaison psychiatry, a service that has been characterized as difficult to measure and for which there have been consistent calls for evidence to demonstrate effectiveness.54 An integrated health system with CoCM fully introduced could give consultation-liaison psychiatrists the opportunity to identify inpatients with depression and connect them to an intervention that could follow them after discharge as part of an effective care transition.
While this paper used national data to generalize the results, a clinically and financially successful model will require the careful selection of a patient population. Collaborative care is team-based and reimbursed as a bundle; an organization aiming to capture all the revenue must treat patients whose entire care team practices in-house. Therefore, patients in the pilot must have all their care team employed at the same institution to collect the full reimbursement (as opposed to cost sharing with outside entities). For this report, we focused on patients who either have Medicare or private insurance. This paper provides a framework for estimating the benefits of implementing the CoCM in the context of a health system that offers inpatient and outpatient services. We believe that the use of the model has potential to improve depression outcomes in a cost-effective manner.
Limitations For the purposes of creating the financial model, some simplifications had to be made. For example, everyone under 65 years of age in our model was assumed to be privately insured, with everyone aged 65 years or older assumed to be on Medicare. In reality, individuals under 65 years of age can receive Medicare. Also, for simplicity, Medicaid was not considered, though the number needed to bill to Medicare and private payers to break even falls well below a single care manager’s caseload capacity, creating enough leeway to bill Medicaid. Medicaid nationally reimburses at approximately 72 percent of the rate of Medicare.55 Since we used national data, the results in specific localities will vary when calculating reimbursements from Medicare. This was not meant to be an exhaustive implementation guide but rather an introduction to specific topics the authors deemed important based on empirical experience delivering behavioral care and a careful review of the literature.
Future Directions
The bundled nature of CoCM payments might be of help in addressing some of the current limitations in billing for telemedicine for most patients. Medicare limits reimbursement for telehealth to beneficiaries located in specific originating sites, for example, such as a rural Health Professional Shortage Area or a county outside a Metropolitan Statistical Area in a rural census tract.56 For CoCM, the care manager must be available to provide face-to-face services in person, but the provision of face-to-face services is not required, thus allowing the care manager to furnish telehealth services to Medicare patients who might otherwise not receive them.41 Within the scope of collaborative care, services delivered in any form under the model are compensated based on time rather than mode. To overcome barriers related to regional variations in access to mental health clinicians, it is important to be able to offer services remotely. Selecting the most appropriate platform for delivering telepsychiatry, in this case, comes down to user-friendliness, The Health Insurance Portability and Accountability Act of 1996 (HIPPA) compliance, service stability, ability to interact with EMR, and cost-effectiveness. The present literature on telepsychiatry focuses more on best practices regardless of platform.57 Similarly, the American Psychiatric Association published a “Telepsychiatry Toolkit,” which includes general guidelines, such as minimum transmission speeds, HIPAA compliance, and encryption standards.58 In the future, more in-depth analysis may be run to consider the impact of adding Medicaid patients to the payer mix, or to adjust the members of the care team (e.g., using a marriage and family therapist in place of an LCSW). As health systems implement interventions such as CoCM, further studies will be needed to gauge the strengths and challenges of implementation, as well as the financial impacts.
References
- United States Centers for Disease Control and Prevention. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. https://www.cdc.gov/nchs/products/databriefs/db303.htm. Accessed May 28, 2019.
- Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54(3):216–226.
- Saarijarvi S, Salminen JK, Toikka T, et al. Health-related quality of life among patients with major depression. Nord J Psychiatry. 2002;56(4):
261–264. - Berlim MT, McGirr A, Fleck MP. Can sociodemographic and clinical variables predict the quality of life of outpatients with major depression? Psychiatry Res. 2008;160(3):
364–371. - Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155–162.
- IsHak WW, Collison K, Danovitch I, et al. Screening for depression in hospitalized medical patients. J Hosp Med. 2017;12(2):118–125.
- Ramasubbu R, Taylor VH, Samaan Z, et al. The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and select comorbid medical conditions. Ann Clin Psychiatry. 2012;24(1):91–109.
- Knol MJ, Twisk JW, Beekman AT, et al. Depression as a risk factor for the onset of Type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49(5):837–845.
- Musselman DL, Tomer A, Manatunga AK, et al. Exaggerated platelet reactivity in major depression. Am J Psychiatry. 1996;153(10):
1313–1317. - Jonas BS, Franks P, Ingram DD. Are symptoms of anxiety and depression risk factors for hypertension? Longitudinal evidence from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Arch Fam Med. 1997;6(1):43–49.
- Surtees P, Wainwright N, Luben R, et al. Sense of Coherence and mortality in men and women in the EPIC-Norfolk United Kingdom Prospective Cohort Study. Am J Epidemiol. 2003;158(12):1202–1209.
- Van der Kooy K, van Hout H, Marwijk H, et al. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry. 2007;22(7):613–626.
- Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527–1537.
- Jonas BS, Mussolino ME. Symptoms of depression as a prospective risk factor for stroke. Psychosom Med. 2000;62(4):463–471.
- Moussavi S, Chatterji S, Verdes E, Tandon A,et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858.
- Bock JO, Luppa M, Brettschneider C, et al. Impact of depression on health care utilization and costs among multimorbid patients—from the MultiCare Cohort Study. PLoS One. 2014;9(3):e91973.
- Ford DE, Erlinger TP. Depression and C-reactive protein in US adults: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2004;164(9):1010–1014.
- Marciniak M, Lage MJ, Landbloom RP, et al. Medical and productivity costs of anxiety disorders: case control study. Depress Anxiety. 2004;19(2):112–120.
- Jansen L, van Schijndel M, van Waarde J, van Busschbach J. Health-economic outcomes in hospital patients with medical-psychiatric comorbidity: a systematic review and meta-analysis. PLoS One. 2018;13(3):e0194029.
- Citrome L, Jain R, Tung A, et al. Prevalence, treatment patterns, and stay characteristics associated with hospitalizations for major depressive disorder. J Affect Disord. 2019;249:378–384.
- Cancino RS, Culpepper L, Sadikova E, et al. Dose-response relationship between depressive symptoms and hospital readmission. J Hosp Med. 2014;9(6):358–64.
- Kessler RC, Akiskal HS, Ames M, et al. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am J Psychiatry. 2006;163(9):1561–1568.
- von Ammon Cavanough S. Depression in the hospitalized inpatient with various medical illnesses. Psychother Psychosom. 1986;45(2):
97–104. - Helvik AS, Skancke RH, Selbaek G. Screening for depression in elderly medical inpatients from rural area of Norway: prevalence and associated factors. Int J Geriatr Psychiatry. 2010;25(2):
150–159. - Siu AL. Screening for depression in adults: US preventive services task force recommendation statement. JAMA. 2016;315(4):380–387.
- Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323.
- Pederson JL, Warkentin LM, Majumdar SR, McAlister FA. Depressive symptoms are associated with higher rates of readmission or mortality after medical hospitalization: a systematic review and meta-analysis. J Hosp Med. 2016;11(5):373–380.
- Dennis M, Kadri A, Coffey J. Depression in older people in the general hospital: a systematic review of screening instruments. Age Ageing. 2012;41(2):148–154.
- Albrecht JS, Gruber-Baldini AL, Hirshon JM, et al. Depressive symptoms and hospital readmission in older adults. J Am Geriatr Soc. 2014;62(3):
495–499. - Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516.
- Naylor M, Brooten D, Jones R, et al. Comprehensive discharge planning for the hospitalized elderly. Ann Intern Med. 1994;12(20):999–1006.
- Naylor M, Brooten D, Jones R, et al. Comprehensive discharge planning for the hospitalized elderly—a randomized clinical trial. Ann Intern Med. 1994;120(12):999–1006.
- Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281(7):613–620.
- Naylor MD, Brooten DA, Campbell RL, et al. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–684.
- Naylor MD, Kurtzman ET, Pauly MV. Transitions of elders between long-term care and hospitals. Policy Polit Nurs Pract. 2009;10(3):187–194.
- Naylor MD, Bowles KH, McCauley KM, et al. High-value transitional care: translation of research into practice. J Eval Clin Pract. 2013;19(5):
727–733. - Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College Of Emergency Physicians, and Society for Academic Emergency Medicine. J Gen Intern Med. 2009;24(8):971–976.
- Kansagara D, Chiovaro J, Kagen D, et al. Care transitions from hospital to home. J Hosp Med. 2016;11(3):221–230.
- Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525
- Community Preventive Services Task Force. Recommendation from the community preventive services task force for use of collaborative care for the management of depressive disorders. Am J Prev Med. 2012;42(5):521–524.
- United States Centers for Disease Control and Prevention. Frequently Asked Questions about Billing Medicare for Behavioral Health Integration (BHI) Services. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/Behavioral-Health-Integration-FAQs.pdf. Accessed May 29, 2019.
- United States Centers for Disease Control and Prevention. Physician Fee Schedule. https://www.cms.gov/apps/physician-fee-schedule/. Accessed May 29, 2019.
- Advancing Integrated Mental Health Solutions Center. Guidelines on Caseload Size for Behavioral Health Care Managers and Psychiatric Consultants. https://aims.uw.edu/sites/default/files/CareManager_CaseloadSize_Guidelines.pdf. Accessed May 29, 2019.
- Advancing Integrated Mental Health Solutions Center. CoCM Behavioral Health Care Manager: Sample Job Description, Typical Workload & Resource Requirements. https://aims.uw.edu/sites/default/files/CareManagerJobDescription_0.pdf. Accessed May 29, 2019.
- Advancing Integrated Mental Health Solutions Center. Psychiatric Consultant: Sample Job Description, Typical Workload & Resource Requirements. https://aims.uw.edu/sites/default/files/PsychiatricConsultantJobDescription_0_0.pdf . Accessed May 29, 2019.
- United States Department of Labor. Social Workers. https://www.bls.gov/ooh/community-and-social-service/social-workers.htm#tab-5. Accessed May 28, 2019.
- United States Department of Labor. Psychiatrists. https://www.bls.gov/oes/2017/may/oes291066.htm. Accessed May 28, 2019.
- Healthcare Cost and Utilization Project. Trends in hospital inpatient stays by age and payer, 2000–2015. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb235-Inpatient-Stays-Age-Payer-Trends.jsp. Accessed May 29, 2019.
- Organisation for Economic Cooperation and Development. Length of hospital stay (indicator). https://data.oecd.org/healthcare/length-of-hospital-stay.htm. Accessed May 28, 2019.
- Kaiser Family Foundation. Hospital adjusted expenses per inpatient day. https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed May 28, 2019.
- United States Centers for Disease Control and Prevention. Hospital value-based purchasing. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/Hospital_VBPurchasing_Fact_Sheet_ICN907664.pdf. Accessed May 28, 2019.
- National Committee for Quality Assurance. Healthcare effectiveness data and information set: summary table of measures, product lines and changes. https://www.ncqa.org/wp-content/uploads/2018/07/20170701_HEDIS_2017-Measures.pdf. Accessed May 28, 2019.
- Bao Y, McGuire T, Chan Y, et al. Value-based payment in implementing evidence-based care: the Mental Health Integration Program in Washington State. Am J Manag Care. 2017;23(1):48–53.
- Wood R, Wand AP. The effectiveness of consultation-liaison psychiatry in the general hospital setting: a systematic review. J Psychosom Res. 2014;76(3):175–192.
- Kaiser Family Foundation. Medicaid-to-Medicare fee index. https://www.kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed May 28, 2019.
- United States Centers for Disease Control and Prevention. Telehealth services. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/TelehealthSrvcsfctsht.pdf. Accessed May 28, 2019.
- Recupero P, Fisher C. Resource document on telepsychiatry and related technologies in clinical psychiatry. https://www.psychiatry.org/File%20Library/Psychiatrists/Directories/Library-and-Archive/resource_documents/Resource-2014-Telepsychiatry-Clinical-Psychiatry.pdf. Accessed May 28, 2019.
- American Psychiatric Association. Telepsychiatry Toolkit. https://www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit. Accessed May 28, 2019.